The Project Gutenberg EBook of Dietetics for Nurses, by Fairfax T. Proudfit This eBook is for the use of anyone anywhere at no cost and with almost no restrictions whatsoever. You may copy it, give it away or re-use it under the terms of the Project Gutenberg License included with this eBook or online at www.gutenberg.org Title: Dietetics for Nurses Author: Fairfax T. Proudfit Release Date: August 8, 2010 [EBook #33379] Language: English Character set encoding: ISO-8859-1 *** START OF THIS PROJECT GUTENBERG EBOOK DIETETICS FOR NURSES *** Produced by Kevin Handy, John Hagerson, Sam W. and the Online Distributed Proofreading Team at http://www.pgdp.net
Transcriber's Note
Key letters in table header rows have a faint grey dotted underline. Hover your mouse over them to see the column labels.
This text contains some uncommon characters (⅓, ⅔, ⅙, ⅛, ⅜ and ⅞). If they do not display properly, you may need to adjust your browser settings.
THE MACMILLAN COMPANY
NEW YORK · BOSTON · CHICAGO · DALLAS
ATLANTA · SAN FRANCISCO
MACMILLAN & CO., Limited
LONDON · BOMBAY · CALCUTTA
MELBOURNE
THE MACMILLAN CO. OF CANADA, Ltd.
TORONTO
BY
FAIRFAX T. PROUDFIT
INSTRUCTOR AND CLINICAL DIETITIAN, MEMPHIS GENERAL
HOSPITAL, AND ST. JOSEPH’S HOSPITAL, CONSULTING
DIETITIAN, MEMPHIS ASSOCIATED CHARITIES, AND
PUBLIC HEALTH NURSING ASSOCIATION,
MEMPHIS, TENNESSEE
SECOND EDITION
Completely Revised
NEW YORK
THE MACMILLAN COMPANY
1923
All rights reserved
PRINTED IN THE UNITED STATES OF AMERICA
Copyright, 1918 and 1922,
By THE MACMILLAN COMPANY.
———
Set up and electrotyped. Published November, 1918
Second Edition completely revised and reset
Published, July, 1922
Press of
J. J. Little & Ives Company
New York, U. S. A.
Dedicated
to the
Great Army of Nurses
in the Service
The old order of things is passing. The keynote of to-day’s work is prevention, rather than cure, children are taught to eat correctly that they may grow into the strong, healthy men and women which are needed to make any nation great. This instilling of good health habits must rest upon the nurse, the nutrition worker, the physician and the home-maker. Close coöperation is necessary among these workers and a definite understanding of the way to accomplish the best results, in this respect, must come from the training of those who are undertaking this all important work.
The present revision of this text is the outgrowth of several years of close attention to the progress, changes and adjustments which are being made daily in this important subject of nutrition. The changes made in this revised edition are all in the line of constructive teaching. The material has been reorganized that no time may be lost in a search for the proper word to illustrate a definite point. The method of project teaching used in this edition, is not a new one, although the name may possibly be unfamiliar to some. Every good teacher recognizes the value of motivation as a means of getting an idea “across.” The revision of this text was undertaken with the idea of leading the student to think for herself and to put into practice the scientific facts learned in class room and ward.
The author is indebted to many of her colleagues for the encouragement and constructive criticism which enabled her to make the changes which will, it is hoped and believed, materially aid the student nurse in the study of [Pg viii] Dietetics. She also wishes to express her appreciation for the many helpful suggestions made by her co-workers in this respect, especially to Misses L. H. Gillett and L. Willson for valuable criticism and to Miss H. Buquo for assistance in the preparation of the manuscript.
F. T. P.
No other science has so much to do with the general welfare of mankind as the study of food and its effects in the human body. When we use the term “dietetics” as representing “the effect of the food in the human body,” we do so in a very broad sense, for the subject is a big one, requiring comprehensive terms to express it.
The problems of nutrition are many. Food alone is no small subject and a still greater one is the utilization of food materials in such a way that the body may gain the greatest value with the least expenditure of vital forces. These problems are discussed in this text and the methods of overcoming them are given in the simplest possible language. For this purpose the subject of nutrition has been divided into groups: (1) a comprehensive study of the sources of food, its composition and nutritive value; (2) the effect of food in the body under normal conditions, as in health; and (3) its behavior and effect when conditions in the body become abnormal, as in disease. In this way much of the non-essential material is eliminated from the course of study and only that included which it is necessary for the nurse to understand and which she will constantly use both in the hospital and later on in the practice of her profession. The simple methods of study presented in this text are given with the idea of avoiding confusion in the mind of the average pupil nurse by fitting in the course with her other studies rather than by making it stand out as a separate subject. In this way she will be able to see at a glance the connection between the body processes and the materials which are used to carry them on. Thus her study of physiology, anatomy and bacteriology go hand in hand with that of dietetics, each bearing a distinct relationship to the others.
| SECTION I | ||
| FOOD AND ITS SIGNIFICANCE | ||
| CHAPTER | PAGE | |
| I | Food | 1 |
| II | Fuel Value of Food | 36 |
| III | Food Requirements of the Body | 42 |
| SECTION II | ||
| LABORATORY OR DIET KITCHEN WORK | ||
| IV | Methods of Feeding in Normal and Abnormal Conditions | 59 |
| V | Food Materials and Their Preparation | 81 |
| VI | Infant Foods and Formulas Used in Abnormal Conditions | 140 |
| SECTION III | ||
| THE HUMAN MACHINE | ||
| VII | The Human Body | 165 |
| SECTION IV | ||
| DIETO-THERAPY | ||
| VIII | Pregnancy and Lactation | 191 |
| IX | Infant Feeding | 199 |
| X | Care and Feeding of Children in Normal and Abnormal Conditions and in Infectious Diseases | 231 |
| XI | Feeding of Adults in Diseases of the Gastro-intestinal Tract | 245 |
| XII | Diseases of the Intestinal Tract | 263 |
| XIII | Fevers in General | 281 |
| XIV | Typhoid Fever | 288 |
| XV | Diseases of the Respiratory Tract | 301 |
| XVI | Dietetic Treatment Before and After Operation | 312 |
| XVII[Pg xii] | Urinalysis | 323 |
| XVIII | Acute and Chronic Nephritis | 336 |
| XIX | Diseases of the Heart | 365 |
| XX | Diabetes Mellitus | 372 |
| XXI | Diseases of the Liver | 404 |
| XXII | Gout, Obesity and Emaciation | 418 |
| XXIII | Other Conditions Affected by Diet | 451 |
| Table I. Edible Organic Nutrients and Fuel Values of Foods | 461 | |
| Table II. Ash Constituents of Foods in Percentage of the Edible Portion | 472 | |
| Table III. Showing 100-Calorie Portions of some Common Foods, Together with Their Protein, Nitrogen, and Mineral Content | 478 | |
| Table IV. Composition and Fuel Value of most of the Foods used in the Invalid Dietary | 484 | |
| Table V. Vitamines in Foods | 496 | |
| Heights and Weights for Children under Five Years of Age | 499 | |
| Height and Weight Table for Boys | 500 | |
| Height and Weight Table for Girls | 501 | |
| Pelidisi Chart | 502 | |
| The Nutritional Index—The “Pelidisi” | 503 | |
| Index | 505 |
Preliminary Course of Lectures and Laboratory Work
The value of a knowledge of food and its effect in the human body cannot be overestimated. In health, this knowledge leads to higher standards, since by pointing out the errors in one’s mode of living, good health habits may be established, which will, undoubtedly assure the individual of a better nourished and a more vigorous body.
There is no question as to the value of health either from the standpoint of comfort or of economy. And the knowledge which will enable one to spread the good work intelligently cannot but raise the standards of living throughout the entire community.
In taking up the study of dietetics, the student is introduced to some of the fundamental principles governing the health and well-being of a people, since dietetics includes a study of food and its relation to the body.
The relationship between right food and good health is very close; how close is being demonstrated constantly in experimental fields of scientific research.
To be able to judge whether the food one eats daily is giving the best possible value from a physiological and economic standpoint, requires a definite knowledge of food, its source, composition and nutrient value, as well as its relation to the body in health and disease.
No one is capable of giving constructive advice upon matters pertaining to diet, unless he has acquired this knowledge through training. A nurse should obtain this training during her course in the hospital, through the class room, the wards and the diet kitchen.
[Pg 2] The dividing line between health and disease is frequently almost imperceptible, and without a knowledge of the normal body, it is, at times, impossible to tell where the normal leaves off and the abnormal begins. For this reason a nurse must understand normal nutrition, that is, the behavior of food in the healthy body, before undertaking the task of ministering to the body attacked by disease.
In a text of this kind, it is impossible to cover all phases of the subject, especially since day by day new discoveries are being made with relation to food and its uses in the body. But with careful attention to the principles set forth, a nurse should be able to carry out the dietary orders given her by the physician and dietitian in the hospital. And, when her course of training is finished, she should find herself equipped to assist in raising the standard of health through her knowledge of dietetics. With this brief summary of the aims and object of the study of dietetics, we will begin the actual work with a study of Food.
Food Materials.—Food is the name given to any substance which, taken into the body, is capable of performing one or more of the following functions:
1. Building and repairing tissue, maintenance, growth, and development of the muscles, bones, nerves, and the blood.
2. Furnishing the energy for the internal and external work of the body.
3. Regulating the body processes, maintaining the proper alkalinity and acidity of the various fluids throughout the body, regulating the proper degree of temperature, and determining the osmotic pressure, etc.
For the convenience of study scientists have arranged the foodstuffs in groups:
[Pg 3] 1. According to type;
2. According to their chemical composition;
3. According to the function they perform in the body.
All foods are composed of certain chemical elements; namely, carbon, oxygen, hydrogen, nitrogen, sulphur, phosphorus, iron, magnesium, potassium, chlorine, sodium, calcium, with traces of various others. The manner in which these elements are combined and the amounts in which they occur determine the group to which the combination belongs, and give to the foodstuff its characteristic position in human nutrition.
The chemical elements are combined in food and in the body, as: (a) carbohydrates, composed of carbon, oxygen and hydrogen; (b) fats, composed of carbon, oxygen and hydrogen; (c) proteins, composed of carbon, oxygen, hydrogen, nitrogen and sulphur; (d) water, composed of hydrogen and oxygen; (e) mineral salts. The first three foodstuffs constitute the Organic Food group. The last two include the remaining chemical elements, calcium, phosphorus, sodium, potassium, chlorine, magnesium, iron and traces of others which make up the Inorganic Food group.
Each of the foodstuffs belonging to the organic group is capable of being burned in the body to produce heat for: (a) the maintenance of the body temperature; (b) internal and external work.
Neither water nor mineral salts alone can be burned to produce heat; nevertheless, they enter into the composition and take part in every function performed by the carbohydrates, fats and proteins; therefore one foodstuff cannot be said to be of greater importance than another, since the needs of nature are best met by a judicious combination of all. However, the wear and tear of life can be more [Pg 4] efficiently accounted for, and the strain upon the organism reduced more nearly to a minimum when the various foodstuffs are furnished in amounts which science is proving to be necessary for the health and well-being of the organism.
The sixth essential food substance, the Vitamines, together with the adjustment of the five foodstuffs just mentioned—the amounts and types of each in the dietary which will assure the body of the best results—has been, and still is a subject of grave interest. Even on the most perfect adjustment of these foodstuffs, the diet would fail to give the desired results without the inclusion of the sixth, or vitamine factor, which has proved to be essential for the growth and development of the normal body, as well as for its protection against certain deficiency diseases.
In order to obtain the best results from food, both from a health and an economic standpoint, it is necessary to become familiar with the foodstuffs as they are combined to make up the various common food materials. One foodstuff may be a producer of heat, but may lack certain chemical elements which are essential to the building of tissues; another may be able to accomplish both functions in the body, but will prove too expensive to use as fuel, except when it is absolutely necessary to do so. Thus, it is essential for the nurse to understand where and how both the foodstuffs and the vitamines occur in nature, in order to make use of them more advantageously. The following table gives the sources of the foodstuffs, after which a description of the individual foodstuffs and vitamine factors will serve to point the way to their use in the dietary:
| Milk, cheese (especially skim milk cheese). | ||||
| Eggs. | ||||
| Meat (lean meat in particular). | ||||
| Poultry, game. | ||||
| Fish. | ||||
| Proteins | Cereals, corn, wheat, rye, oats, etc. | |||
| Bread and breadstuffs (crackers, pastry, macaroni, cake). | ||||
| [Pg 5] | Beans, peas, lentils. | |||
| Cotton seed. | ||||
| Nuts. | ||||
| Gelatin. | ||||
| Wheat products (bread, cake, crackers, pastry, macaroni, spaghetti). | ||||
| Cereal grains, breakfast foods. | ||||
| Corn products, corn meal, green corn. | ||||
| Rice, sago, tapioca, taro. | ||||
| Potatoes (white and sweet). | ||||
| Carbohydrates | Starchy fruits (bananas). | |||
| Sweet fruits (oranges, grapes, pineapples). | ||||
| Dried fruits (prunes, dates, raisins, currants). | ||||
| Sugar cane, sorghum cane. | ||||
| Sugar beets, sugar maples. | ||||
| Products made from sugar (candy, jellies, preserves, marmalade). | ||||
| Butter, cream, cheese. | ||||
| Olive oil, cotton seed oil, peanut oil, corn oil, almond oil. | ||||
| Soy bean. | ||||
| Corn meal, cotton seed meal and flour, oatmeal. | ||||
| Fats | Pork (bacon especially), other fat meat. | |||
| Codfish (and other fatty fish). | ||||
| Eggs (yolk). | ||||
| Cocoa, chocolate. | ||||
| Brazil nuts, almonds, pecans, and other nuts rich in fat. | ||||
| Water | All foodstuffs except those which have been put through a drying process. | |||
| Mineral salts (organic form) | Nitrogen (in proteins, meat, eggs, milk, fish, gluten of wheat, zein of corn meal, legumen of beans, peas, and lentils). | |||
| Phosphorus (eggs, yolk especially, cream, vegetables, whole wheat, cereals, breadstuffs, oatmeal, dried beans and peas). | ||||
| Iron (organic and inorganic form) | Eggs, milk, lean meat, cereal products, whole wheat,dried beans and peas, vegetables, spinach in particular, onions, mushrooms, fruits, port wine. | |||
| [Pg 6] | Milk.[1] | |||
| Eggs. | ||||
| Calcium (organic and inorganic form) | Soft tissues and fluids of all animals, skeleton and teeth of animals. | |||
| Wheat (the entire grain), flour, oatmeal, polished rice. | ||||
| Dried beans and peas. | ||||
| Green vegetables (beets, carrots, parsnips, turnips, potatoes). | ||||
| Fruits (apples, bananas, oranges, pineapples, dried prunes). | ||||
| Nuts (almonds, peanuts, walnuts). | ||||
| Lean beef, eggs, milk. | ||||
| Sulphur (organic and inorganic form) | Wheat flour, entire wheat, crackers, etc. | |||
| The proteins | Oatmeal. | |||
| Beans, peas. | ||||
| Potatoes. | ||||
| Sodium, potassium, magnesium, iodine, chlorine | These elements are associated with the other mineral salts in foods, and a diet in which they are adequately supplied furnishes sufficient magnesium, potassium, chlorine, sodium, and iodine for the general needs of the body. | |||
| Fat soluble “A.” | ||||
| Butter, cream, whole-milk. | ||||
| Whole-milk powder. | ||||
| Whole-milk cheese. | ||||
| Cod liver oil, eggs. | ||||
| Brains, kidney. | ||||
| Cabbage (fresh-dried). | ||||
| Carrots, chard, lettuce. | ||||
| Spinach, sweet potatoes. | ||||
| Water soluble “B.” | ||||
| Yeast (brewers’). | ||||
| Yeast cakes, yeast extract. | ||||
| Whole-milk, whey. | ||||
| Milk powder (whole and skimmed). | ||||
| Vitamines[2] | Nuts, cereals (corn embryo, wheat embryo, wheat-kernel, rice (unpolished)). | |||
| Beans (kidney, navy, soy). | ||||
| Cotton seed, peanuts, bread. | ||||
| [Pg 7] | Cabbage, carrots, celery. | |||
| Cauliflower, onions. | ||||
| Parsnips, potatoes. | ||||
| Peas (fresh), spinach. | ||||
| Rutabaga, fruit, grapefruit. | ||||
| Orange, lemon, tomato, raisins. | ||||
| Water soluble “C.” | ||||
| Fruits: Orange, lemon, tomatoes (canned). | ||||
| Tomato (fresh), grapefruit, limes, apples. | ||||
| Vegetables: Spinach, lettuce, cabbage (raw). | ||||
| Peas (fresh), onions, carrots, cauliflower. | ||||
| Potatoes (to a less extent). | ||||
| Whole-milk (to a less extent). | ||||
A study of the individual foodstuffs and vitamines will furnish the first link in the chain which constitutes our present knowledge of dietetics.
In the ordinary mixed diet of man, the carbohydrates predominate, being not only the most abundant, but also the most economical source of energy. The term carbohydrate covers all of the simple sugars and those substances which can be converted into simple sugars by hydrolysis; the ones of special interest in this study are divided into three groups, known as, Monosaccharides (C6H12O6); Disaccharides (C12H22O11) and Polysaccharides (C6H10O15).
Monosaccharides.—Glucose, Fructose and Galactose are substances whose monosaccharide molecules contain one sugar radical; hence they cannot be hydrolized to simpler sugars (sugars of lower molecular weight). Those constituting this group of sugars are all soluble, crystallizable and diffusible substances, which do not undergo changes from the action of the digestive enzymes, consequently these sugars will enter the blood stream in their original form, unless attacked by the bacteria which inhabit the stomach [Pg 8] and intestinal tract. The monosaccharides are all susceptible to alcoholic fermentation. Each member of the group is utilized in the body for the production of glycogen and for the maintenance of the normal glucose of the blood.
Disaccharides.—Sucrose, Maltose and Lactose are substances yielding, upon hydrolysis, two molecules of simple sugar: each of these sugars is crystallizable and diffusible: all are soluble in water, and to a less degree in alcohol—sucrose and maltose are more soluble than lactose. When attacked by the digestive enzymes, these sugars are changed to monosaccharides.
Polysaccharides.—Starch, Dextrin, Glycogen and Cellulose are substances more complex in character than the above-mentioned groups. They are built up of many sugar molecules, which yield upon complete hydrolysis many molecules of simple sugar. The polysaccharides are insoluble in alcohol, and only soluble to a certain extent in pure water. Some members of this group swell and become gelatinous in the presence of moisture and heat; some become of a colloidal form in water, and will pass through filter paper; others remain unchanged.
A brief description of the various members of these different groups of carbohydrates will assist the nurse in the ways and means of utilizing them in the dietary to the best advantage.
Glucose, which is abundant in the juice of plants and fruits, and to a more or less degree in the blood of all animals (usually about 0.1%) occurs free in nature. This sugar is likewise obtained from many carbohydrates, either through the action of acids, or as the result of the digestive enzymes, and as such becomes the principal form in which the animal body utilizes the carbohydrates ingested. Under normal conditions the glucose in the blood is constantly being burned and replaced; it is only when the body loses to a greater or less degree the ability to burn the glucose that [Pg 9] it accumulates in the blood, from which it must escape by way of the urine. There are times, such as when very large quantities of carbohydrates are eaten at once, when glucose will also appear in the urine; but under such circumstances it is generally found to be merely temporary, and for this reason, the condition is known as temporary glycosuria. As a rule, however, the surplus of glucose absorbed, whether it be eaten as such, or is found as the result of enzymic action upon the other carbohydrates, is converted into glycogen and stored in the liver and to a less extent in the muscles. Glycogen is readily reconverted into glucose, which is used by the body for the production of energy. It has been estimated that over half the energy manifested in the human body is derived from glucose, and it is in this form that the tissues of the body will ultimately make use of most of the carbohydrates in food. Practically all of the fruits, and many of the vegetables, are rich in this form of carbohydrate, but grapes contain more than any of the other fruits, while sweet corn, onions, and unripe potatoes contain appreciable amounts.
Fructose.—The second member of the monosaccharide group is more or less associated with glucose in plant and fruit juices, and is used like that substance for the production of glycogen in the body. Eaten as such, or produced as the result of digestive action upon cane sugar, fructose is changed into glycogen, chiefly upon entering the liver, and for this reason will not be found to enter largely into the blood of the general circulation.[3]
Honey is the most abundant source of fructose in nature.
Galactose.—This sugar, unlike the other members of this group, is not found free in nature, but it is produced as the result of hydrolysis of milk sugar, either by enzymes or by acids. Like glucose and fructose, galactose seems to promote the production of glycogen in the body. [Pg 10] Certain substances known as galactosides, which are combinations of galactose and some substances other than carbohydrates, are found in the nerve and brain tissues of the animal body.
Disaccharides.—Of the second group of carbohydrates, we are probably more familiar with sucrose, or cane sugar, than with either of the other two, since it is in this form that the greater part of the sugar eaten is purchased.
Sucrose.—By far the greater part of the sugar entering into the average dietary is manufactured from sugar and sorghum canes, and from sugar beets; but appreciable quantities are derived from the sugar maple and sugar palms. Many of the sweet fruits are rich in this form of sugar; pineapples are said to contain at least half of their solids in sucrose; and although other fruits and vegetables do not contain so high a percentage of this sugar, oranges, peaches, apricots, dates, raisins, prunes, carrots and sweet potatoes contain goodly quantities, which are associated with glucose and fructose. Sucrose is readily hydrolized, either by acids or enzymes. The inverting enzyme (invertase) of yeast and sucrase of the intestinal juice, convert sucrose to fructose and glucose, in which forms it is absorbed into the portal blood. It is believed that when sucrose is eaten in very large quantities, it is sometimes absorbed from the stomach. In these cases it does not become available for use in the body, but acts in the same manner as when injected directly into the blood stream, being excreted unchanged by way of the kidneys. According to Herter, sucrose is much more susceptible to fermentation in the stomach than either maltose or lactose; and since it has no advantage over these sugars from a standpoint of nutrition, they are frequently substituted for sucrose in cases where the dangers arising from fermentation must be avoided.
Maltose (Malt sugar) is an important constituent of germinating grains—malt and malt products being [Pg 11] formed as the result of enzymic action (amylases) on starch. A similar action takes place in the mouth as the result of the ptyalin in the salivary juices and in the intestines from the action of the starch-splitting enzyme, amylopsin, in the pancreatic juice. The maltose thus formed is further converted into glucose by the sugar-splitting enzyme in the intestinal juice, and in this form it is chiefly absorbed. Maltose is also an intermediate product formed during the manufacture of commercial glucose as the result of the boiling of starch with dilute acids.
Lactose (sugar of milk) is one of the most important constituents in the milk of all mammals. In freshly secreted human milk, lactose occurs in quantities ranging from 6 to 7%, and in the milk of cows and goats from 4 to 5%. Lactose is much less soluble than sucrose, and decidedly less sweet; hence, owing to this latter property, as well as to its lack of susceptibility to fermentation, lactose is frequently used to bring up the sugar content of infant formulas to the desired percentage, and the diets used in the abnormal conditions when additional energy material is needed. During the process of digestion, lactose is hydrolized by the lactase in the intestinal juice, yielding one molecule of glucose and one of galactose. Like maltose, little if any of this sugar is absorbed in its original form, since experiments made with injections of lactose into the blood result in the rapid and almost complete elimination by way of the kidneys. No such results are obtained when even large amounts of lactose are taken by way of the mouth.
Polysaccharides.—This group of carbohydrates is complex in character, built up of many sugar molecules, and upon digestion must be broken down into simple sugars before they can be utilized by the body.
Starch is the form in which the plant stores her supply of carbohydrates. It is found in this form in roots and [Pg 12] (mature) tubers, three-fourths of the bulk of which is made up of this material. From one-half to three-quarters of the solids of grains is made up of starch also. Pure starch is a fine white powder, odorless and almost tasteless. It is insoluble in cold water and alcohol, but changes from an insoluble substance to a more soluble one upon the application of heat. Upon hydrolysis starch gives first a mixture of dextrin and maltose, then glucose alone as an end-product. This hydrolysis may be the result of enzymic action, as occurs upon bringing starch in contact with the ptyalin in the saliva, or with the amylopsin in the pancreatic juice; or it may be the result of boiling starch with acid, as is seen in the manufacture of commercial glucose.
Dextrin, as has already been stated, is an intermediate product of the hydrolysis of starch by acid or enzymes.
Glycogen is the form in which the carbohydrates are stored in the body, just as starch is the form in which they are stored in plants. It is found in all parts of the body, but is especially abundant in the liver. Here it is stored in the cell substance rather than in the nucleus. The storage of glycogen in the human body depends largely upon the mode of life and upon the diet. Active muscular work, especially out of doors, uses up the store of glycogen with great rapidity; while rest and a sedentary life promotes its storage. The body readily converts its supply of glycogen into glucose, the form in which the body uses the carbohydrates for fuel.
Cellulose is a woody, fibrous material insoluble in water and to a certain extent impervious to the action of the digestive enzymes. This carbohydrate constitutes the skeleton of plants just as the bones constitute that of the animal body. It is probable that owing to the length of time required for this carbohydrate to be broken down in digestion, much of it escapes oxidation entirely. Hence, it passes down the digestive tract lending bulk to the food mass and [Pg 13] thus promoting peristalsis throughout the whole of the digestive tract.
Organic Acids.—Certain of the carbohydrate foods (fruits and green vegetables) contain appreciable amounts of organic acids or their salts; oranges and lemons, for example, are rich in citric acid; grapes contain considerable quantities of potassium acid tartrate, apples and other fruits have malic acid; many of the fruits have succinic acid; a few foods contain oxalic acid, or oxalates. All of these organic acids are burned in the body to produce energy, with the possible exception of the oxalates, which seem to have little, if any, food value. According to Sherman, these organic acids have a lower fuel value, per gram, than carbohydrates, but are reckoned as such in computing a food in which they exist. The function of these acids is chiefly that of neutralizing the acids formed in the body in metabolism. Being base-forming in character, they function after absorption and oxidation in the body as potential bases—the base associated with the acid in their ash combining with carbonic acid to form carbonates, which act as above described.
Bacterial Action upon Carbohydrates of Foods.—The bacteria that act chiefly upon the carbohydrates belong to the fermentative type. The substances formed as a result of this activity are certain acids—lactic, butyric, formic, acetic, oxalic, and possibly alcohol. Certain forms of carbohydrates are more susceptible to bacterial fermentation than others. Herter claims that sucrose and glucose are much more so than lactose, maltose, or starch. The substances thus formed through bacterial activity are not believed to be toxic in character, but merely irritating. However, the irritation arising from excessive fermentation in the stomach may lead to gastric disturbances of a more or less serious nature; hence the amount of carbohydrate taken under certain conditions must be adjusted carefully.
[Pg 14] The Effect of Heat upon Carbohydrates.—The changes wrought in the carbohydrates as a result of heat have already been discussed to a certain extent. It is seen that the sucrose (cane sugar) is soluble alike in hot and cold water; the same is true of maltose; but lactose is much more soluble in hot water than it is in water which has not been heated. So far as their digestibility is concerned, the application of heat (boiling) neither increases nor decreases the utilization of these sugars by the body.
With starch it is an entirely different matter. It has been found that the application of heat, either as dry heat, or in the presence of moisture, brings about a definite change in the character of the foodstuff. Pure starch admixed with water and boiled, passes into a condition of colloidal dispersion, or semi-solution, known as starch paste (Sherman). This is graphically illustrated in the cooking of potatoes, in which the starch and water are mixed in nature; and in the cooking of cereals and like starchy foods, to which water is added in preparation for their cooking. In both cases the application of heat adds greatly to the digestibility of the raw material by reason of the change which is wrought in these substances, causing them to be more readily acted upon by enzymes in the digestive juices.
This solubility of carbohydrates in hot water may be utilized in the washing of utensils in which these substances have been prepared; thus saving much time and effort on the part of the nurse in either the diet kitchen or in the home.
The second member of the organic food group, and one which is almost as widely distributed throughout animal and vegetable life as the carbohydrates, is found in the fats. This foodstuff, while composed of the same chemical elements that go to make up the carbohydrates, contains these [Pg 15] elements in different proportions; that is, fats contain less oxygen and more hydrogen than carbohydrates.
Typical Fats.—The fats (as already shown in the Table on page 5) are derived from both animal and plant life, but, like the carbohydrates, do not always occur in the same form. Those of animal origin include:
Adipose Tissue of man and animals, tallow of mutton, suet, and oleo oil of beef, lard of pork.
Phosphorized Fats, which include lecithin and lecithans, occur abundantly in the brain and nerve tissues and to a less extent in the cells and tissues of man, animals, and plants of which it seems an essential part. Egg yolk is the most abundant source of phosphorized fat in food material, but milk likewise furnishes an appreciable amount.
Cholesterol (fat-like substances).—“The fatty secretions of the sebaceous glands of man and of the higher animals which furnish the natural oil for hair, wool and feathers,” (Starling), lanoline, which is a purified wool fat, consist chiefly of cholesterol. According to Mathews, cholesterol is an essential constituent of the blood, and is found in the brain and in nearly all living tissues. It is likewise believed to be the “mother substance” from which bile acids are derived.
Fat Soluble “A.”—The vitamine factor which occurs dissolved in certain fats, namely, milk (whole), butter, egg yolk, the organs of animals, and codfish liver.
Definition of Fat.—The fats are all glycerides; that is, they are substances made up of combinations of fatty acids and glycerine, which constitute a definite group of chemical compounds, certain members of which are liquid in form, while others are solid, or semi-solid. The liquid fats are known as fatty oils. The fatty acids in which we are chiefly concerned in this study are: Butyric, Stearic, Oleic, and Palmitic. Most of the common fats owe their form and flavor to the type and amount of the various fatty acids of [Pg 16] which they are composed. For example, butter is made up of ten fatty acids; but its soft, solid form is due to the olein and palmitin (glycerides of oleic and palmitic acids) which it contains; and its characteristic flavor, as well as its name, to its butyric acid content (about 5 to 6%). It is evident that the degree of softness or hardness of a fat may be determined chiefly by the amount of oleic acid in its composition. Most of the common oils with which we are familiar in food are composed chiefly of olein. Stearin (the glyceride of stearic acid) is the hardest of the fatty acids, while palmitin, although classed with the solid fats, is not so hard as stearin. Lard and butter are higher in olein and palmitin and are consequently semi-solid, while suet and tallow, consisting chiefly of stearin, are much harder than the other food fats.
Characteristics of Fats.—The fats are all insoluble in water, and only partially so in cold alcohol, but they dissolve readily in ether. As a rule, the fat occurring in the animal body is more or less characteristic of the species. For example, animals that live on land have a harder fat than those living in the water; warm blooded animals, harder fats than cold blooded ones (fish); and carnivorous animals, harder fats than herbivorous species.
Fats are lighter than water, hence will float in it. An emulsion is a suspension of fat in a fluid, and the fat in this case must be very finely divided and mixed with some other material which will prevent a coalescence of the fat globules. In milk, which is one of the best natural emulsions, the additional substance is protein.
Effect of Heat upon Fat.—When fats are brought to a high temperature, the glycerine which they contain decomposes with the production of a substance known as acrolein, which has an irritating effect upon the mucous membranes. It is possible that the over-heated fatty acids add their quota to the production of irritating fumes. As [Pg 17] a rule, it is inadvisable to use frying as a method of preparing food for the sick or for children. Doubtless, if every cook understood the exact degree of heat to apply in frying, and knew just how moist to have the food mixture which she intended to cook in this manner, better results would be obtained; but since the average cook knows little about the scientific application of heat to fat or the changes brought about thereby, it is safer to make use of other methods of food preparation under the circumstances.
Functions of Fat.—This foodstuff undoubtedly serves as the most compact form of fuel available to the body for the production of energy. Weight for weight, fat furnishes twice as much heat as the carbohydrates, and in bulk the difference is even more striking; for example (about) two tablespoonfuls of sugar are required to produce 100 calories, whereas one scant tablespoonful of olive oil will produce a like number of heat units. As a source of supply for reserve energy in the body, fat is most valuable. This reserve fuel is stored in the form of adipose tissues underlying the skin and surrounding the vital organs, lending contour to the form and protecting the organs from jars and shocks. Distributed throughout the body, fat may be found as (a) cholesterol (in the cells of the muscles, organs, and nerve tissues), which acts as a protection against the destruction of the red blood cells; (b) phosphorized fat (lecithin), the universal distribution of which, according to Starling, seems to indicate that it plays an important part in the metabolic process of the cells, serving as a source of phosphorus which is required for the building up of the complex nucleoproteins of the cell nuclei.
Upon investigation it was found that neither the fats nor carbohydrates were the chief constituents of the active tissues. It was found, in fact, that the carbohydrates [Pg 18] occurred in very small quantities only in the muscles, and that frequently the quantity of fat was likewise limited. Other substances, containing nitrogen and sulphur in addition to carbon, oxygen, and hydrogen, which were invariably present, and which are essential constituents of all tissues and cells, both in animals and in plants, must be necessary to all known life. To these substances, believed at the time to be the fundamental constituents of all tissues, Mulder gave the name Protein, from the Greek, meaning “to take first place.” Later investigations proved that, while the proteins were essential to the building and repairing of the tissues and cells in general, they were not the only factors concerned in the work; that certain mineral salts were necessary constituents of all tissues, and must be present in order for any normal growth and development to occur.[4]
Composition of Proteins.—The average nitrogen content of common proteins is about 16%; that is, in 100 grams of protein there will be approximately 16 grams of nitrogen, or in 6.25 grams of protein there will be 1 gram of nitrogen. To estimate the protein content of a food when the percentage of nitrogen is known, it is necessary simply to multiply the percentage of nitrogen present, by the nitrogen factor, 6.25; or, if the amount of nitrogen is desired, when the percentage of protein is given, to divide by same factor.
Construction of Proteins.—In plant structure the building up of the proteins is accomplished by the plants from inorganic substances existing in the soil and air; but in the animal body this is not possible, because the construction of the tissues requires the use of other proteins—the most available ones being found in food. Each animal [Pg 19] (or species) forms the proteins characteristic of its own tissues,—while the proteins of food are similar to those found in the body, they cannot be utilized in their original form, but must be split into simpler substances from which the cells of the various tissues throughout the body may select those particularly adapted for their purpose. These transformed substances are known as amino acids, the production of which is a result of digestion in the digestive tract. There are about seventeen of these acids entering into the construction of the common proteins. One scientist has likened these units to letters of the alphabet, which, being combined, spell many proteins. When a protein contains all of the essential units, it may be said to be “complete,” the best example of which may be seen in milk, eggs, and meat. When a protein lacks some of the essential elements, or letters of the protein alphabet, it is said to be incomplete. Gelatin is the best example of this type of protein, but the cereals and beans must likewise be supplemented by other substances; milk being the one most generally used for this purpose. For the purpose of building young tissues, and maintaining those already mature, it is logical to use foods containing the foodstuffs in their best form; that is, those that not only contain the complete protein, but also the requisite mineral salts and vitamines. Foods lacking in some of these respects become adequate when supplemented by these foods which can supply the missing constituents; hence, the use of such incomplete protein foods need not necessarily be abandoned, for, as in the case of cereals, the foods are both economical and palatable, and, when used in addition to milk, furnish valuable adjuncts to the dietary.
Classification of Proteins.—A brief description of some of the more important proteins with which we are chiefly concerned will serve to simplify the formulation of a diet. Those assuming the most important position in nutrition [Pg 20] and food are globulins, albumens, nucleoproteins, phosphoproteins, hemoglobins, and derived proteins such as proteoses and peptones. The albumens and globulins associated together occur in the tissues of both animals and plants. The albumens are richer in sulphur than the globulins and are found more abundantly in the animal fluids, such as the blood, while the globulins predominate in the more solid tissues of animals and in plants. The close association of these two proteins is particularly noticeable in the blood and cells. They have different characteristics, however.
Albumins.—The best examples are found in egg albumin (white of egg), lactalbumin (milk), serum albumin (blood), leucosin (wheat), legumelin (peas). Albumins are all soluble in pure water, and are coagulable by heat. Coagulation, due to the action of the ferments in the body, takes place in milk, blood, and muscle plasma. Certain albumens are particularly adapted for the building and repairing of tissues. Among those that have been used in feeding experiments to determine whether or not they were capable, when used as the sole protein in the diet, of maintaining animals in normal nutrition, and of supporting normal growth in the young animal,—may be cited lactalbumin and egg albumin. These experiments provided diets adequate in other respects, the object being to determine the value of the various proteins. It was found that the albumin from milk was more efficient in this respect than the egg albumin.[5]
In the invalid dietary the solubility of the albumins in water makes them of especial value as reinforcing agents, since they may be introduced into fluids without materially altering either their flavor or their bulk.
Globulins.—Simple proteins, insoluble in pure water, [Pg 21] but soluble in neutral salt solutions; examples, muscle globulin, serum globulin (blood), edestin (wheat), physelin (beans), legumin (beans and peas), tuberin (potatoes), amandin (almonds), arachin, and conarachin (peanuts).
Alcohol-Soluble Proteins.—Simple proteins soluble in alcohol of from 70-80% strength. Insoluble in absolute alcohol, water and other neutral solvents. Examples of these proteins may be seen in the gliadin of wheat, zein of corn, and hordein of barley.
Albuminoids.—These substances represent one group of incomplete proteins, inasmuch as they cannot alone support protein metabolism. However, they are classed with the proteins and may be substituted for at least a part of these compounds in the daily dietary, since they are able to do much of the work of the pure proteins. The best example of this group is seen in gelatin. This substance contains many of the structural units of meat protein but in very different relative amounts. It has not, therefore, the chemical units necessary to repair the worn-out parts of cell machinery.[6]
Conjugated Proteins:—Nucleoproteins, Phosphoproteins and Hemoglobin.
(a) Nucleoproteins.—This type of protein is characteristic of all cell nuclei, and is particularly abundant in the highly nucleated secreting cells of the glandular organs, such as the liver, pancreas, and the thymus gland. The nucleoproteins are composed of simple proteins and nuclein. Nucleic acid is rich in phosphorus and upon decomposition yields some of the purin bases (xanthin, adenin, guanin), a carbohydrate and phosphoric acid.[7]
(b) Phosphoproteins.—Compounds in which the phosphorus is in organic union with the protein molecule otherwise than a nucleic acid or lecithin. Examples: caseinogin (milk), ovovitellin (egg yolk).
[Pg 22] (c) Hemoglobin.—Much of the greater part of the iron existing in the body occurs as a constituent of the hemoglobin of the red blood cells. When the intake of iron is not sufficient to cover the output, there must be a consequent diminution in the hemoglobin of the blood with a corresponding development of anemia.
The importance of knowing these characteristic proteins is apparent. Not only will such knowledge lead to a more intelligent use of protein foods in the normal dietary, but it will prove of the greatest assistance in the adjusting of the foodstuffs in diet for individuals suffering from certain abnormal conditions.
In abnormal conditions this knowledge of the various proteins—their composition, source, and behavior in the body assumes a position of the greatest importance; since it represents the means for safeguarding a patient from the results caused by the wrong kind of food. In certain types of nephritis, for example, it is perfectly safe to give milk where the ingestion of meat and eggs might cause serious, if not fatal, results. In treating gout, when it is deemed advisable to limit the purin foods in order to control in a measure the retention of uric acid in the body, the realization that certain of the nucleoproteins, upon being broken down in the body, yield the purins, which in turn give rise to the production of uric acid, will permit the nurse to adjust the diet so as to eliminate such foods entirely (see Gout). The importance of keeping the hemoglobin content of the blood normal has already been mentioned.
The Effect of Heat upon Proteins.—The fact that certain proteins are most susceptible to heat has already been stated, but the application of this knowledge in the preparation of protein foods is important. In milk, for example, whole raw milk forms a large hard curd; whereas boiled milk curdles in a much finer and softer form. Pasteurized [Pg 23] milk shows smaller curds than raw whole milk, but larger than the boiled whole milk.[8]
An egg cooked by the application of a long-continued high temperature (212° F.) has a tough white; whereas an egg cooked until hard at a temperature under the boiling point shows a tenderness in the white which renders it distinctly more palatable. Soft-cooked eggs leave the stomach in less time than is required for hard cooked ones; poached (cooked in water under the boiling point), shirred eggs (cooked in hot dish), and soft-cooked eggs are among the most readily digestible forms of eggs. Raw eggs are slightly less stimulating to acid secretion in the stomach and require a longer time to leave the stomach than boiled eggs. Thus it is seen that in many cases the difference in preparation of the protein foods may make a difference in the way in which the digestive tract handles them. Necessarily, this point is emphasized more in abnormal than in normal conditions; for example, albuminized orange juice gives rise to a distinct gastric secretion, and leaves the stomach rapidly—a great advantage in certain abnormal conditions, and especially in those requiring liquid diet of high nutriment value.
The knowledge of the coagulation of proteins by heat points out the advantage of using cold water over hot in the preliminary cleansing of utensils in which protein foods have been prepared. Certain members of this group are soluble in pure water, and will readily dissolve; whereas, if the water is heated, their coagulation would prevent this taking place so readily.
Functions of Protein in the Body.—The proteins serve two distinct uses in the body; first, that of building and repairing tissues and furnishing, in conjunction with other [Pg 24] substances, material for growth; second, that of producing energy for the internal and external work of the body. For this latter function a large percentage of the proteins ingested is used; consequently, since the carbohydrates and fats are primarily the energy furnishing material most readily used by the organism, it is clearly demonstrated that the average individual takes more protein into the body than is necessary for its maintenance. Except during the period when an allowance for growth must be made, it is probable that a much smaller daily consumption of protein could be made without disadvantage to the organism, leaving the bulk of the work, in so far as the running of the engine is concerned, to the other organic foodstuffs.
Man can exist for days, even weeks, without food, but without water life soon becomes extinct. This substance is composed of hydrogen and oxygen in the proportion of two to one; that is, to each atom of oxygen there will be found two atoms of hydrogen. This is always the case no matter where it is found. When foods are put through a drying process the water is taken out and the rest of the chemical composition of the food remains unchanged.
This foodstuff, unlike those belonging to the organic group, is not changed during the process of digestion, nor does the application of heat or cold affect it, save from a physical standpoint. Water boils at a temperature of 100° C. (212° F.), and freezes at a temperature of 0° C. (32° F.).
Function of Water.—The uses of water in the body are many, and the advantage arising from a sufficient amount of this foodstuff in the dietary cannot be overestimated. It is no longer considered an error in diet to drink a moderate amount of water with the meals, so long as it is not used as a substitute for mastication, and as a means [Pg 25] of washing the food into the stomach. In the diet, both as a beverage and as a part of most of the food materials ingested, water serves to moisten the tissues; to furnish the fluid medium for all of the secretions and excretions of the body; to carry food materials in solution to all parts of the organism; to stimulate secretory cells producing the digestive juices, thereby aiding in the processes of digestion, absorption and excretion; to promote circulation; to furnish material for free diuresis, thus preventing to a great extent the retention of injurious substances by the body, which might otherwise take place.
Factors Determining the Amount of Water Needed.—In normal conditions it is probable that the kind and amount of exercise taken has more to do with the amount of water needed by the body than any other factor, since the vigorously worked body excretes more water by way of the skin than the quiescent one. With a normal amount of exercise, it is advisable to drink from six to eight glasses of water each day, increasing the amount to a certain extent when exercise causes a great loss through perspiration. It is always advisable, however, to keep in mind that an excessive amount of fluid taken into the body throws a corresponding amount of work on the organs (the stomach, kidneys and heart). In certain abnormal conditions, the body’s water supply is depleted. This is particularly true in the case of hemorrhage, vomiting, and diarrhea. Under other conditions (certain types of nephritis), the body becomes overburdened through the excess of water retained, owing to the difficulty which the kidneys show in eliminating it. This retention of water by the tissues gives rise to the condition known as edema.
Ash.—The eight remaining chemical elements, i.e., calcium, magnesium, sulphur, iron, sodium, potassium, [Pg 26] phosphorus, chlorine, constituting the mineral salts or ash, are likewise classed as food on account of the work which they perform in the body. Some of these elements enter the body as essential constituents of the organic compounds, and are metabolized in the body as such, becoming inorganic only upon oxidation of the organic materials of which they form a part.
Importance of the Mineral Salts.—The way in which the mineral elements exist in the body and take part in its functions, has been graphically outlined by Sherman as follows.
“(1) As bone constituents, giving rigidity and relative permanence to the skeletal tissues. (2) As essential elements of the organic compounds which are the chief solids of the soft tissues (muscles, blood cells, etc.). (3) As soluble salts (electrolytes) held in solution in the fluids of the body; giving to those fluids their characteristic influence upon the elasticity and irritability of muscle and nerve; supplying material for the acidity and alkalinity of the digestive juices and other secretions; and yet maintaining the neutrality, or slight alkalescence, of the internal fluids as well as their osmotic pressure and solvent power.”[9]
The above outline, showing the various ways in which the mineral constituents enter and take part in the various functions, as well as in the structure of the body, make it evident that the same close attention and study which was given to the other foodstuffs must be accorded to these substances. When the student realizes that the presence of certain salts dissolved in the blood assists in the regulation of the vital processes of the body such as the digestion, circulation and respiration; that they are responsible for the contraction and relaxation of the muscles; that they assist in controlling the nerves; that they are, in a way, [Pg 27] instrumental in releasing the energy locked up in food—the value of these elements becomes very evident, and their importance in the dietary inestimable. Some of the mineral salts are more widely distributed in food than others, and the danger arising from their deficiency in the diet is not so great as is the case with others; hence attention is called to those found by investigators to be most often lacking or deficient in the average diet; i.e., calcium, phosphorus, and iron. A brief summary of the special parts played by these elements will be outlined here.
Calcium.—Physiology teaches that about eighty-five per cent. of the mineral matter of the bone, or at least three-quarters of the ash of the entire body, consists of calcium phosphates. It has long been known that this mineral salt is necessary for the coagulation of the blood, and science has demonstrated that “the alternate contractions and relaxations which constitute the normal beating of the heart are dependent, at least in part, upon the presence of a sufficient, but not excessive concentration of calcium salts in the fluid which bathes the heart muscles.”[10]
Phosphorus.—According to Sherman, phosphorus compounds are as widely distributed in the body, and as strictly essential to every living cell as are proteins. Science has also proved that they are important constituents in the skeleton, in milk, in glandular tissue, in sexual elements, and in the nervous system; that these compounds take part in the functions of cell multiplication, in the activation and control of enzyme actions, in the maintenance of neutrality in the body; that they exert an influence on the osmotic pressure and surface tension of the body, and upon the processes of absorption and secretion. Like calcium, phosphorus is absolutely essential to the growth and development of the body, and, as in the case of the mineral, its presence in the dietary must be accorded strict attention, in [Pg 28] order to avoid the results accruing from its deficiency. Casein, or caseinogen of milk and egg yolk (ovovitellin), are the substances richest in this mineral salt. The fact that the phosphorus existing in grains (cereals) may be removed largely in the process of milling, makes it advisable to consider the use of the breads made from the whole grains.
Iron.—The presence of iron as an essential constituent of hemoglobin has already been discussed. That which is not in the hemoglobin is chiefly found in the chromatin substances of the cells.
The body does not keep a reserve store of iron on hand as is the case with calcium and phosphorus in the bone tissues, but must depend upon the daily intake in food to supply its needs. The iron content of food materials is not large, but a careful regulation of the iron bearing foods (see Table on page 5) will make it easy to cover the demands of the body with a material which has been found to do its work most efficiently. Medicinal iron has received much attention in the determination of the essential needs of the body. “Whether medicinal iron actually serves as material for the construction of hemoglobin is not positively known, but we have what appears to be a good evidence that food iron is assimilated and used for growth and for regeneration of the hemoglobin to much better advantage than are inorganic or synthetic forms, and that when medicinal iron increases the production of hemoglobin, its effect is more beneficial in proportion as food iron is more abundant—a strong indication that the medicinal iron acts by stimulation rather than as material for the construction of hemoglobin” (Sherman).
The newborn infant has a store of iron already on hand, derived from the mother through the placenta before birth. After the birth, and through the nursing period, the child receives a certain amount of iron from the mother’s milk. This supply is not altogether reliable, however, since any [Pg 29] disturbance of the digestion will tend to interfere with its absorption, and consequently deprive the organism of what would otherwise be used for the building up of the blood supply. Thus it is clearly indicated that the infant’s safest source of iron is from the mother during the pre-natal period. This supply must necessarily come from her diet during this time, and is made possible by regulating day by day the iron bearing foods in her dietary. After the original store of iron is reduced to that of the adult (after the child has tripled in birth-weight, generally at 12 or 13 months), and during the remainder of the growth period, it is very necessary to regulate the iron-bearing food in the diet, in order to insure the child of an adequate amount to cover the demands made by the increasing blood supply.
Up to a few years ago it was believed a complete diet should contain an adequate amount of protein of a proper type, a sufficient amount of calcium, phosphorus and iron, and enough carbohydrates and fats to furnish the body with sufficient fuel to cover its energy expenditures. This belief was proved to be incorrect a number of years ago by Dr. Hopkins of England. In making certain feeding experiments with rats, Dr. Hopkins showed that some substance or substances present in milk, other than those already mentioned, was essential for the growth of the animal; that animals deprived of this material grew for a time, but gradually ceased to do so. Later on, Osborne, Mendel, McCollum and Davis discovered a like substance in butter fat; and still later Dr. McCollum found the same growth stimulating material, or one very like it, existing in the leaves of plants. These scientists found, upon investigation, that there were probably two substances in milk—one soluble in the fat, the other in the protein-free and fat-free whey—both of which were essential for normal growth. In [Pg 30] 1911 Dr. Funk discovered in rice polishings a substance which he believed to be a cure and preventive of Beri-beri; to this substance, which is now believed to be identical with the second substance found in milk, he gave the name “vitamine.” Dr. Funk’s name “Vitamine” is now accepted to cover a number of substances essential to growth, and for the prevention and cure of certain diseases. To the first two has been added a third member of the vitamine family, which has proved to be a cure and preventive of scurvy. These substances are called—on account of the substances in which they are soluble—“Fat soluble A,” “Water soluble B,” and “Water soluble C.” The table on page 496 shows the sources from which these factors may be obtained. The four plus system is used by Dr. Eddy to describe the abundance with which they occur.[11]
Function of “Fat Soluble A.”—All investigators agree that the “A” vitamine is an essential factor in the growth of young tissue, and the repair of mature tissues. McCollum claims that this vitamine is likewise a factor in the prevention of the eye disease known as xerophthalmia, and other scientists also hold this opinion. Eddy states that a diet lacking in the “A” vitamine will, in the majority of cases, result in stunted growth and the development of the eye disease, and that the appearance of the latter may be taken as a sure indication of the absence or deficiency of this vitamine.
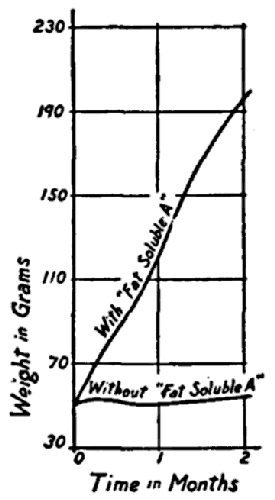
The following diagram shows the effect of adding fat soluble “A” to the diet which was adequate in other respects. This chart represents the growth curve of young rats.[12]
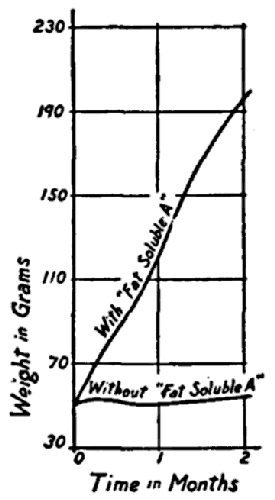
Figure showing the effect upon growth of adding “fat soluble A”
to a diet adequate in all other respects.
Courtesy of Dr. E. V. McCollum.
Mellanby of England believes the “A” vitamine to be a factor in the prevention of rickets. Scientists of America have recently investigated this disease, and Dr. Hess (New [Pg 31] York) has found cod liver oil to be a remedy for it. Cod liver oil is known to be rich in “Fat soluble A,” but whether the cure of rickets is due to the presence of this vitamine in the oil, or to a possible fourth vitamine, is still undetermined.
Effect of Heat on the “A” Vitamine.—Heat, as applied in the ordinary methods of cooking, is not believed to exert a great deal of destruction upon the “A” type of vitamine; but hydrogenation, the process used in the hardening of certain fats in the manufacture of lard substitutes, is said to destroy it completely.
“Water Soluble B.”—The second vitamine discovered in milk and believed to be identical with the Funk vitamine is more widely distributed than the “A” vitamine. For this reason it is not so likely to be deficient in the diet as is found to be the case with the “A.” A glance at the table shows that the best sources outside of yeast are the seeds of plants and the milk and eggs of animals. In beans and peas the “B” vitamine is distributed throughout the entire seed, but in the cereal grains it is found chiefly in the embryo. As a result, bread made from fine white flour or meal is much more apt to be deficient in vitamine of the “B” type than that which is made from the whole grain; the same is true of rice and other cereals. Spinach, potatoes, carrots and turnips show an appreciable amount of the vitamine, but beets are known to be extremely poor in it. Nuts too are considered a valuable source.
Function of the “B” Vitamine.—Like the “A” vitamine, water soluble “B” is believed to be essential to growth. [Pg 32] Funk established its value as a preventive and cure of Beri-beri, the disease common in the Orient among people living largely upon a diet of polished rice and fish. Besides being a growth-stimulating substance and an antineuritic, the “B” vitamine is highly valued for its stimulating effect upon the appetite. To this property is probably due at least part of the credit for which certain substances work for the promotion of growth in animals. This can be utilized to good advantage for children showing a disposition to refuse food, by supplementing formulas made from milk,[13] with the expressed juice of vegetables and fruits known to be rich in the “B” vitamine.
Effect of Heat on the “B” Vitamine.—This vitamine also shows a resistance to heat; that is, as applied in the methods generally used in cooking, pasteurization temperatures do not materially affect the vitamine property of the formula as far as the “A” and “B” factors are concerned.
The Effect of Alkali (Soda) upon the “B” Vitamine.—It has been an ordinary practice to add soda to the water in which certain vegetables are cooked, for the ostensible purpose of softening the vegetables and hastening their cooking. The practice has been condemned by many scientists who are making experiments along these lines, on account of its destructive power upon the “B” vitamine. Chick and Hume in England claim that when the amount of food given contains originally just sufficient vitamines to cover the growth factor the use of soda in the cooking water does serious harm to these vitamines. This is a point well worth remembering. It is often difficult to persuade certain individuals to eat vegetables in appreciable quantities; if the vitamines were reduced though the method of preparing the food, these individuals would not obtain a sufficient quantity of the vitamines.
[Pg 33] “Water Soluble C.”—The third member of the vitamine family is known for its antiscorbutic property; that is, it is the best known cure and preventive of scurvy. It likewise exerts a certain amount of influence upon the growth of the animal and must be present in the diet, in order that the health and well-being of the individual may be safeguarded. The “C” vitamine, like the “B” vitamine, is soluble in water, and is present to an appreciable extent in the fresh juices of the fruits and vegetables. Some are richer in this respect than others (orange and tomato juice), while the cereals, grains, seed of plants, sugars, oils, and meats are singularly deficient. Milk (whole) does not contain a great amount of the “C” vitamine, and this amount is still further reduced under certain methods of preparation. Milk powders, made either from the whole or the skimmed milk, are found to contain only very small amounts of this essential substance. Condensed milk and cream are supposed to be free of “C,” and the same is true of eggs.
Effect of Heat on “C” Vitamine.—All authorities agree that the “C” vitamine is much more sensitive to heat than the other two; and for this reason much of the value obtained from this vitamine in uncooked material may be lost when the food containing it is subjected to long-continued heat. Hess claims that the temperature used for pasteurizing milk for some time, is more destructive to this vitamine than boiling water temperature continued for a few minutes only.[14] There is need for care in formulating the diet for children to see that they are given fresh fruit every day; or when that is not possible, to see that they are at least given tomato juice. This substance is rich in the antiscorbutic vitamine, and according to experiments made by Sherman, LeMer and Campbell, loses fifty per cent. of its antiscorbutic power when boiled one hour. Dr. Delf at the Lister Institute experimented with raw and cooked [Pg 34] cabbage, and found that when this material was cooked for one hour at temperatures ranging from 80° to 90° C the loss in antiscorbutic power amounted to 90% in the cooked leaves over the raw material. Dr. Delf also concluded from her experiments that it was advisable to add neither acid nor alkali in the cooking of vegetables if these substances were to give their maximum value of vitamines.
From the foregoing description of these vitamine factors, it is readily seen why so many dietaries are deficient in these essential substances. The limited sources from which to obtain the “A” vitamine; the sensitiveness of the “B” vitamine to the action of alkalies; the sensitiveness of the “C” vitamine to heat, alkali and acid, moreover the limitation of its presence chiefly to the fresh fruits and plant juices,—all point to the need of special care in the selection of the food materials and of the manner in which these materials are prepared for consumption.
In the descriptions just given of the various foodstuffs, especially in regard to their function in the body, it is readily seen that no one foodstuff is used to the exclusion of another. It is further seen that in the upkeep of the body, which includes not only the building and repairing of its tissues, but the running of the engine and maintaining of its normal temperature, the organism uses each and all of the organic food substances for the production of heat. Furthermore, while the tissues are chiefly built from protein material, and physiology teaches that protein can be built only from other protein, these tissues contain a certain amount of carbohydrate, fat, mineral salts, and water; this furnishes distinct evidence that the building of the cells and tissues of the body cannot be accomplished by means of protein alone, but by the judicious balancing of all the foodstuffs in the dietary.
[Pg 35] Science has gone even further than this, as has just been demonstrated, and has proven that without the substances known as vitamines the normal growth and development in the young would be arrested, and that the maintenance of the adult body would be impaired. It has also proven that certain diseases owe their development to deficiencies in the vitamine supply to the body.
(a) Outline briefly what is believed to be the essentials of an adequate dietary.
(b) List the fuel foods and show their most economical source.
(c) List the best sources of the complete proteins.
(d) Show how the incomplete protein foods may be made adequate for growth.
[1] One quart of milk contains more calcium than a quart of clear saturated solution of lime water.
[2] For complete list, see Eddy’s Table, in Appendix.
[3] “Chemistry of Food and Nutrition” (revised edition), by Sherman.
[4] Scientists are proving the need for certain vitamine factors in the diet in order that the growth and development of young tissues and the repair of adult tissues may proceed. The part played by these substances will be discussed later.
[5] “Chemistry of Food and Nutrition” (2d ed.), by Sherman.
[6] “The Basis of Nutrition,” by Graham Lusk.
[7] “Food Products,” by Henry Sherman.
[8] Abstracts made from thirteen papers from the Laboratory of Physiological Chemistry, Jefferson Medical College, Philadelphia; published in the “American Journal of Physiology and Science,” by Minna C. Denton. U.S. Department of Agriculture.
[9] “Chemistry of Food and Nutrition” (revised), p. 333, by Henry Sherman.
[10] “Chemistry of Food and Nutrition” (revised edition), by Sherman.
[11] “The Vitamine Manual,” p. 64, by Walter Eddy
[12] Courtesy of Dr. E. V. McCollum.
[13] Milk from cows whose diet has been deficient in vitamines shows a like deficiency in vitamine content—the same is true of mother’s milk.
[14] “The Vitamine Manual,” p. 64, by Walter H. Eddy.
Science has proved that the human body is composed of certain chemical elements and that food materials are combinations of like elements; it has likewise proved that the body will utilize her own structure for fuel to carry on the work of her various functions unless material is supplied for this purpose from an outside source, namely, food, which in chemical composition so closely resembles that of the human body.
Amount and Type of Food.—The next point of investigation would logically be the amount and kind of food necessary to best accomplish this purpose. To be able to do this it was necessary to have some standard unit by which to measure the amount of heat each food was capable of producing when burned outside the body, after which it was more or less simple to calculate the heat production of each of the food combinations within the organism. An apparatus known as the “Bomb Calorimeter”[15] was devised by Berthelot, and adapted for the examination of food materials by Atwater and Blakesley. The food material to be tested was placed within the bomb, which was charged with a known amount of pure oxygen. The bomb was then sealed and immersed in a weighed amount of pure water, into which a very delicate thermometer was inserted. The food within the bomb was ignited by means of an electric fuse, and the heat given off by the burning of the material was communicated to the surrounding water and [Pg 37] was registered upon the thermometer. It was evident that some definite name had to be devised by which these heat units might be known. Hence the name “calorie,” which represents the amount of heat required to raise the temperature of 1 kilogram of pure water 1 degree centigrade, or about 4 pounds of water 1 degree Fahrenheit.
Transformation of Foods into Available Fuel.—A comparison has been made between the human body and steam engine, but this comparison is not adequate, since the food does not produce heat within the body originally, but energy of which heat is a by-product. Each food combination has a certain amount of dormant energy within its structure and this energy does not become active nor can it be utilized by the body until the food, of which it is a part, is changed within the organism to substances more nearly like its own. This liberated active energy is then used as a motive power to carry on the internal and external work of the body, and the heat, which is invariably the consequence of any active energy (motion), leaves the body as such. It will be seen, then, that the human body acts not as a steam engine, but rather as a transforming machine by means of which the dormant energy of the food is transformed into an active agent of which heat is a natural result.
In the calorimeter it was found that the carbohydrates and fats burned to the same end products, namely, carbon dioxide and water, while the proteins, upon oxidation, produced carbon dioxide, water and nitrogen gas. In the body it was found that the carbohydrates and the fats acted in exactly the same manner as in the calorimeter, producing the same end products. But this was not the case with the proteins; the oxidation process of this chemical combination was found to be not nearly so complete within the body as in the calorimeter, and instead of the free nitrogen as produced in the apparatus there were urea and other [Pg 38] nitrogenous substances eliminated which, while combustible, represented a less complete oxidation of the proteins.
The following table represents the amount of heat produced as the result of a complete oxidation of the foodstuffs in the calorimeter.
TABLE[16]
| Carbohydrates | 4.10 cal. per gram |
| Fats | 9.45 cal. per gram |
| Protein (nitrogen × 6.25) | 5.65 cal. per gram |
The loss of potential energy due to the incomplete oxidation of the proteins in the body is approximately 1.3 calories to each gram of protein in food; consequently in calculating the fuel value of protein foods, due allowance must be made for these losses. Allowance must also be made for the incomplete digestion, or losses occurring in the digestion, of the foodstuffs. These losses, as well as the approximate amount of each constituent absorbed, are represented in the following table.[17]
| Lost | Absorbed | |
| Carbohydrates | 2 per cent. | 98 per cent. |
| Fats | 5 per cent. | 95 per cent. |
| Proteins | 8 per cent. | 92 per cent. |
The physiological fuel factors of food, or the amount of heat produced as the result of combustion of 1 gram of organic food material after the above-mentioned losses have been accounted for, may be obtained as follows.[18]
| Carbohydrates | 4.10 × 98% = 4 cal. per gram |
| Fats | 9.45 × 95% = 9 cal. per gram |
| Proteins | 4.35 × 92% = 4 cal. per gram |
In primeval days, when man led a more natural life, his very existence depended upon his ability to wrest from the earth his 4—9—4; these, then, constitute what are known as the “physiological fuel factors” of carbohydrates, fats, and proteins respectively.
Determination of Fuel Value of Food.—In determining the amount of heat produced by a given amount of food, it is first essential to reduce the amount to grams (for example, 1 lb. equals 480 grams): first, because the gram is a unit of weight commonly used in dietetic calculations; second, because the fuel factors are based on the amount of heat produced by the burning of one gram of organic foodstuffs. Knowing the composition of food, that is the number of hundredths of protein, carbohydrate and fat it contains, it is a simple matter to estimate its fuel value by multiplying the amount of each contained in one gram by its physiological fuel factor 4.4.9. Thus if the composition of a food is 3-3/10% protein, 4% fat and 5% carbohydrate, one gram would contain .033 gram of protein, .04 gram of fat and 0.5 gram of carbohydrate. Hence one gram of milk would produce
| .033 × 4 | = | .132 calorie from protein |
| .040 × 9 | = | .360 calorie from fat |
| .050 × 4 | = | .200 calorie from carbohydrate |
| or | .692 calorie in all |
But it is not necessary to estimate the fuel value of so small a quantity as one gram, and, since the value of protein, carbohydrates and fats is always the same it is more satisfactory to estimate the amount of the organic constituents contained in the entire given quantity of food, rather than stopping to figure out the fuel value of the small quantity.
This is done by multiplying the entire number of grams of food given by the amount of protein, fat and [Pg 40] carbohydrate contained in one gram, then multiplying these results by the physiological fuel factor of each. Thus 100 grams of milk would yield
| 100 × .033 | = | 3.3 × 4 | = | 13.2 calories from protein |
| 100 × .040 | = | 4.0 × 9 | = | 36.0 calories from fat |
| 100 × .050 | = | 5.0 × 4 | = | 20.0 calories from carbohydrates |
| or a total of | 69.2 calories from 100 grams of milk. | |||
The Standard or 100 Calorie Portion.—Just as it has been more convenient to estimate a larger rather than a smaller quantity of food material, so it is frequently more desirable to estimate a hundred calories, rather than one calorie. This is especially useful when dietaries of high caloric (fuel) value are to be estimated, or dietaries in which foods of like composition and fuel value are to be interchangeable. In such cases it is a simple matter to select the desired number of 100 calorie portions of those foods which are to make up the dietary.[19]
Method of Estimating the 100 Calorie Portion.—The number of calories yielded by 100 grams of food material is taken as a basis upon which to estimate the 100 calorie portion, and X represents the number of grams required to yield this portion. The problem is one of “simple proportion,” for example, take the 100 grams of milk just estimated, we found that 100 grams (or c.c.) furnished 69.2 calories of heat, then, 100:69.2 :: X:100—145; or 145 grams of milk are required to furnish 100 calories of heat. Suppose it is desirable to substitute eggs for a part of the milk in the diet, eggs have a higher fuel value per unit of weight than milk, their average composition being 13.4% protein, and 10.5% fat (no appreciable amount of carbohydrates), 100 grams of eggs would yield
| 100 × .134 | = | 13.4 × 4 | = | 53.6 calories from protein |
| 100 × .105 | = | 10.5 × 9 | = | 94.5 calories from fat, |
| or a total of | 148 calories. | |||
[Pg 41] The Standard or 100 calorie portion of eggs would be,
100:148 :: X:100 = 68
or the number of grams required to yield 100 calories.
Thus it is seen that in using the fuel value of a hundred grams of food material for estimating the standard or 100 calories portion the extremes are always the same. Hence, the weight of the 100 calorie portion may always be obtained by multiplying the extremes and dividing the result by the number of calories furnished by 100 grams of food material.
(a) Compare the fuel value of the various common food materials.
(b) How does the fuel value of a chicken salad compare with that of fruit salad?
(c) Figure the fuel value of a cupful of cream of tomato soup and compare it with that furnished by the same quantity of beef broth.
(d) Weigh and measure a 100-calorie portion of spinach and compare it with a 100-calorie portion of sweet potato.
[15] For full description and methods used, see “Journal of The American Chemical Society,” July, 1903.
[16] “Chemistry of Food and Nutrition” (revised edition), by Sherman.
[17] “Chemistry of Food and Nutrition,” by Sherman.
[18] “Chemistry of Food and Nutrition” (revised), by Sherman.
[19] See Table of Standard or 100 Calorie Portions, in Appendix.
The human body, as far as can be judged, does not use one nutrient to the exclusion of another, but science has proved that the best results are obtained from diets balanced to suit the needs of the body, providing the fuel and repair materials in the amounts which are calculated to give the maximum value with the minimum expenditure on the part of the organism.
For while no two individuals are exactly alike, there are factors which govern or influence the food requirements of all, and thus make it possible to estimate the needs of the body with a fair degree of accuracy.
It has been found, by means of calorimeter experiments (direct and indirect), that a certain amount of heat is produced within the body, regardless of external movement or food; that is, when a body is lying absolutely quiet with no movement save that of breathing, the internal work of the organism, which is continuous, releases so much heat, and this is produced whether there is food to replace it or whether the body structure is burned. This is known as the basal rate of metabolism, and constitutes the normal basal requirements. Any external movement will increase this rate; the greater the activity the higher the increase. Consequently external work calls for food in addition to that which is used to run the engine, in order to save the body from destruction.
DuBois[20] finds “Basal Metabolism above normal in exophthalmic goiter, in fevers, in lymphatic leukemia, and [Pg 43] in pernicious anemia, in severe cardiac disease, and in some cases of severe diabetes and cancer; it is lower than normal in cretinism, and in myxedema, in old age, in some wasting diseases and perhaps in some cases of obesity.” This fluctuation in the Basal Rate of metabolism furnishes a factor in the diagnosis of disease, not only recognized but coming more and more in use.
For the Adult.—Muscular activity, Age and Size, are most important factors influencing the food requirements. The physical condition and environment of the individual also exert a certain amount of influence upon the intake of food.
Work.—Muscular activity, as already stated, increases the body expenditures; consequently the more active the work the greater amount of energy food needed per unit of weight.
Age.—As the individual grows older, the rate of metabolism decreases until, in old age, it is not more than a third to a fifth of what it was in earlier life. This is due to a general “slowing down” of the machinery, the heart does not beat so rapidly, nor is the respiration so quick. The digestive organs, the heart, the liver, and the kidneys, cannot handle the volume of food which was required during the period of greatest physical activity. Hence, any great excess over and above that which is needed for the maintenance of the body in health will be a source of danger to the elderly person. Von Noorden claims the food requirements of individuals from
60 to 70 years of age to be reduced 10%; for people from
70 to 80 years of age to be reduced 20%; for people from
80 to 90 years of age to be reduced 30%.
[Pg 44] Sex.—Science has proved, that there is little difference in the food requirements of men and women, provided they are alike in age, weight and size, and are doing the same amount and type of work. But women, as a rule, weigh less than men, hence their food requirements are approximately less.
Murlin finds the food requirements of pregnant women to be some what higher than of non-pregnant ones, and the requirements of the nursing mother to be higher than either (see chapter on Pregnancy and Lactation).
For the Child.—The factors influencing the food requirements are different, to a certain extent, from those of the adult. The main difference lies in the fact that the adult needs food only for the maintenance and repair of the body, while the child must have food, not only to cover its maintenance requirements, but to support the growth and development which should be continuous from birth to maturity. Resistance, too, must be developed during this period in order to safeguard the child through life.
The rate of metabolism in the infant is greater than at any other period of life, consequently, even if a child were one-third the weight of its parent, it would inevitably cease to grow and would become malnourished, if its food requirements were reckoned at only one-third that of the parent.
Adjusting the Food Requirements.—Taking these factors as guides for estimating the food requirements of man, it is evident that no hard and fast law can be laid down to cover all, that each individual must adjust the food intake according to the weight and activity of the body. Sherman has arranged the following table showing the energy expenditures per hour for the average man (154 pounds), per pound of body weight (these are approximate averages only).
TABLE[21]
| Sleeping quietly | 60-70 calories per hour |
| Awake, lying still | 70-85 calories per hour |
| Sitting at rest | 100 calories per hour |
| Standing at rest | 115 calories per hour |
| Tailoring | 135 calories per hour |
| Typewriting rapidly | 140 calories per hour |
| “Light exercise” (stationary bicycle) | 170 calories per hour |
| Shoemaking | 180 calories per hour |
| Walking slowly (about 2¼ miles an hour) | 200 calories per hour |
| Carpentry or metal work | 240 calories per hour |
| “Active exercise” (stationary bicycle) | 290 calories per hour |
| Walking briskly (about 3¾ miles an hour) | 300 calories per hour |
| Stone working | 400 calories per hour |
| Severe exercise, such as sawing wood | 450 calories per hour |
| Running (about 5½ miles an hour) | 500 calories per hour |
| Very severe exercise (stationary bicycle) | 600 calories per hour |
The above table, calculated for an average man weighing 154 pounds, may seem less simple to use than one based on the energy requirements per pound of body weight per hour, of an average individual. For example, a man weighing 123 pounds and performing practically the same amount and type of work as done by the man weighing 154 pounds would require practically one-fifth less calories than the latter individual. Hence, to facilitate the estimation of the food requirements for average individuals, the following table is included.[22]
| Sleeping | 0.42 calorie per hour, per lb. of body wt. |
| Sitting at rest | 0.65 calorie per hour, per lb. of body wt. |
| Light muscular exercise | 1.10 calories per hour, per lb. of body wt. |
| Active muscular exercise | 1.90 calories per hour, per lb. of body wt. |
| Severe muscular exercise | 3.00 calories per hour, per lb. of body wt. |
Possibly a few explanatory words, as to the terms used in the above tables, will assist the nurse in making the necessary calculation. “Sleeping quietly” makes allowance for no movement save that of respiration; any undue restlessness will call for an increase in the above allowance.
[Pg 46] “Sitting at rest” includes the time spent at meals, sitting in class room, ward office, studying or reading. It does not include much walking about the room, rising frequently, or nervous restlessness.
“Light exercise” includes all light house work, running an ordinary sewing machine, walking about office or ward, (receiving ward included). It does not include washing, sweeping or scrubbing.
“Active exercise” includes washing, sweeping, scrubbing, general house work, carpentry, and such sports as tennis, basket ball, and ordinary gymnasium work.
“Severe exercise” includes road workers (working with pick and shovel) fast running, baseball, football, and swimming.
“Very severe exercise” includes the work done by miners, handling of freight, and lumbermen, especially those working in extreme cold, where the severe cold makes extra demands on the fuel supply. By making use of the averages just mentioned it should be a simple matter to calculate the food requirements of any normal individual. It is necessary to know the weight of the person in question, and the manner in which the twenty-four hours are spent, and, in the case of elderly individuals, make the reductions believed to be necessary for health.
Method of Using the Tables.—Let us take a nurse in training for this purpose. Suppose the nurse weighs 110 pounds, and spends the twenty-four hours as follows,
| Sleeping | 8 hours |
| Sitting at meals | 2 hours |
| Studying | 2 hours |
| In class | 1 hour |
| On duty | 9 hours |
| Off duty (walking briskly) | 2 hours |
Her daily food requirements would probably be approximately 2,235 calories. This estimate would be increased, [Pg 47] if she were obliged to do much heavy lifting, scrubbing of beds, or other duties requiring the expenditure of much effort. It would be decreased if the hours spent in study and class room work were increased and the hours on the ward shortened. The estimation may be made as follows,
| Sleeping 8 hrs. | 110 × 0.42 × 8 | = | 370.0 calories |
| Sitting at meals 2 hrs. | 110 × 0.65 × 2 | = | 143.0 calories |
| Sitting in class 1 hr. | 110 × 0.65 × 1 | = | 71.5 calories |
| Studying, 2 hrs. | 110 × 0.65 × 2 | = | 143.0 calories |
| On duty 9 hrs. | 110 × 1.10 × 9 | = | 1089.0 calories |
| Off duty (walking briskly) 2 hrs. | 110 × 1.90 × 2 | = | 418.0 calories |
| Total for day | 2234.5 calories | ||
This estimate may be made to suit any individual, the man in the office or the one working on the streets, the woman living at home or the one spending eight or ten hours scrubbing the floors of a great office building; it is simply a matter of adjusting the calories in the dietary to meet the requirements of body weight and muscular activity.
Energy Requirements for Children.—In estimating the energy needs of children, the above method is not satisfactory, since the storage of material for growth must be considered, as well as the activities of the body. The growth period includes the years from birth to the eighteenth year, after which time the food requirements of the body are made on a basis of weight and muscular activity, as in all adults. The table on the following page shows the food allowances made for healthy children; in the feeding of malnourished or underweight children, more food in proportion to age is given in order to overcome the handicap under which they are suffering.
| Age | Calories per Day | |
| Years | Boys | Girls |
| Under 2 | 900-1200 | 900-1200 |
| 2-3 | 1000-1300 | 980-1280 |
| 3-4 | 1100-1400 | 1060-1360 |
| 4-5 | 1200-1500 | 1140-1440 |
| 5-6 | 1300-1600 | 1220-1520 |
| 6-7 | 1400-1700 | 1300-1600 |
| 7-8 | 1500-1800 | 1380-1680 |
| 8-9 | 1600-1900 | 1460-1760 |
| 9-10 | 1700-2000 | 1550-1850 |
| 10-11 | 1900-2200 | 1650-1950 |
| 11-12 | 2100-2400 | 1750-2050 |
| 12-13 | 2300-2700 | 1850-2150 |
| 13-14 | 2500-2900 | 1950-2250 |
| 14-15 | 2600-3100 | 2050-2350 |
| 15-16 | 2700-3300 | 2150-2450 |
| 16-17 | 2700-3400 | 2250-2500 |
| Years | Calories per pound, per day |
| Under 1 year | 45 |
| 1-2 | 40-43 |
| 3-4 | 37-40 |
| 4-5 | 37-40 |
| 5-6 | 35-37 |
| 6-7 | 34-35 |
| 7-8 | 32-34 |
| 8-9 | 30-35 |
| 9-10 | 30-35 |
| 10-11 | 28-32 |
| 11-12 | 28-32 |
| 12-13 | 28-32 |
| 13-14 | 25-30 |
| 14-15 | 20-25 |
| 15-16 | 20-25 |
| 16-17 | 20-25 |
After which time the food requirements are based on degree of muscular activity, boys and girls of seventeen years and over requiring as much food as men and women.
Children, like adults, differ in degrees of activity; that is, one child may be very active, running and playing more strenuously than another. Hence a margin of safety must [Pg 49] be allowed to cover the energy expenditures of the more active child, to safeguard it against becoming malnourished.
To facilitate the computation of the food requirements of children a schedule showing the number of calories per pound of body per day is included on opposite page.
The food requirements are such as to allow of a steady increase in the weight and stature of the child; the rate of gain for normal children should be as follows:
| Age Boys | Average gain, Ounces | Age Girls | Average gain, Ounces |
| First year | 3½-4½ | First year | 3½-4½ |
| Second year | 2½-3 | Second year | 2½-3 |
| Third year | 1¾-2 | Third year | 1¾-2 |
| Fourth to eighth year (inclusive) | 1¼-1½ | Fourth to eighth year (inclusive) | 1¼-1½ |
| Ninth to eleventh year (inclusive) | 1¾-2 | Ninth to twelfth year (inclusive) | 1¾-2¼ |
| Twelfth to thirteenth year (inclusive) | 2¾-3 | Thirteenth to fifteenth year (inclusive) | 2¾-3¼ |
| Fourteenth to sixteenth year (inclusive) | 3-4 | Sixteenth and seventeenth year (inclusive) | 1-2 |
The averages just given are for healthy children; those who are underweight for their age and height should show a more rapid increase in weight with an increased food allowance. It must also be remembered that a simple gain in weight is not sufficient evidence of a child’s normality; a freedom from gastro-intestinal disturbances, and a resistance to disease, are equally essential.
There have been tables arranged to show the proper weight for height for boys and girls of different ages (see appendix). These are valuable since, by their use, attention is called to the child who is not up to the average. Medical examination of such children frequently shows reason [Pg 50] for their underweight, and measures may be instituted which may save the child from a lifetime of poor health.
Dr. Pirquet has arranged a scale (Pelidisi Chart) showing the state of nutrition in children, based upon the sitting height (in centimeters), to weight (in kilograms). See appendix.
There is never a period in life in which protein is not needed. During the early years it is essential that the proteins, or at least a goodly portion of them, be obtained from animal sources, milk and eggs in particular; when cereals and legumes (beans and peas) are used to provide for the protein requirements, they must be supplemented by milk or eggs (or both), in order that the growth and development of the child may proceed at a normal rate.
Adults require protein for the repair of old tissues and to furnish material for the building of new cells, and again it is believed advisable to have at least a portion of this protein from animal sources, milk, meat or eggs.
Just as energy foods and proteins must be adjusted in the dietary to safeguard the health of the body, so the mineral salts must be adjusted for a like purpose. Studies made of the dietaries of a number of families brought to light the fact that the children more often suffered from a deficiency of calcium, phosphorus and iron in their diets than they did from too little protein,[25] proving that it is quite as essential to adjust the mineral salts in the diet as it is that of the organic constituents.
According to Sherman the diet of an adult should contain each day per pound of body weight:
| [Pg 51]Protein | 0.5000 gram or more |
| Phosphorus | 0.0100 gram or more |
| Calcium | 0.0050 gram or more |
| Iron | 0.0001 gram or more |
These averages, while covering the needs of the mature body, do not furnish the necessary amount of protein, or mineral salts to support the growth and development of the child. Hence, it has been deemed advisable to reckon the requirements of the latter per thousand calories, instead of per pound of body weight, in this way obviating some of the danger of protein and mineral deficiencies.
McCollum, Simmonds and Pitz have shown that a deficiency in the inorganic content of a diet may result in a retarding or suspension of growth. This result has been overcome on the introduction of the proper mineral salts into the diet. This salt mixture is such as to make the total ash, approximate that found in the composition of milk ash.
The following diagram illustrates this point.
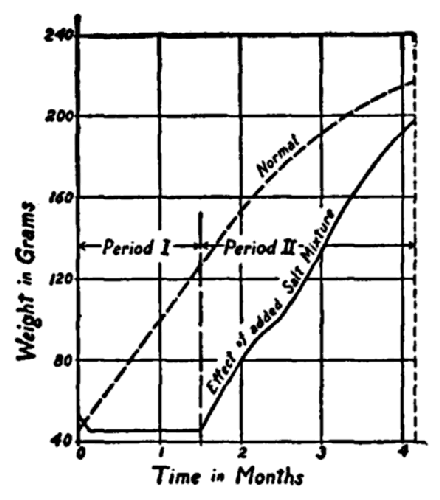
Effect upon growth of adding to a diet otherwise adequate a salt mixture of such composition as to make the composition of the total ash similar to that of milk ash; immediate resumption after entire suspension of growth. Courtesy of Dr. E. V. McCollum.
[Pg 52] The following outline will serve as a guide in making the estimates for the food requirements of children:
| Protein | 25.000 grams or more |
| Phosphorus | 00.480 gram or more |
| Calcium | 00.250 gram or more |
| Iron | 00.005 gram or more |
Vitamine Needs.—We have seen the manner in which the energy and protein foods have been adjusted in the diet, but these can not alone assure the body, and especially the growing body of a normal maintenance and repair of its tissue, or support the growth which is essential at this time. This function is believed to belong to the vitamines, since feeding experiments have demonstrated the fact that animals soon cease to grow, develop deficiency diseases, and finally die, when deprived of the essential constituents. Gillett advises, as a safe rule, the use of one, and preferably two foods known to be rich in the fat soluble vitamine, in each day’s food allowance, milk and leafy vegetables, for example. If the foods containing phosphorus, calcium, and iron are taken in sufficient quantity, the second, or “B” vitamine needs, will probably be adequately covered, but the presence of the “C” vitamine must be carefully attended to; some fresh fruit or vegetables (see table) is obligatory each day to insure the individual against the development of scurvy.
Factors Affecting the Food Selection.—The estimation of the energy needs of the body, and the selection of the foods to furnish the fuel for this purpose, depend largely upon the individual. The digestion of the fats, as well as the way in which the body utilizes them, makes the use of this foodstuff more or less limited according to the ability of the individual to take care of them, the minimum [Pg 53] allowance for children being between 2 and 3 ounces per day. According to Gillett, “If boys and girls get at least this amount from butter and its substitutes, cream, bacon, fat meat and oils, additional amounts from their food will provide a margin of safety, without overtaxing the digestive system.”
After determining the amount of fat required in each day’s food allowance, it is a simple matter to adjust the carbohydrates. It is safer from a health standpoint, to obtain the greater portion of this foodstuff from starchy foods rather than from the sugars, many foods rich in starch, likewise contain appreciable amounts of protein and fat, whereas sugar is practically one hundred per cent. carbohydrate. The ease, too, with which this substance ferments in the stomach, and the manner in which it destroys the appetite for other foods, makes the use of much of it in concentrated form unadvisable, especially in the diet of children.
The amount of sugar allowed each day, should be limited to an ounce or ounce and a half (2 to 3 tablespoonfuls), and a less quantity is desirable. In order to obtain the best results, with the least deleterious effect on the body, it is advisable to give sugar in dilute form. A piece of pure candy after a meal may not harm the child; but just before, or between meals, as well as the habit of making the breakfast cocoa and cereal of syrup-like sweetness is deplorable, and should in all instances be discouraged.
The American Red Cross recommends the following method for estimating the amount of sugar in the dietary: “Add one-half the weight of such foods as jellies, jams and preserves, and three-quarters the weight of such foods as candy, honey and syrup, to the weight of sugar used.” The amount of sugar consumed, as such, by the adult each day, is not of such paramount importance as it is in the [Pg 54] case of children, but even for adults an excessive amount of carbohydrate in this form is not considered advisable from a health standpoint.
In order to assure each member of the family of getting all of the materials needed for the growth, repair and regulation of their bodies, as well as the necessary fuel material with which to run the engine and to maintain the proper body temperature, the following practical method is suggested for the planning of the daily dietary.
1. Milk:
One quart for each child under two years of age. From 1 pint to 1 quart for each child from two to five years of age. (M. S. Rose of Teachers’ College advises at least a quart for every child of six years and under, at least 1 pint for children from six to sixteen, and one half of a pint thereafter.)
2. Cereals and Breadstuffs:
(Activity of person determining the amount.)
| For children under two years of age | 1-3 oz. a day |
| For children from two to five years | 2-5 oz. a day |
| For children from five to twelve years | 5-9 oz. a day |
| For all over twelve years of age | 9-16 oz. a day |
3. Meat or its Substitute:
For children under five years no meat is needed.
(a) Meat:
| For children from five to ten years | 1-2 oz. (no more) a day |
| For children from ten to fourteen years | 2-4 oz. (no more) a day of meat or fish. |
| For individuals over fourteen years | 2-6 oz. should be the maximum for the day. |
(b) Eggs:
| For children under two years | no eggs are given.[26] |
| For children from two to five years | 3-5 eggs may be given each week, being substituted for part or all of the meat. |
[Pg 55] (c) Beans, Peas, Cheese:
For children it is necessary to use milk abundantly when beans or peas are substituted for the meat or egg proteins.
4. Vegetables:
| For children under six months[27] | no vegetables need be given. |
| For children from six to nine months | 1 oz. gradually increased to 6 oz. of strained vegetable soup (see formula, page 223). |
| For children from twelve to fifteen months | 1 small baked potato may be added, and such vegetables as peas, string beans, carrots, spinach, squash, lima beans (strained). |
Two vegetables, one of which should be potatoes (white), should be given each day. A leafy vegetable (spinach greens, string beans, kale, lettuce) should be given from three to four times each week and oftener if possible.
5. Fruit:
| For children from six months on (earlier if physician approves) | 1-2 tablespoons orange or prune juice a day. |
| For children from first to second year | 1-3 tablespoons twice daily. |
| For children from two to five years | 3-4 tbsp. or more, twice daily (amount governed by health of child). |
All children should be given fresh fruit three or four times a week; some fruit given every day. Adults may be served dried fruit most days, but some fresh fruit should be given each week.
6. Desserts:
One sweet dish (custards, cereal puddings, junkets) once or twice a day, but little if any clear sugar should be given (cereals should be served with very little if any sugar).
7. Fats:
| For each person over five | 2-3 oz. of fat (purchased as such) a day, depending upon the age and ability of the individual to digest fats. |
[Pg 56] Suggestions for Serving Meals.—After reckoning the number of calories needed for the day, it is well to remember that the protein must be adequate in type and amount; that there should be an abundant supply of vitamines and iron in each day’s ration; that milk should always be included in order to make sure of having a sufficient amount of calcium in the diet; that there should be only one heavy protein dish at any one meal, and that it is unwise to serve a meal in which the fluids predominate on account of their deficiency in energy and proteins.
If a meal is made up of the right kind of foods, in the proper proportion, and each individual eats sufficient to assure the maintenance of the normal weight, is free from gastro-intestinal disturbances, and shows a normal resistance to disease, it is more than probable that a sufficient quantity is being consumed each day.
All foods should be carefully selected, and properly prepared in order to derive the maximum benefit therefrom, and the regularity and attractiveness with which the meals are served have almost as much to do with the health and happiness of the individual, as the character of the foods included in the day’s dietary.
(a) Calculate the dietary requirements of a nurse weighing 125 pounds, who spends 8 hours sleeping, 8 hours on duty, 2 hours at meals, 2 hours brisk walking, 2 hours in the class room, and 2 hours reading or studying.
(b) Calculate the diet for a child of ten years of age, weighing 65 pounds, showing the number of calories, the amount of protein, calcium, phosphorus and iron necessary to make this diet cover the requirements of the child.
[20] “Archives of Internal Medicine,” Vol. XXVII (1916), p. 916.
[21] “Chemistry of Food and Nutrition,” (revised), p. 186, by Henry Sherman.
[22] The Same.
[23] Gillett, A. I. C. P. of N. Y.
[24] Table compiled from material in “Feeding the Family,” by Rose.
[25] “The Adequacy and Economy of Some City Dietaries,” by Sherman and Gillett.
[26] Part of soft-cooked egg may be given at the beginning of eleventh month; this must be given at the noon meal, and should not be included in each day’s meal (two or three times a week is sufficient).
[27] Dr. Hess advises the use of canned tomato juice as a substitute for orange juice when the latter is unobtainable.
There are several methods of feeding which have been adopted to meet the needs of the individual under various conditions: Feeding by mouth, gavage or forced feeding, rectal feeding (nutrient enemata), and inunction.
Feeding by Mouth.—The first method is the one used in health and in the majority of abnormal conditions. In cases where there is a certain abnormal development of the mouth or throat, and in some cases of insanity or unconsciousness, where for some reason it is impossible for the individual to swallow, this method cannot be used.
Forced Feeding.—With very young children and babies gavage or forced feeding is found at times to be necessary. In these cases a small rubber catheter is introduced into the stomach through the nostrils and the milk or other fluid poured through the tube. In unconscious or insane patients it is often found necessary to insert a gag (a cork will serve the purpose) between the teeth to prevent the biting of the tube when it is inserted through the mouth into the stomach.
Food Used for Forced Feeding.—The food in these cases consists of reënforced soups, milk gruels, or nutrient beverages, not more than six or eight ounces given at one time. Finely chopped meat and vegetable purées have been given in this way when the digestion of the patient was not impaired, but when conditions rendered it necessary to resort to this method of feeding.
[Pg 60] Technique of Gavage.—The apparatus used in gavage consists of a moderate sized soft rubber tube to which is attached a rubber or glass funnel and a “pinch cock.” The tube should be filled with water to prevent air entering the stomach and causing pain or discomfort. In certain cases the patient refuses to swallow the tube and it will be found necessary to use some means to force the passage if the throat is shut off. By closing the nostrils the patient will be obliged to breathe through the mouth, thus opening the passage into the throat through which the tube may be quickly slipped. In certain abnormal conditions the gastric organ is so badly impaired as to render it impossible for the patient to retain food taken in by way of the mouth. It is often found that food introduced into the stomach by means of the “stomach tube” will be retained and utilized which otherwise would be rejected. It is disagreeable, however, and should only be used when it is impossible to feed otherwise.
Rectal feeding is used when the other organs of digestion are impaired to such an extent as to render the need of more food obligatory. Many investigators believe that rectal feeding is absolutely useless, while others have firm faith in its efficacy.
Technique of Rectal Feeding.—The rectum should be cleansed by flushing with a soapsuds enema one hour before the nutrient enema is given. This should be done once a day, in the morning. The cleansing enema may be either soapsuds, a solution of bicarbonate of soda, or boric acid (1 teaspoonful to the pint), or a saline solution. When there is much mucus, or if the rectum is inflamed, the soda or boric acid solution may be more soothing than the saline or soapsuds enema. After one hour’s rest the patient should be given a nutrient enema.
The method of administering nourishment through the rectum is important. A nutrient enema injected only into [Pg 61] the lower bowel not only does no good, but may actually cause a good deal of unnecessary discomfort to the patient.
Temperature of Enema.—Care must be taken not to have the temperature of the nutrient enema too hot or too cold or it will be promptly rejected. The patient is placed on the side with one knee flexed; the solution is poured into a fountain syringe bag or an enamel container (heat the container before pouring the solution into it or the latter will be chilled). The bag or container has attached to it a rubber tube with a cock adjusted so that only a small stream will flow in at a time. To the end of this tube a rubber rectal tube or catheter—1 cm. (about ½ inch)—is attached. This should be well greased (do not use glycerin as this substance is irritating to the mucous lining of the rectum). The liquid should be allowed to fill the tube before it is inserted into the rectum, to prevent any air passing in with it. The tube should be inserted with a gentle twisting movement, using very little force or the tender mucous membranes will be injured. Insert the tube twelve or more inches, since the solution is more completely absorbed if given high up in the bowel. The bag containing the solution should be held only a few inches higher than the rectum, thus allowing only a small stream to pass in and allowing an air space above the stream for the passage of gas which may be accumulated in the upper part of the rectum. The tube should be allowed to remain in the rectum for fifteen or twenty minutes, then very gently withdrawn to prevent the liquid from being rejected. A pad of gauze may be pressed against the anus to assist the patient in retaining the enema. It is well to divert the attention of the patient also, to further assist her in retaining the liquid.
Duration of Rectal Feeding.—Rectal feeding cannot be substituted for a great length of time, first, because the patient cannot absorb sufficient nourishment in this way to [Pg 62] fully cover the body requirements, and, second, because the rectum becomes more or less sensitive and will reject the liquid before it has an opportunity to be absorbed. From three to four nutrient enemas a day is about the limit for the average patient. Between the nutrient enemas it is advisable to give one of saline solution.
The following régime is practiced during the “Total Abstinence Period” in the treatment of gastric ulcer: 7 A.M., cleansing enema; 8 A.M., nutrient enema; 1 P.M., nutrient enema; 3 P.M., saline enema; 6 P.M., nutrient enema. One saline and one nutrient enema may be given during the night if the patient is very weak. She should not be wakened, however, to be given the enema.
Feeding by Inunction.—This method consists in the rubbing into the body of certain nutrient oils, such as olive oil, cocoanut oil, cocoa butter, etc. It is of little value, but is occasionally resorted to with very much emaciated and underfed infants, when digestional disorders make it impossible to introduce enough food by mouth to cover the needs of the body.
There are a number of diets formulated to meet the various normal and abnormal conditions. In hospitals these are classified as follows, for the convenience of both nurse and doctor:
House Diet.—That which is served to the hospital staff, the nurses, and those patients not requiring special diets.
Liquid or Fluid Diet.—Consisting of milk, nutrient and other palatable beverages, broths, and thin gruels.
Light, Semi-solid or Convalescent Diet.—Composed of thick or cream soups, eggs, toast, cereals, custards, jellies and ice cream, and later vegetable purées, broiled birds, chicken, lamb chops, and rare beefsteak.
[Pg 63] Mixed Diet.—The diet used in normal conditions and for those not affected by any special food.
Special Diets.—Those designed to be used for certain pathological conditions, such as scarlet fever, nephritis, etc. These diets are classified as follows:
Milk Diet.—A diet in which milk is the sole article of food.
Carbohydrate-free Diet.—One in which the sugars and starches are eliminated.
Purin-free Diet.—One in which the foods rich in purin bases are eliminated. This is used in gout, arteriosclerosis, etc.
Salt-free Diet.—Diet in which sodium chloride (salt) is as far as possible excluded. It is used in certain cases of nephritis when edema is present.
Nephritic Diet.—A diet used in nephritis and diseases complicated by nephritis (scarlet fever). In this diet the protein foods, meat in particular, are restricted, milk being the exception.
Diabetic Diet.—A diet in which the carbohydrates are restricted or eliminated.
“Allen Treatment of Diabetes” consists chiefly of “starvation” for a given period and a reëducation of the organs to a toleration for carbohydrates.
Emaciation Diets.—Those containing a high percentage of fat-forming foods, such as milk, cream, eggs, cereals, potatoes, etc., olive oil.
Obesity Diets.—Those containing as few of the fat-forming foods as possible, such as cream, olive oil, potatoes, white bread, etc., pastry and desserts, candy and soda water, and containing lean meats, fish or shellfish cooked and served without butter or other fats, fresh or stewed fruit without sugar, green vegetables and salads served without oil or other fats; one egg a day two or three times a week, coffee [Pg 64] and tea without sugar or cream, toasted gluten bread (1 slice) without butter, saccharine substituted for sugar.
There are a number of other diets, but they come more or less under the above heads.
As the patient’s tray assumes an important part of the daily régime, it is necessary to give close attention to the arrangement and serving of it. There are certain definite rules to observe: (1) The linen, silver, glassware, china, and food must be absolutely clean. (2) The tray must be sufficiently large not to appear crowded. (3) The arrangement of the obligatory articles, such as salt and pepper, silver, water glass, napkin, etc., must be alike at every meal; this not only facilitates the service by making it easy for the nurse to see whether any of these necessary articles are left off, but it also enables the patient to find them without trouble.
The Linen.—The linen cover of the tray must be clean and uncreased. The napkin likewise must be clean and unwrinkled. The china must be free from chips and cracks. Care must be taken not to put a collection of odd pieces on the tray as it gives an untidy appearance.
The Silver.—The silver must be bright and in cold weather made slightly warm, as must also the china. The chill of cold silver may readily obliterate a fragile appetite, and to place hot food in cold dishes will deprive it of much of its palatability. The foods intended to be hot must be really hot, not warm, and those which are intended to be cold should be thoroughly chilled before being served to a patient. The placing of flowers on a tray is a questionable addition to it; a single flower laid across the folded napkin may add daintiness and attractiveness, but it is poor judgment to over-decorate, either with flowers or by garnishing the dishes.
[Pg 65] Arranging the Tray.—If the nurse will place the necessary articles upon the tray and memorize their position so that she will be able to duplicate the same at each meal, she will be able to tell at a glance if everything needed is in its proper place, thereby saving herself unnecessary steps and the patient the worry of having to wait until they can be brought. Food should not be allowed to stand in the sickroom, and glasses or plates in which food has been served should be removed from sight as soon as the patient finishes with them. Care must be taken, however, not to create the impression of hurry or the patient will be made nervous and either will lose her appetite or have indigestion.
The nurse should be careful of her topics of conversation during the meal hour. Especially must disagreeable subjects and business matters be rigidly excluded if the invalid is to obtain the full benefit of the food served her.
1. Setting the Tray.—Tray should be sufficiently large not to give the appearance of being crowded, but not too large.
2. Tray cover must be spotless, and of a size to just cover the edges of tray; if too large, make a pleat down the center.
3. Place service plate directly in front of patient.
4. Knife, cutting edge in, to the right of plate; fork, tines up, to the left of plate.
5. Spoons, bowls up, next to the knife.
6. Napkin on the lower left side of tray, open edges to the lower right side.
7. Bread and butter plate on top of napkin.
8. Soup tureen in lower right corner, with cup and saucer above it.
9. Tea or coffee pot and hot water pot in upper right-hand corner of tray, with sugar bowl next to hot pot and cream pitcher next to sugar bowl.
[Pg 66] 10. Place salt and pepper next to cream pitcher (to the left).
11. Water glass in upper right corner of tray.
12. Second vegetable dish placed on the upper right side of dinner plate.
13. Place dessert to the upper left of dinner plate.
Suggestions for Serving.—Make tray as attractive as possible.
In the cases requiring special diets, the nurse should make out the “diet sheet” for the day. In hospitals this is passed to the dietitian, who carries out the directions laid down by the physician. The nurse, however, should carefully check the tray before serving it, since mistakes sometimes occur, and to give the wrong food to a patient suffering from certain disorders may give rise to serious trouble, causing pain and discomfort and at times death.
Contamination of Food.—Food should always be protected from dirt and dust and from contamination and pollution from flies and other insects. Typhoid fever and certain intestinal disturbances have been known to result from flies coming in contact with raw food—milk, for example. Poisoning due to polluted water used to freshen vegetables has already been spoken of. All of these types of poisoning may be avoided by using care in the handling of the fresh foods. Ptomaines, however, are not easy to prevent. Their source cannot always be traced to one particular article of diet. They may be present in cooked, raw, frozen, or canned foods. At times the evidence of extreme decomposition will be found in the foods themselves, while at other times there will be no such evidence in the food, but the result of the ptomaine will be perfectly evident whenever certain individuals partake of that food. This is a personal idiosyncrasy which it is impossible to account for.
Food Poisoning.—Poison caused by decomposed eggs has manifested itself in individuals who have partaken of [Pg 67] cake in which such eggs were used. Canned meat and fish have produced the most violent types of ptomaine poisoning. As a rule in these cases the canned article has begun to decompose and while the decomposition may not have advanced sufficiently far to be discernible from the flavor or odor, it is there, and if the resistance of the individual eating this food is not great, serious danger may result. Poisoning develops in some individuals upon the eating of shellfish, strawberries, oranges, pimentos, and various other foods,—another evidence of personal idiosyncrasy against certain articles of diet. There is no way to overcome these idiosyncrasies; the only thing to do is to warn the individuals so affected to let the offending foods alone.
The adulteration of food, which formerly was practised by unscrupulous dealers to cover up inferior articles, or by manufacturers to prevent or arrest decomposition in canned goods, is regulated by law. The passage of the National Pure Food and Drug Act gave the Government authority to regulate the preservatives and coloring matter used in canned and bottled goods, forcing the manufacturers to state on the label the exact contents of each bottle or can. There are likewise stringent laws governing the adulteration of milk, butter, and other articles of food.
Tests for Adulterants.—Boric acid, borax, and formaldehyde are the preservatives more often found in milk. These chemicals are introduced to arrest the natural souring and decomposition which takes place after milk reaches a certain age. Occasionally salicylic acid and sodium carbonate are used. Formaldehyde may be detected by placing about 20 c.c. of milk in a small glass vessel or tube. Dilute with an equal amount of pure water, add commercial sulphuric acid, allowing it to flow gently down the inside of the tube. A purple ring will appear at the zone of contact [Pg 68] if formaldehyde is present. “Boric acid and borax may be detected by adding a drop or two of hydrochloric acid to a few drops of milk in a white dish and then several drops of a saturated alcoholic solution of turmeric. The dish is then heated gently for a few minutes, and, if boric acid or borax is present, a pink or dark red color will appear. A dark blue-green should appear when the dish is cooled and a drop of ammonia added.”[28]
Canned goods must be carefully examined before being used. The domestic canned goods are rarely adulterated, but imperfect sterilization and defective cans may bring about a condition of fermentation and gas formation due to bacterial action. Cans should have a concave appearance on the top. If there is a bulging of the can it may be due to gas formation, and a small hole should be made in the can to note any escape of this gas. Should there be any indication of fermentation, the contents should be discarded. It is advisable to look with suspicion on cans that appear old, rusty, and soiled; they are probably left-over stock and liable to be bad. Peas which have been imperfectly sterilized produce a type of gas which is soluble in the liquid. After decomposition has occurred there will be no apparent evidence by the escape of gas, but the liquid will be found to be excessively acid, and will present a muddy appearance. Certain foreign importations of canned goods are preserved in color by the introduction of certain color preservatives. Peas—petits pois, for example—and the very small string beans which are imported are intensely green from the copper sulphate used. Its presence may be detected by adding a few drops of hydrochloric acid to some of the colored material, then dropping in a bright steel nail, knitting needle, or knife blade. There will be a deposit of copper salts (like copper plating) upon the steel if the preservative is present in the can. Canned corn is often [Pg 69] artificially sweetened with saccharine, which may be detected by shaking several tablespoonfuls of the liquid in an equal amount of chloroform. Saccharine is soluble in chloroform, while sugar is not. Allow the mixture to stand a few minutes and remove some of the chloroform which has settled at the bottom. Place in a small dish, evaporate the chloroform by gently heating the dish; taste the residue; if sweet, saccharine is present.
Coffee is adulterated more often when it is put up in ground or powdered form than when sold in the bean. Real coffee contains a small percentage of oil, and will float when thrown into a glass of water. Substitutes generally sink to the bottom. Coffee substitutes are often made up of starch-containing materials, such as cereals, beans and peas. This starch may be detected by mixing one tablespoonful of the suspected coffee in a little cold water, adding one cup of boiling water; allow it to boil two minutes, filter through cotton, and pass the liquid through charcoal to remove the color. When it is cold, add a few drops of dilute iodine solution. If starch is present, a blue color will appear.
Food is prepared for consumption by a number of methods and the method by which the food is prepared either increases or decreases its digestibility, palatability, and general usefulness.
Certain foods, as has already been stated, require a high degree of temperature to make them wholesome, but if this temperature is applied by means of heated fat, as in frying, the food is changed from a wholesome to a more or less indigestible article. In health the organs of digestion are capable of overcoming much of the harm wrought by wrong preparation, but even in the healthy, normal individual a steady diet of fried food will eventually undermine what is [Pg 70] known as good digestion. In abnormal conditions (illness) frying is a method seldom, if ever, used.
Preparation of Food.—The various methods to which food is subjected in preparation for human consumption may be summed up as follows: boiling, simmering, steaming, baking, roasting, broiling, frying, sautéing.
Boiling is cooking in water raised to the boiling point, 212° F. (sterilizing). This method is commonly used in the cooking of starchy vegetables and cereals, and in the cooking of green vegetables, such as spinach, carrots, beets, corn, asparagus, etc. Stewing is a form of boiling. As a rule water is used, and the vessel is left uncovered, so that as the food is cooked the surplus moisture evaporates, leaving the food tender. Dried fruits, such as prunes and apricots, are prepared by this method.
Simmering is cooking in water, the temperature of which is not raised to the boiling point, but kept between 200° F. and 210° F. This method is used in the preparation of eggs and dishes in which eggs predominate, since proteins are made tough if subjected to a high degree of temperature. Coddled eggs, for example, are prepared by placing the egg in a clean vessel and pouring over it the boiling water, then covering the vessel and allowing it to stand for ten or fifteen minutes. The vessel and the cold egg reduce the temperature of the water to about 185° or 190° F. and in this way prevent a toughening of the albumen of which eggs are chiefly composed. Soups, broths, ragouts, etc., are prepared by this method.
Steaming is cooking over hot water or by steam. This method may be accomplished on the top of the stove in a “double boiler” or in the oven in a deep covered pan fitted with a “rack” to hold the article to be cooked. Either method allows the vessel in which the food is placed to be surrounded by boiling water, but does not insure sufficient heat to raise the food within to the boiling point.
[Pg 71] Baking and roasting are both brought about in the oven. Bread, biscuits, pies and other pastry, potatoes, cakes, etc., are baked, while meats, roast of beef, lamb, veal, mutton, as well as chicken, turkey, duck, and large fish are roasted. The heat in the oven may be intense. The outside or cut surface of the meat is seared, the soluble albumens are coagulated, thus sealing the juices within. If the meat is placed in a pan surrounded by cold water and then placed in the oven, the juices are “drawn out” in the water. These juices contain the flavoring matter or extractives. Meat so treated is not so palatable or highly flavored as that which has first been subjected to intense heat, the water for the gravy added later.
Frying and sautéing is cooking in hot fat. Food may be fried in deep fat, as is demonstrated in the cooking of croquettes, doughnuts, etc., or it may be sautéd in butter or oil in a shallow frying pan or griddle. The latter method is used in making hashed brown potatoes, for example; also in the cooking of griddle cakes, etc.
Broiling.—In broiling or grilling the article to be cooked is exposed to direct heat, either to the blaze or to a very hot surface. The result is the same as in roasting. The outer surface is seared, sealing the juices within. Meat to be broiled is generally cut thinner than that to be roasted. The article, whether it is meat (steak), chops, birds, or chicken, is placed about three inches away from the flames and turned frequently until the surfaces are seared, after which the article is placed in a cooler part of the stove to allow the interior to be cooked. Pan broiling is done on top of the stove. The article to be broiled is placed directly upon a very hot surface, there is no grease used and the meat must be turned frequently to prevent burning.
Poaching.—This term is applied chiefly to the cooking of eggs in a shallow pan of water heated just below the boiling point. To be properly poached an egg must be [Pg 72] perfectly fresh, or the white and yolks will run together and present an unappetizing, unpalatable appearance.
The following time-table should be used in the preparation of food to insure correct cooking:
| Material | Method | Time |
| Beef (fresh) | Boiled | 4 to 6 hours |
| Corned beef | Boiled | 4 to 7 hours |
| Shoulder or leg of mutton | Boiled | 3 to 5 hours |
| Shoulder or leg of lamb | Boiled | 2 to 3 hours |
| Fowl (4 to 5 pounds) | Boiled | 2 to 4 hours |
| Chicken (3-lb. hen) | Boiled | 1 to 1½ hours |
| Ham | Boiled | 4 to 6 hours |
| Lobster | Boiled | 25 to 30 minutes |
| Salmon (whole) | Boiled | 10 to 15 minutes |
| Vegetables: | ||
| Asparagus | Boiled | 25 to 30 minutes |
| String beans | Boiled | 1 to 2 hours |
| Dried beans | Boiled | 1 to 2 hours |
| Beets (new) | Boiled | 45 minutes to 1 hour |
| Beets (old) | Boiled | 4 to 6 hours |
| Beet greens | Boiled | 1 hour or more |
| Brussels sprouts | Boiled | 15 to 20 minutes |
| Cabbage (for creamed cabbage) | Boiled | 10 to 15 minutes |
| Cabbage | Boiled | 30 to 80 minutes |
| Cauliflower | Boiled | 1 to 1½ hours |
| Celery | Boiled | 2 to 2½ hours |
| Corn (green) | Boiled | 10 to 20 minutes |
| Onions | Boiled | 45 minutes to 2 hours |
| Oyster plant (salsify) | Boiled | 45 minutes to 1 hour |
| Parsnips | Boiled | 30 to 45 minutes |
| Peas | Boiled | 20 to 60 minutes |
| Carrots | Boiled | 20 to 40 minutes |
| Potatoes (white) | Boiled | 20 to 35 minutes |
| Potatoes (sweet) | Boiled | 20 to 30 minutes |
| Rice | Boiled | 20 to 30 minutes |
| Squash | Boiled | 20 to 30 minutes |
| Spinach | Boiled | 15 to 20 minutes |
| Tomatoes (stewed) | Boiled | 20 to 30 minutes |
| Turnips | Boiled | 45 to 60 minutes |
| Coffee | Boiled | 3 to 5 minutes |
| Beef (ribs or loin, rare) per pound | Roasted | 8 to 10 minutes |
| Beef (ribs or loin, well done) per pound | Roasted | 12 to 15 minutes |
| Beef (rolled, rare) per pound | Roasted | 12 to 15 minutes |
| [Pg 73]Beef (rolled, well done) per pound | Roasted | 15 to 20 minutes |
| Leg of lamb per pound | Roasted | 10 minutes |
| Leg of mutton per pound | Roasted | 15 minutes |
| Mutton (stuffed, forequarter) per pound | Roasted | 15 to 20 minutes |
| Lamb, well done, per pound | Roasted | 15 to 18 minutes |
| Veal, well done, per pound | Roasted | 20 to 25 minutes |
| Pork, well done, per pound | Roasted | 20 minutes |
| Chicken, well done, per pound | Roasted | 15 to 20 minutes |
| Turkey (8 to 10 pounds) | Roasted | 3 hours |
| Ducks (domestic) | Roasted | 1 to 1½ hours |
| Ducks (wild) | Roasted | 20 to 30 minutes |
| Small birds | Roasted | 15 to 30 minutes |
| Large fish | Roasted | 45 minutes to 1 hour |
| Fish steaks, stuffed | Roasted | 45 minutes to 1 hour |
| Steak, 1 inch thick | Broiled | 6 to 12 minutes |
| Steak, 1½ inches to 2 inches thick | Broiled | 15 to 20 minutes |
| Lamb chop or mutton chop | Broiled | 10 to 15 minutes |
| Quail | Broiled | 12 to 20 minutes |
| Squab | Broiled | 12 to 20 minutes |
| Spring chicken (broiler) | Broiled | 20 to 40 minutes |
| Shad | Broiled | 12 to 15 minutes |
| Bluefish | Broiled | 12 to 15 minutes |
| Bread (loaf) | Baked | 45 minutes to 1 hour |
| Rolls (risen) | Baked | 20 to 25 minutes |
| Biscuits | Baked | 10 to 12 minute |
| Muffins | Baked | 20 to 25 minutes |
| Sponge cake (loaf) | Baked | 45 to 60 minutes |
| Layer cake | Baked | 20 to 25 minutes |
| Cookies | Baked | 10 to 15 minutes |
| Custards | Baked | 20 to 60 minutes |
| Steamed brown bread | Steamed | 2 to 3 hours |
| Pastry | Baked | 30 to 45 minutes |
| Potatoes | Baked | 30 minutes to 1 hour |
| Scalloped dishes | Baked | 20 minutes |
| Steamed puddings | Baked | 1 to 4 hours |
| Plum pudding | Baked | 2 hours (after steaming 10 hours) |
The ice-box plays an important rôle in the preservation of the health and comfort of the family, as well as that of the invalid. Therefore the first consideration is the [Pg 74] cleanliness of it. The old-fashioned boxes were constructed without ventilation. This was clearly a mistake, since many foods absorb both the odor and flavor of the substances about them if allowed to stand for any great length of time in a closed compartment with them. The ice-boxes or refrigerators of to-day have a ventilation system which insures a circulation of air constantly throughout the interior of the box. The drain pipes require special attention, because no matter how clean the box itself is kept, the melting of the ice causes a slime to accumulate on the inside of the pipe which will clog it and become offensive unless it is flushed out often. This may be accomplished by pouring through it a solution made by dissolving one-half ounce of borax, washing soda, or ammonia in one gallon of boiling water. The adjustable part of the pipe can be removed and cleaned with a long brush made for the purpose. The pipe is then replaced and the boiling water poured through. In this way the entire drainage system of the box is completely cleaned. All loose bits of food which may drop from the containers to the floor and shelves should be carefully removed each day and the interior of the box and shelves thoroughly wiped out. Three times a week is sufficient to wash and flush the box and pipes unless milk, cream, or other food materials have been spilled, in which case it should be washed at once before it has an opportunity to sour or spoil and become offensive. Ice should always be washed off before being put in the box, and all milk and cream bottles should likewise be wiped with a clean wet cloth before being placed on the ice.
Hot food must never be put in the ice-box, as the heat from the food will raise the temperature of the air in it. In some cases the sudden chilling of the food itself is undesirable, but this is not so often the case. However, the best results are obtained by first allowing the food to cool, [Pg 75] and then placing it on ice. This is particularly the case with jellies made from gelatin.
Milk and milk products, cream, butter, buttermilk, cheese, etc., meat, fish, and, at times, eggs should be kept in a refrigerator or in a cold place such as the cellar in the country, when it is impossible to procure ice.
Broths of all sorts, beef juice, and meat jellies will sour and decompose unless kept close to the ice. Carbonated waters, such as Vichy, Apollinaris, White Rock, etc., as well as champagne and other sparkling wines, must be kept in a dark, cool place, lying on the side. It is better to put only one or two bottles on the ice at a time, since the wine flattens (loses its sparkle) if it is ever allowed to become warm after once being placed on ice. Koumiss and other fermented milk products must be treated in a like manner to assure having them served at their best.
There are certain fundamental rules to be observed in the selection of our food materials, whether they are intended for those in health or for those suffering from pathological conditions. These rules are definite and obligatory. All food materials must be of good quality; that is, they must be of known purity and cleanliness, and adulteration should not be tolerated. In health the small amount of preservative used in certain canned and bottled foods would probably have little if any effect on the individual, but in sickness this is not always the case. With regard to milk, this point has particular significance. To obviate danger, the nurse should use discrimination in the selection of the dealer from whom the meat, milk, eggs, fruit, and vegetables are purchased, as well as the grocer who supplies the remainder of the food materials used by the patient.
The next point of consideration is the care of the food materials. This is quite as important as the selection, for even the best of food may be ruined by careless handling, not only in the preparation, but likewise during the period before it is prepared for the invalid’s consumption. The rules governing the handling of food materials before they reach the consumer are subject to inspection by law, but the housekeeper or nurse has no such rules to guard or govern her; hence she may be wantonly careless or ignorantly unsanitary unless taught the right way to care for the food in her charge. Perishable fruits and vegetables must be kept in a cool place to preserve their freshness.
Method of Washing Dishes.—Cleanliness must be observed in the care of all food materials and the utensils in which they are to be prepared. If the nurse will observe the scientific rules governing the solubility of the foodstuffs, she will be able to save herself much time and trouble. For example, it is a known scientific fact that starch is insoluble in cold water and more or less soluble in boiling water, hence it would be a useless waste of time to try to wash a utensil in which a starchy food has been cooked in cold water. Fats solidify under the influence of cold and melt under the influence of heat, so that hot water should be used in conjunction with soap or an alkali to remove grease from dishes and silver and utensils. Albumens are soluble in cold water and are coagulated in hot, therefore to remove milk, egg white, and like protein substances from glasses, spoons, etc., it is advisable to soak first in cold water to wash out the food material, and then to wash thoroughly in hot soapsuds to cleanse and polish. The dishcloths used in the washing and drying of dishes and kitchen utensils should be washed after using in hot soapsuds, rinsed in clear water, then dried in the sun. When this is impossible, they should [Pg 77] at least be hung in the fresh air to make them sweet and clean before the next using. In contagious diseases the care of the utensils and dishes used by the patient is of the utmost importance. They should be thoroughly sterilized before being placed with those used by the rest of the family, otherwise the disease may be communicated to the unaffected members. A word about the handling of glasses and spoons used in administering medicine in the sickroom: It is advisable when possible to keep these separate from those used on the tray, as many medicines have a very lasting and disagreeable taste, which is more than apt to cling to the spoons or glasses in which they are measured and in turn be communicated to the food, making it distinctly unpalatable. This has been found to be the case with asafetida, valerian, ichthyol, etc.
The metric system is a system of weights and measures expressed in the decimal scale. The principal units with which we are concerned are:
| The liter—L. | Cubic centimeter—c.c. |
| The gram—gm. | Centigram—cgm. |
| Milligram—mgm. | |
These units have prefixes to show how they are divided decimally, i.e.:
deci.—0.100
centi.—0.010
milli.—0.001
| 10 milligrams | = | 1 centigram | (cgm.) |
| 10 centigrams | = | 1 decigram | (dgm.) |
| 10 decigrams | = | 1 gram | (gm.) |
| 10 dekagrams | = | 1 hektogram | (hgm.) |
| 10 hektograms | = | 1 kilogram | (kilo.) |
| 1000 kilograms | = | 1 metric ton |
A cubic centimeter of water weighs 1 gram; 28.35 grams = 1 ounce.
[Pg 78] A liter of water weighs 1 kilogram; 1 kilogram of water = 2.2 lb.
| 4 saltspoons | = 1 tsp. | ||
| 3 tsp. | = 1 tbs. | ||
| 4 tbs. | = ¼ cup or ½ gill | ||
| 8 tbs. | = ½ cup or 1 gill | ||
| 16 tbs. | = 1 cup or ½ pint | = 8 oz. | = 227 gm. |
| 2 cups (c.) | = 1 pint | = 454 gm. | |
| 2 pints (pt.) | = 1 quart (qt.) | = a little less than 1 liter. | |
| 4 qt. | = 1 gal. | ||
| 2 tbs. butter | = 1 ounce (oz.) | ||
| 2 cups butter (solid) | = 1 pound (16 oz.) | ||
| 2 cups granulated sugar | = 1 pound | ||
| 2½ cups powdered sugar | = 16 oz. | = 1 lb. | |
| 4 cups flour (sifted) | = 16 oz. | = 1 lb. | |
| 1 pt. milk or water | = 16 oz. | = 1 lb. | |
| 1 pt. chopped meat | = 16 oz. | = 1 lb. | |
| 10 medium size eggs (with shells) | = 1 lb. | ||
| 8 eggs, without shells | = 1 lb. | ||
| 2 cups rice | = 1 lb. | ||
| 4 tbs. butter | = 2 oz. | = ¼ cup | |
| 2 tbs. sugar | = 1 oz. | ||
| 4 tbs. flour (sifted) | = 1 oz | ||
| 4 tbs. coffee (powdered) | = 1 oz. | ||
| 2 tbs. powdered lime | = 1 oz. | ||
| 2 tbs. lemon juice | = 1 oz. | ||
| 2 tbs. orange juice | = 1 oz. | ||
| 1 glass orange juice | = 8 oz. or ½ pint | ||
| 2⅔ cup oatmeal | = 1 lb. | ||
| 4¾ cup rolled oats | = 1 lb. | ||
28.35 grams = 2 tablespoons = 1 ounce of the following substances: arrowroot, barley flour, brandy, butter, grape juice, lemon juice, orange juice, molasses, cream, dry peptonoids, liquid peptonoids, milk (whole, skimmed), buttermilk, malted milk, rice flour, oatmeal, olive oil, wine.
Materials requiring 3 tablespoons to weigh 28.35 gm. or 1 oz.:—corn meal, farina, gum gluten flour, Graham flour, white flour.
Material requiring 4 tbs. to weigh 1 oz.: cocoa.
The standard measuring cup holds 8 ounces or 16 tablespoonfuls.
| 1 ordinary glass (water) | = | 8 ounces |
| 1 coffee cup | = | 8 ounces |
| 1 tea cup | = | 6 ounces |
| 1 wine glass | = | 2 ounces |
[Pg 79] The following list shows the approximate weights and measures of the foods comprising dietaries:
| Asparagus, 8 stalks, E.P. | = 2 ounces |
| Apple (1 medium size) | = 5 ounces |
| Bread, 1 slice, home-made, 4 in. × 3½ in. × ½ in. | = 1 ounce |
| Bread, 1 slice, baker’s, 4 in. × 3½ in. × ¾ in. | = 1 ounce |
| Bread, 1 slice, whole wheat, 2½ in. × 2¾ in. × ¼ in. | = .7 ounce |
| Bread, 1 slice, corn, 3 in. × 3 in. × ½ in. | = 2 ounces |
| Bread, muffin, 1 small, or biscuit | = ½ ounce |
| Banana, 1 medium size | = 5 ounces |
| Chicken, 1 serving | = 3 ounces |
| Chicken (creamed) 2 tbs. | = 1½ ounces |
| Cream, 2 tbs. | = 1 ounce |
| Custard (soft, ½ cup) | = 4½ ounces |
| Custard (baked, ½ cup) | = 4 ounces |
| Cream (ice, ½ cup) | = 4 ounces |
| Custard (rice, ½ cup) | = 3½ ounces |
| Dates (3 medium size) | = 1 ounce |
| Eggs (scrambled, ¼ cup) | = 2 ounces |
| Eggs (poached, 1 egg) | = 1½ ounces |
| Fish, medium serving, 2½ in. × 3 in. | = 2½ to 3 ounces |
| Honey, 4 tsp. | = 1 ounce |
| Hominy (cooked, ½ cup) | = 4 ounces |
| Lamb chop, E.P., 2 × 2 × ½ inch | = 1.6 ounces |
| Lemon or other jellies, ½ cup | = 3.8 ounces |
| Steak (sirloin), 3 × ½ × ¾ in. | = 3 ounces |
| Vegetables: | |
| Beets, 1 medium size (4 slices) | = 2 ounces |
| Carrots, ⅓ cup diced | = 2½ ounces |
| Peas (canned or drained), ⅓ cup | = 3 ounces |
| Potatoes, baked, sweet, 1 medium size | = 6 ounces |
| Potatoes, baked, white, 1 medium size | = 3 ounces |
| Spinach, cooked, 1 serving, ½ cup | = 4 ounces |
| Tomatoes, 1 medium size—fresh | = 3 to 4 ounces |
| Soups: | |
| Cream, ½ cup | = 4 ounces |
| Clear soup, 1 cup | = 7½ ounces |
A percentage of a number is the result obtained by taking the stated number of hundredths of it. The rate per cent. is a fraction whose denominator is 100 and whose numerator is the given number of hundredths; thus 6% of a number is 6/100 of that number.
The method of figuring the per cent. of foodstuffs in a [Pg 80] food material is simple. Milk, for example, has a percentage composition of 3% protein, 4% fat, and 5% sugar. To find the definite amounts of these foodstuffs in 1 ounce of milk it is best to reduce the ounce to grams, since the gram is the unit of measurement generally used.
| 1 ounce | = | 28.35 grams |
| In 1 oz. there will be 28.35 × .03 | = | 0.85 gram protein |
| In 1 oz. there will be 28.35 × .04 | = | 1.13 grams fat |
| In 1 oz. there will be 28.35 × .05 | = | 1.41 grams sugar |
There are two scales used in thermometry, the Fahrenheit and the Centigrade. The former is generally used. However, since many of the scientific calculations are made using the Centigrade scale it is wise for the nurse to understand how to translate one to the other.
Centigrade has 0° as the freezing point and 100° as the boiling point, while Fahrenheit has 32° as freezing point and 212° as boiling point. To change Fahrenheit to Centigrade it is necessary to subtract 32 from 212 in order to make the freezing points correspond. This would read 212 -32 = 180° F. = 100° C; hence a degree Centigrade represents 5/9 of a degree Fahrenheit.
To change Centigrade to Fahrenheit it is necessary to remember that every Fahrenheit degree is 9/5 times as large as the Centigrade and the addition of 32° must also be made. For example: Change 105° F. to Centigrade: 105°-32° × 5/9 = 41° C. Change 50° C. to Fahrenheit: 50° × 9/5 + 32° = 90° + 32° = 122° F.
[28] “Diseases of Nutrition and Infant Feeding,” by Morse and Talbot.
Dairy Products.—Milk, cream, and other dairy products form such an important part of the invalid dietary that they require especial care in their selection. “Certified Milk” is the safest. This is protected by special inspection. The methods and standards governing the production and distribution of certified milk were adopted by the American Association of Medical Milk Commissions, May 1, 1912. The sanitary condition of the dairy, the cleanliness of the vessels into which the milk is placed, the health of the milkers, and a surety that no member of their family with whom they come in contact has any kind of contagious disease, are all obligatory. The feed for the cows and the purity of the water given them to drink must be inspected and made to conform to the standard laid down for certified milk. The milk of sick cows and those having tuberculosis is absolutely condemned. The composition of certified milk is standardized as follows: the fat standard shall be 4%, with a permissible range varying from 3.5% to 4.5%. The proteins shall be 3.5%, with a permissible range varying from 3% to 4%. Certified milk shall not contain more than 10,000 bacteria to the cubic centimeter when it is delivered. This inspection and standardizing necessarily raises the price of certified milk above that of milk not so rigidly cared for, and when the additional expense makes it impossible for the patient to afford certified milk, the only thing to do is to be sure of the reliability of the dealer from whom the milk is purchased and the cleanliness of the dairy from which it is procured. Buttermilk [Pg 82] and butter are the milk products which require some attention as to selection. The former grows sour with age and the odor of advanced fermentation and decomposition is readily recognized. Sweet butter, butter without salt, is less apt to be old when purchased than the salted variety, as the flavor of rancid fat is unmistakable in butter which has not been especially treated.
Milk.—Milk is without a doubt the most valuable food in the invalid dietary, furnishing not only a highly nutritious beverage, but likewise acting as a carrier of additional nourishment when such is necessary. Its form, its lack of definite flavor and odor, all add to its value as a food in sickness. Milk is one of the few foods which includes in its composition all of the chemical combinations known as foodstuffs. The carbohydrates, comprising 4.88% to 5% of the solids in milk, occur as lactose or milk sugar. This sugar belongs to the disaccharide group, and is, in the majority of cases, readily digested by even the most delicate digestive apparatus. This form of sugar lends itself particularly well as a reinforcing agent, and is generally used in such cases as typhoid fever, etc. The fat in milk, comprising 4% of the solids and occurring as butter fat (cream), is made up chiefly of olein and of palmitin, with smaller amounts of stearin and from 5% to 6% of its composition in the form of butyric acid (the fatty acid to which butter owes its name and flavor) and traces of other fatty acids, as well as small quantities of cholesterin, lecithin, and a yellow coloring matter.
The proteins of milk, which form the curd or larger part of the solids, according to Van Slyke[29] are in the form of casein and albumen. There are 3.6 parts casein to 1 part soluble proteins, but these figures vary somewhat at times. Casein is insoluble in pure water, but dissolves readily in water to which an alkali or calcium carbonate is added. The [Pg 83] soluble protein in the form of lactalbumen is one of the constituents of whey. This substance contains more sulphur than does casein, but no phosphorus.
Whey is the opalescent fluid which remains when the casein is precipitated, and is composed of water 93.8%, total ash 0.44% (König).
Mineral salts, 0.7% of milk, are made up of calcium, potassium, sodium, magnesium, iron, sulphur, phosphorus, and chlorine. Milk is so rich in calcium that it requires only 400 c.c. (or about 2½ cups) to furnish 1 gram of calcium. This is the amount believed to be necessary for the welfare of man each day and this must be derived from food.[30]
Water.—The fluid part of milk is composed chiefly of water, constituting 87% of whole milk.
Milk as a food for infants will be discussed in another chapter.
As has already been said, no food has so far been discovered which could be effectually substituted for milk. There is no food, however, which requires more attention in its selection and care. It is very susceptible to both odors and flavors, absorbing them both readily, as will be found if milk be placed in the same compartment with foods of strong odor and flavor, without being properly covered and protected. This is particularly noticeable with cucumbers, melons, etc.
Milk also furnishes a splendid medium for bacterial growth, and if left exposed to the air, put into unclean receptacles, or kept in a warm place, will immediately become more or less contaminated, after which it is unwise to use it. Sterilization and pasteurization will in a measure overcome the bacterial contamination, but milk purchased from a dairy which is not clean or milked under unsanitary conditions will remain dirty, hence unfit for [Pg 84] human consumption. When the morning’s milk supply is brought to the house it should be in clean, well-stoppered bottles, but before placing it in the ice-box the tops of the bottles should be carefully wiped off with a wet cloth to remove any superficial dust which may be adhering to them. Every time a portion of the milk is removed thereafter the tops should be again cleansed before the milk is poured out. This is a wise precaution, and often prevents contamination from the hands, etc.
The amount of water in milk prevents its being an adequate food for adults except in certain pathological conditions. However, it furnishes a supplementary food unequaled by any other beverage known. There are fortunately only a few individuals who are unable to drink milk. There are many who fancy they cannot do so, but if the nurse has the ingenuity to utilize some of the various methods whereby milk is made more digestible, it will generally be found that the patient can take it without trouble. In cases of personal dislike, if the milk is flavored or colored or made up into soup, cocoa, chocolate, junket, custards, blanc-mange, etc., it will usually prove acceptable.
Application of Heat.—A word as to the changes which are brought about as the result of heat as applied to milk. These changes are demonstrated in the two methods commonly used in the preparation of milk known as “pasteurization” and “sterilization.” Pasteurization is rather an indefinite term to use, unless the time and the temperature to which the milk is subjected are given. According to Morse and Talbot “the term sterilization should never be applied to the processes used in the preparation of milk for the feeding of infants, because the milk is never rendered bacteriologically sterile by them.”[31]
As a rule the flavor and odor of milk are not changed by heat until the temperature reaches nearly to the boiling [Pg 85] point. A scum then forms on boiling milk, composed of casein 50.86%, fatty matter 45.42%, ash 4.72% (Rosenau). Prolonged boiling changes the color of milk from a creamy white to a yellowish brown which deepens with boiling. This is due to the caramelization of the milk sugar. Cream will not rise (or its rise will be very slow) on milk which has been subjected to a temperature of 150° F. for thirty minutes or more because the fat droplets are broken down so that they cannot hold together at that temperature and become more completely distributed throughout the fluid.[32]
Pasteurization is acknowledged to be preferable to sterilization in milk used for infant feeding because the higher the temperature the greater the change in the chemical composition of the fluid. According to Morse and Talbot[33] the temperature of the pasteurization should be as low as possible. Pasteurization at 140° F. for 20 minutes is sufficient; lower temperatures are not. “At this temperature there is no change in the taste, odor, or color of the milk, no noteworthy changes in the chemical composition are produced, the ferments and bactericidal action are unaffected and bacterial toxins and non-spore-bearing microorganisms are destroyed.”[34]
Rosenau[35] states that the bacillus of typhoid, diphtheria, and dysentery, as well as the cholera vibrio and other pathogenic non-spore-bearing bacteria which are often found in milk, are destroyed at a temperature of 140° F. for twenty minutes, and at higher temperatures for shorter lengths of time.
Sommerfield’s[36] investigations prove that butyric acid [Pg 86] bacilli are destroyed at a temperature of 212° F. for from 1 to 2 minutes.
It must be understood that no matter what method is used to insure purity in milk, nothing does away with the necessity for keeping the milk both clean and cold. The receptacles in which the milk is allowed to stand, the vessels in which it is measured, and the person who handles it must be absolutely clean, and the nurse must keep in mind the fact that pasteurization does not completely destroy the bacterial growth in milk, that it merely diminishes it, and she must see that the milk which has undergone the pasteurizing process is kept cold, otherwise the microörganisms which are present, even if to a less extent than in raw milk, will undoubtedly multiply.
Adulteration of Milk.—There is not nearly so much adulteration of milk to-day as there was a few years ago. The stringent laws governing the care and composition of the milk make it unprofitable for the dairymen to practise it. However, there are times when such things are done and care must be taken to prevent it. Milk is, as has already been stated, very susceptible to contamination, and that which is infected with putrefactive bacteria is not fit for food even if the dealer has doctored it with formaldehyde. However, the danger to-day is not so much from drugs as from lack of care in the handling of the milk. It is well to remember, however, that water is an adulteration just the same as formaldehyde and perhaps more pernicious, since the quantities of the latter are so small in an ordinary quantity of milk as not to make a great deal of difference except in the feeding of invalids and children, while watered milk is a swindle not only to the pocketbook but to the body also, since the requisite nutritive value is lacking.
Selection and Care of Milk.—There are a few essential facts to keep in mind in regard to milk: (1) Be sure of the source of the milk supply, especially in the feeding [Pg 87] of the sick and of infants. Milk for such cases should always be purchased from inspected dairies when it is possible. (2) Keep the milk cold; the best milk in the world will spoil if left in a warm place. (3) Always keep the milk bottle well covered, thus eliminating the danger of contamination, flies, etc.
135-152 calories
| 6 ounces (¾ glass) fresh whole milk. | 1-2 eggs (whites only). |
Have the milk thoroughly chilled.
Clip egg whites with scissors and strain through cheesecloth to remove stringy parts. Now stir into the milk with a fork.
If patient does not object to foam, the mixture may be placed in a milk shaker with pieces of ice and shaken until creamy, then poured over cracked ice.
135 calories
| 6 oz. (¾ glassful) fresh whole milk | 1 egg white |
Place the milk on ice to become thoroughly chilled. Clip the egg white with scissors and strain through cheesecloth to free it from strings; stir into cold milk. If patient does not object to foam, the milk and egg whites may be placed in a milk shaker, and agitated for 4 or 5 minutes, then poured over cracked ice. This beverage may be flavored to suit the taste of patient. Vanilla, caramel, or coffee may be used to give variety.
To add additional nourishment 1 teaspoonful of Sanatogen, or Plasmon may be added, or 1 tablespoonful of Panopepton or liquid peptonoids used instead of the casein products.
59 calories
| 3 oz. milk | 3 oz. ginger ale or sarsaparilla |
Pour into a milk shaker and shake with cracked ice until foamy.
298 calories
| 4 oz. rich milk | 1 tbs. whisky (or sherry) |
| 2 oz. cream | 1 tbs. sugar (or less) |
| 1 egg white (if additional nourishment is desired) | |
A grating of nutmeg on top. Place ingredients in shaker as directed above, and shake a few minutes to thoroughly mix ingredients. Pour over cracked ice, grate nutmeg or cinnamon over the top. The milk may be peptonized if necessary, using ½ tube of Fairchild’s peptonizing powder.
314 calories
| 1 pt. of milk | 1 tube of (Fairchild’s) peptonizing powder |
Dissolve the powder in 1 gill of cold water, and place in a clean quart jar (glass).
Pour in 1 pint of cold milk and stop the bottle with cotton, shake well and place the bottle in a saucepan containing water just warm enough to allow of the hand being immersed without being burned (115° F.).
Keep the water at this temperature for 5 to 10 minutes or longer according to the degree of peptonization desired. Lift out of the warm water and plunge into cold, then place at once on ice.
The milk may be poured from bottle into a clean saucepan and brought quickly to a boil to prevent further peptonization; this process, however, is apt to make the milk [Pg 89] very bitter and should not be used unless it is to be flavored with fruit juice.
212 calories
Take a goblet about one-third full of finely crushed ice, add a tablespoonful of St. Croix rum, a dash of curaçao or any liquor that is agreeable to the taste; fill the glass with “specially peptonized milk,” stir well, and grate a little nutmeg on top. Add 1 tablespoon sugar.
627 calories
| 1 qt. fresh whole milk (or skimmed if desired) | 1½ to 2 oz. (Bulgarian) starter, or 1 buttermilk tablet[37] |
If latter is used dissolve tablet in 1 gill of cold water.
Stir the buttermilk starter into the cold milk and place in a one-half gallon glass jar, place the cover on loosely and allow the jar to stand for 12 hours or until the milk is well clabbered. (Insert a thin-bladed knife close to the jar so that the rest of the milk is not disturbed to see if the coagulation is complete.) When this is accomplished place the jar in the ice-box. After the milk has become thoroughly cold, beat thoroughly. The mixture is like any well-made buttermilk. If the cream is removed before adding the culture the milk will be lower nutrient value, but in many cases this is necessary since it is often the fats which cause a disturbance.
147-166 calories
| 2 tsp. cocoa | ½ cup boiling water |
| 1-2 tsp. sugar | ⅔ cup milk |
[Pg 90] Mix cocoa and sugar together and add boiling water slowly. Boil 3 to 5 minutes; heat milk in double boiler and add cocoa mixture. Beat with Dover egg beater to distribute cocoa and prevent scum forming. Serve with or without whipped cream. Cocoa may be reinforced as directed in “broths” with albumen or the whole or yolk of one egg well beaten. If the white alone is used, care must be observed that the liquid is not hot enough to coagulate the albumen. Proprietary foods and casein preparations are used in like manner.
161 calories
| ⅔ cup milk | ¼ tsp. vanilla extract or a grating of nutmeg |
| ½ junket tablet | 1 tbs. sugar |
Heat milk to 100° F. Add junket tablet dissolved in 1 tbs. cold water. Mix in sugar and flavoring, and pour into molds to jelly. When junket becomes firm, place in ice until needed.
428 calories
| ½ cup each cream and rich milk | 2 tbs. sugar |
| 1 junket tablet | ½ tsp. vanilla |
Heat cream and milk to 100° F. and proceed as in junket. When mixture is jellied turn into freezer, as any ice cream. This is the most wholesome of ice creams and especially suited for children and patients who have tuberculosis complicated with gastric disturbances.[38]
585-602 calories
| 1 cup thin cream | ½ tsp. vanilla, lemon extract, or almond extract |
| 2 tbs. sugar (more if desired) | |
Method I. Whip cream, add sugar and flavoring, and freeze.
Method II. Scald half the cream and cool. Whip the remaining half, add sugar and flavor and freeze.
Method III. Make “boiled custard,” as directed, add one-half the amount of cream and freeze.
To reënforce ice cream:—Add 1 or 2 egg whites, beaten or unbeaten; these may be added in the beginning, or after the mixture begins to freeze. A tablespoonful of maple sirup, caramel sirup (1 tbs. sugar melted and browned and dissolved in 1 tbs. boiling water), or chocolate sirup may be poured over the ice cream to vary the flavor. Make chocolate sirup by boiling 2 tbs. water, 1 tbs. sugar, and 1 tbs. chocolate to a sirup. 143.3 calories.
289-329 calories
| 1 egg (or 2 yolks) | 1 cup of milk |
| 1 tbs. sugar | Few drops of vanilla |
| ⅛ tsp. salt | |
Prepare as soft custard, freeze.
627 calories
| 1 qt. fresh milk | 1 gill cold water |
| 1 lactone tablet (or 1½ oz. buttermilk starter) | |
(Parke, Davis & Co.’s and Hanson & Co.’s buttermilk tablets are practically the same.)
[Pg 92] Dissolve tablet in cold water and stir into fresh milk (which may or may not be skimmed, according to the directions of the physician, but the finished product is more palatable using whole milk). Pour into a clean jar or wide-mouthed bottle; plug with cotton or close not tightly, allow to stand in room temperature 70°-75° F. 24 hours, shaking the bottle occasionally to keep the cream from rising. At the end of this time pour the milk out (if sufficiently fermented), and beat briskly for 5 to 6 minutes with egg beater or with churn; place on ice until ready to serve.
77-96 calories
| 1 tbs. malted milk | 6 oz. boiling water |
| 1-2 tsp. sugar | ¼ tsp. salt |
| 3 to 5 drops vanilla | |
Heat water to boiling and mix malted milk (Horlick’s) with a little cold water. Stir into the boiling water, add sugar and salt, and serve with or without cream.
107-155 calories
| ½ to 1 tbs. malted milk | 1-2 tsp. sugar |
| 3 oz. each milk and water | ¼ tsp. salt |
Proceed as above.
230-300 calories
| 1 tbs. malted milk | 2 oz. water |
| 1 tbs. cocoa or grated chocolate | 1-2 tsp. sugar |
| 6 oz. milk | 4-5 drops vanilla extract |
Mix cocoa or chocolate with water and boil 2-3 minutes. Pour milk into a double boiler and heat, mix malted milk with a little water and stir into the hot milk, add the cocoa [Pg 93] paste, sugar, and vanilla, mix thoroughly, beat the mixture briskly to mix ingredients thoroughly, and serve with or without cream.
599-1229 calories
| 2 tbs. flour | 1 pt. milk or thin cream |
| 2 tbs. butter | ½ tsp. salt |
Cream butter and flour to a smooth paste, heat milk in double boiler on an asbestos mat over the flame; when it is scalding hot, stir in the butter and flour paste, stir until smooth and the mixture begins to thicken, cover and allow to cook without boiling for 15 minutes; strain. The sauce may be used at once or put into a glass jar in the ice-box until needed.
213 calories
| ⅔ cup cream sauce | ⅓ cup asparagus purée |
Heat sauce and purée in separate saucepans, and when about ready to serve, stir them together, strain carefully, season with salt, and serve with or without croutons of toast or whipped cream. If the sauce is made from the cream instead of milk, the fuel value will be much higher (302.7 calories).
216 calories
| 8 medium stalks of asparagus | 1 tsp. salt |
| 1 qt. water | 1 tbs. flour |
| ½ cup cream sauce | |
Cut off the tips of the asparagus in 1-inch pieces, and place with the rest in a saucepan, and cover with water; [Pg 94] add salt and cook until the tips are tender; lift out and put aside to be used instead of the toast croutons. After the water in which the asparagus is cooked is of sufficiently strong flavor, strain and add the extra spoonful of flour, mixed in a tablespoonful of water; cook 15 minutes, measure ½ cupful, and proceed as directed above.
259 calories
Boil and cream the potato. Make sauce and add potato purée; stir until well blended and serve with toast croutons.
When boiling potato if a sprig of parsley is added and strained out, and a little of the potato water is used to make the purée smooth, the soup will have more character.
224-461 calories
| ¾ cup cream sauce | ⅓ cup vegetable purée |
Proceed as in making other cream soups.
179 calories
| 6 oysters | ¾ cup milk |
| 1 cracker (soda) or 8 oyster crackers | ¼ tsp. salt |
| A dash of pepper | |
Put oysters (and their liquor) into a saucepan, and heat gently; skim thoroughly. Heat milk in separate pan; when very hot add to oysters. Roll the cracker and add to soup just before it is served. Add salt and pepper at the same time.
Eggs.—The table shows eggs to have a chemical composition of water 73.7%, protein 14.8%, fat 10.5%, and mineral salts (ash) 1.0%. Fuel value per pound, 672 calories. The white of the egg, constituting 57% of the entire weight, is composed chiefly of albumen and water with a small percentage of mineral salts in the form of calcium, potassium, magnesium, sodium, phosphorus, chlorin, sulphur, and iron. Typical albumens are always rich in sulphur, and in eggs the sulphur content is much greater in the egg white than it is in the yolk. The yolk of eggs contains more protein and fat than the white, and less water. The protein of the yolk is chiefly in the form of ovovitellin, while the fats occur as palmitin, olein, and stearin. There is also 5% of coloring matter in the yolk of eggs besides lecithin, nuclein, salts of iron, potassium, magnesium, and phosphorus. The latter mineral salt comprises 1.0% in yolk, while in the white there is only .03%. Eggs have a position in the invalid dietary second only to that of milk. They are nutritious, easy of digestion, and exceedingly palatable if properly selected and correctly prepared. The albumen in the white is very susceptible to the effect of heat. At a temperature of about 135° F. the clear, pale yellowish white begins to change to an opalescent tint, and, as the temperature is gradually increased, the texture changes from a viscid, sticky substance to an opaque, jelly-like mass which solidifies with an ever increasing temperature. Hard cooked white of egg, unless it is very finely divided, is considered difficult of digestion, but if the heat is applied gradually and is not raised to the boiling point (212° F.) there is no reason why the hard cooked white of the egg should not be digested. However, it is unwise to cook eggs in this manner for invalids or children. Any of the other methods, with the exception of frying, which [Pg 96] should never be used, is decidedly preferable. Egg albumen is soluble in water and fresh fruit juices, so that it may be used with great success as a reinforcing agent. In fact, the whole egg may be so used, but it is more difficult to disguise the yolk in a beverage than it is the white, and for this reason it is not so adaptable in many cases. Eggs may be cooked by the following methods in the invalid dietary: coddled, soft-cooked, poached, creamed, omelet, scrambled, or in custard. Uncooked eggs may be given in water, milk, wine, or fruit juices.
The selection of eggs is equally as important as the selection of other foods. There are “new-laid eggs,” “fresh eggs,” and just “eggs.” The latter are generally storage and should not be used for the sick or for infants. As a rule old eggs will not stand poaching, the whites and yolks mingle and form an unappetizing mass. It does not make any difference whether the color of the shell is white or brown; if the egg is absolutely fresh the white and yolk should be distinct and easily separated, and when they are not it is safer to discard the egg entirely.
118 calories
| Juice of 1 orange | Juice of ½ lemon |
| 1 tbs. sugar | Enough water to fill the glass |
Sweeten the juice of orange and lemon and pour into a glass filled with crushed ice. Fill glass with plain or carbonated water.
152 calories
Make orangeade as directed in above recipe, without the addition of water. Break the whites of 2 eggs into a saucer [Pg 97] and with scissors cut the albumen until free from membrane and strain, stir this into the orange juice and add several pieces of cracked ice. This is both nourishing and palatable, and the taste of the egg cannot be detected.
107 calories
| Juice of 1 lemon | 1 tbs. sugar |
| Whites of 2 eggs | |
Cut as directed for Albuminized Orangeade. Mix until sugar is dissolved. Pour over a glassful of cracked ice. Fill glass with plain or carbonated water.
151 calories
| 2 oz. (¼ cup) grated pineapple | Juice of 1 lemon |
| 8 oz. (1 cup) cold water, or sufficient quantity carbonated water to fill glass | |
| 1 drop of lemon extract or a little of the peel, grated | 1 tbs. sugar |
Mix lemon juice, water, and pineapple together; add sugar, if not sweet enough, but the less used the better, in all beverages. Add extract and pour into a shaker with a few lumps of ice. Shake well to mix ingredients and pour the pineapple over crushed ice. If this proves too much at a time, make half the recipe. Serve in tall thin glasses holding from 4 to 6 ounces after the ice is put in, or serve in punch glasses with small spoons.
Albuminized Grape Juice is made without the addition of lemon juice unless the white grape juice is substituted for the black, in which case add one or two teaspoonfuls to relieve the flat taste and proceed as in Albuminized Orangeade, using 3 oz. of grape juice.
57 calories
| 1 egg | 1 tsp. lemon juice |
| 2 tsp. sugar | Several sprigs of fresh spearmint |
Whip white of egg; add sugar and lemon juice. Crush lower parts of mint leaves slightly and place in glass. Pour mixture over ice in glass; stir well and serve at once.
Fill glass with carbonated water, Vichy, White Rock, Apollinaris, etc. This is especially good when patient suffers from nausea.
232 calories
| 1 egg white | 3 oz. (6 tbs.) cream |
| 2 tsp. sugar | A few drops of vanilla extract |
| Celestine (French) Vichy to fill glass | |
Whip egg white to stiff froth; whip cream stiff and sweeten, add vanilla; lastly, the egg. Pour over cracked ice and fill up the glass with Vichy.
| 2 tbs. ground coffee | 1 cup boiling water |
| 2 tsp. white of egg | ¼ cup cold (boiled) water |
Mix coffee with 1 tablespoonful of cold water and egg white in small pot (after scalding pot), add boiling water; allow to boil 3 minutes; stir down and add cold water; set pot where coffee will stay hot, but not boil, for 10 to 15 minutes, serve with cream and sugar or use to flavor hot milk.
267 calories
| 1 egg | 1 tbs. rum |
| 2 tbs. cream | 1 tbs. whisky |
| 1 tbs. sugar | |
Beat yolk of egg and sugar together; add cream, rum, and whisky. Beat egg white stiff and stir into the mixture; pour into glass with or without cracked ice.
Nutmeg may be grated over top for those who like it.
Follow recipe for plain eggnog, substituting 2 tablespoonfuls of strong coffee for the rum.
233-257 calories
Is made as directed for plain eggnog, panopepton being substituted for the rum, using 1 ounce instead of 1 tablespoonful. This will probably more than fill a glass, but the whole amount must be made to keep the proportions correct. The whisky may be left in, if desired, or sherry wine may be substituted in its place to give flavor and additional stimulation.
264-316 calories
| 1 egg | 1 tbs. sherry wine or whisky |
| 1 tbs. malted milk | ½-1 tbs. sugar |
| 4 oz. milk | 1 tsp. cream |
Mix milk as directed above and chill thoroughly. Beat egg yolk with sugar and whisky or wine and add to the mixture. Beat egg white stiff and stir into the rest of the [Pg 100] ingredients. Pour into shaker and shake with cracked ice until thoroughly chilled. The cream may be served on top, or beaten into the eggnog.
130 calories
| 1 egg | ½ tbs. butter |
| 1 tbs. water | ⅛ tsp. salt and dash of pepper |
Beat yolk until light colored and thick; add water, salt, and pepper. Beat white until stiff and dry. Turn the yolk over the beaten white and cut and fold the white into the yolk mixture.
Have pan hot and buttered, turn in the mixture, spread evenly in pan and allow to stand about two minutes on the top of the stove at a moderate heat; then remove the pan, place in a moderate oven and cook until a knife thrust into the center comes out nearly clean. Remove from oven, cut across center at right angles with handle of pan and turn over on a hot platter. Omelets may be varied by the use of different garnishes and flavors.
75 calories
| 1 pt. water | 1 egg |
Allow water to boil; wash egg; drop into boiling water and place saucepan where water will keep hot, but not boil; allow to stand 7 to 8 minutes. Serve with salt.
75 calories
Proceed as for coddled eggs, but allow egg to remain from 10 to 15 minutes or even longer, if very soft eggs are not desired.
75 calories
Have small, shallow saucepan half filled with boiling water or milk—if an egg poacher is at hand, use that; otherwise, lower a flat perforated spoon into water and place where the water cannot boil. Break the egg carefully into the spoon, taking care not to break the yolk; allow to stand in hot water until the white is of the consistency of jelly; lift out—slide egg on to hot toast, taking care not to break. (A broken poached egg is very unappetizing, as well as untidy in appearance.)
With milk 131 calories
With cream 170 calories
Cut the crust from one slice of bread and cut bread in one-inch cubes; toast while preparing egg. Beat egg with egg beater until light colored; stir into it 2 tablespoonfuls of rich milk; pour into a double boiler, over hot water; add 1 teaspoonful butter, a little salt and pepper; stir until like thick boiled custard. Pour over toasted cubes of bread and serve at once.
204 calories
| 1 egg | 1 slice of bread (¾ in. thick) |
| ½ tbs. butter | Salt and pepper to taste |
Toast the bread on one side, butter and place on a plate (one which will not break in the oven).
Beat egg white stiff, and pile roughly upon the toast, leaving a slight depression in the center. Slip the unbroken yolk into the depression (take care not to break the egg yolk or the appearance and significance of the dish will be [Pg 102] ruined). Set plate in oven to brown the white (the oven must not be too hot or the white will brown before the yolk is sufficiently cooked to be palatable). Place the remaining butter on the yolk, dust with salt and pepper and serve at once.
289 to 329 calories
| 1 egg (or 2 yolks) | 1 cup milk |
| 1 tbs. sugar | A few drops of vanilla |
Heat milk in double boiler. Beat egg and sugar together. When milk has reached the scalding point (small bubbles form around the edge of the saucepan), stir in the egg. Care must be taken not to allow the water under the saucepan to become too hot, as the custard will curdle if the egg is cooked at too high a degree of temperature. The custard must be stirred constantly in the beginning until it begins to thicken, then several times a minute until it is of the desired consistency and the raw taste is cooked out of the egg. This mixture is done when it will form a coating upon the spoon. Serve with whipped cream on top (57 calories extra with cream).
249 calories
| 1 egg | ¾ cup milk |
| 1 tbs. sugar | A few drops of vanilla |
Beat egg and sugar together, stir into the milk, grease custard cup with butter, pour in the mixture. Set cup on several layers of paper in a deep pan, surround with hot water (to about half its depth). Set pan in moderate oven and allow to cook slowly until custard is firm in the center. It may be served hot or chilled and turned out, with a tablespoonful of whipped cream on top.
[Pg 103] Care must be taken not to allow the oven to get hot, or the egg will coagulate, making a watery, unpalatable, and indigestible mixture.
306 calories
Caramel custard is made exactly the same as baked custard, except that the cup is lined with a caramel made as follows: In a small frying pan, place 1 tablespoonful of sugar, place on the stove and stir constantly until it melts and turns a golden brown (do not allow to burn). Fold a cloth about the custard cup and pour in the caramel, moving the cup about until the sides and bottom are well coated. Pour in the custard mixture and proceed as in baked custard.
381 calories
| 1 egg and 1 extra yolk | 2 lady fingers |
| 1 cup milk | Few drops vanilla |
| 1 tbs. sugar | |
Make soft custard, using the two yolks (no white). Chill custard thoroughly. Line individual ice cream cup with the lady fingers; pour the custard over. Beat the white of egg and place on top. Serve at once. The lady fingers may be dipped in sherry wine if desired, using about 2 tablespoonfuls of wine. (26 calories extra.)
101 calories
| 2 tbs. corn meal | 1 cup water |
| ½ tsp. salt | |
[Pg 104] Allow water to boil, mix corn meal with 3 or 4 teaspoonfuls of cold water. As soon as water begins to boil, stir briskly until gruel begins to thicken. Then place on a cooler part of the stove, and cook gently for 2 hours, replacing water as it evaporates. Strain through a coarse sieve if it lumps.
183 calories
| 3 tbs. (1 oz.) farina | ½ cup boiling water |
| ½ cup rich milk | ¼ cup cold water |
| ¼ tsp. salt | |
Mix farina into a paste with cold water. Stir into boiling water, allow to cook for half an hour (if water boils out, add boiling water). Add milk, and place the saucepan in a hot water bath (double boiler); allow to cook half an hour longer, stirring occasionally.
99 calories
| 2 tbs. (1 oz.) rice | 1 pt. boiling water |
| ½ tsp. salt | |
Soak rice for 1 hour in cold water. Sprinkle into the briskly boiling water, taking care not to stop the boil. Allow to cook until tender; test by pressing a grain between thumb and finger; there should be no hard center. When the rice is done, turn it into a colander and allow water from cold faucet to run over it to wash off surplus starch. Return to saucepan place on stove where moisture can be dried out of the rice without burning it.
2-3 servings, 316 calories
| 4 tbs. rice | ¾ cup water |
| ¼ tsp. salt | ¾ cup milk |
[Pg 105] Wash rice and soak it in cold water for 1 hour (or overnight). Place in an earthenware baking dish, cover with the milk, water and salt. Cover and set in the oven; allow to cook until all of the moisture is absorbed (if the rice is not done by the time the moisture has evaporated, add more milk, or milk and water, and continue until the grains are tender). If the given amount of moisture is not absorbed by the time the rice is tender, drain off the surplus and return the dish to the oven for a few moments. Each grain should be separate, when the dish is prepared correctly.
149 calories
| 1 slice bread, toasted | ¼ cup milk, heated |
| 1 tsp. butter | ⅙ tsp. salt |
Toast the bread on both sides and butter; place in a deep plate and pour over it the hot milk.
240 calories
| 1 slice bread | 1 tsp. flour |
| ¼ cup thin cream | 1 tsp. butter |
| ¼ tsp. salt | |
Cream butter and flour together cold, and stir into hot milk. Stir until the mixture begins to thicken, cover the boiler and allow to cook for 15 minutes. Slice the bread and cut into cubes; toast a delicate brown, and pour over it the cream sauce. Strain the sauce if there are any lumps.
185 calories
| 2 water crackers | ½ cup hot or cold milk |
| 2 tbs. sherry wine | ¼ tsp. grated nutmeg |
[Pg 106] Sugar may be sprinkled over crackers if desired, but it is not ordinarily done.
Place the crackers in a deep plate and pour over each cracker 1 tablespoonful of wine, dust with nutmeg and pour over the hot or cold milk.
3333 (about) calories
| 2 cups flour | 2 tsp. butter, lard, or Crisco |
| ¼ cup sugar | 1 cup seeded raisins |
| ½ cup milk | 1 egg |
| ½ cup oatmeal | ½ cup shelled peanuts |
Mix shortening and sugar together. Mix oatmeal and peanuts (broken into small pieces) into the flour. Add milk and well-beaten eggs, then the raisins; mix into a dough, roll into a thin sheet, and cut into small cakes. Bake in quick oven.
550 calories
| 1 cup milk (scalded) | 3 tbs. sugar |
| 2 egg yolks | 6 dates |
| 2 tbs. minute tapioca | |
Beat sugar and egg together, stir in the tapioca and dates, cut into small pieces. (The dates may be omitted, if desired.) Pour mixture into custard cups and bake slowly (as rice custard) until the tapioca is clear and the custard is fairly firm in center.
570 calories
| ½ cup milk | 2 tbs. minute tapioca |
| ½ cup orange juice | 2 egg yolks |
| ¼ cup sugar | 6 drops orange extract |
[Pg 107] Mix and bake as directed in plain baked tapioca custard. Any other fruit juice may be substituted for the orange, raspberry, pineapple, or grape juice.
475 calories
| 1 apple (pared and cored) | 2 tbs. sugar |
| 1 egg | 1½ tbs. tapioca |
| ¾ cup milk | ⅛ tsp. nutmeg |
Beat egg and sugar together. Heat milk in double boiler and add egg when milk is scalding hot. Stir in tapioca. Cook 20 minutes. Place apple in cup a little larger than the apple and pour the tapioca custard over the apple. Cover the cup and bake 30 minutes in a moderate oven.
470 calories
| 2 slices bread | 2 tbs. sugar |
| 1 large tart apple (or ½ cup blueberries may be substituted for the apple) | |
| 1 tbs. butter | ½ tsp. nutmeg or cinnamon |
Toast bread and break into small pieces, line the bottom of the individual baking dish with toast bits, cover with a layer of apple or berries, sprinkle with sugar and nutmeg or cinnamon, add butter in bits over this, continue the process until the dish is filled, place bits of butter on top of the last layer of toast and set dish in oven; bake about 20 minutes in a slow oven; serve with whipped cream or hard sauce.
309 calories
| 1 tbs. raw rice, broiled | ½ cup milk |
| 1 egg | 1 tbs. sugar |
| 1 tbs. whipped cream | 1 doz. raisins if desired |
| A few drops of vanilla | |
Beat sugar and egg together. Stir into the milk, stir in the rice and flavor (add raisins if desired—29 calories). Grease custard cup and fill with the mixture. Bake slowly (in a pan of hot water) until custard is firm in center. Serve with whipped cream.
532 calories
| 2 oz. orange juice | 2 egg yolks |
| 2 tbs. sugar | ½ cup milk |
| ½ cup boiled rice (or ¼ cup uncooked) | |
Beat egg, sugar, and orange juice together. Mix milk with rice and stir the two mixtures together. Bake as directed in plain rice custard.
356 calories
| ¼ cup rice | 1 cup milk |
| ¼ tsp. salt | |
Place in a double boiler and cook without stirring until milk is absorbed and rice is tender. Then either pack in egg cups (wet first so that rice will slip out without breaking), or take a square of cheesecloth 8 inches square, dust with flour and place about 4 tablespoons of the cooked rice [Pg 109] in center, draw the corners together and tie firmly into a ball. Set the ball in a steamer and steam 1 hour. Remove the cloth gently to prevent breaking the balls. They may be served with custard as a dessert, or as a vegetable with tomato dressing.
503 calories
| 1 cup milk | 1 egg |
| 2 tbs. tapioca (minute tapioca) | 3 tbs. sugar |
Flavor with vanilla or nutmeg, or ¼ square chocolate grated. Scald milk. Boil tapioca in hot water until transparent like jelly, using one cupful of boiling water. (If tapioca does not absorb all of the water, pour off the surplus.) Beat egg and sugar together and add with the milk to the tapioca. Pour into a double boiler, and cook until the raw egg flavor has disappeared. Flavor as desired. 43 calories extra with chocolate.
772 calories
| 2 tbs. sugar | 2 tbs. butter |
| ¼ cup flour | 1 cup milk |
| 2 eggs | ¼ tsp. vanilla |
Sift flour and sugar together and make into a thin paste with part of the milk, heat the remainder of the milk and stir in the flour paste. When the mixture is thick and smooth, stir in the butter, then the beaten yolks and last, the whites (well beaten) are folded in. The mixture is now turned into a baking dish and baked (in a pan of hot water as any other custard) until it is firm in the center and well puffed up and brown. Serve with foamy sauce.
1716 calories
| 7 egg whites | 1 cup sugar |
| 5 egg yolks | ⅓ tsp. cream of tartar |
| 1 cup flour (sifted 3 or 4 times) | ¼ tsp. salt |
Beat whites of eggs until foamy and add cream of tartar; beat until dry and stiff, add the sugar gradually and fold in the well-beaten yolks. Sift the flour and gradually fold into the rest of the ingredients; pour into ungreased sponge cake pans and bake in a moderate oven for 30 to 40 minutes.
721.5 calories
| 4 egg whites | ½ cup flour (pastry) |
| ½ cup sugar | ¼ tsp. cream of tartar |
Whip eggs until foamy and add cream of tartar, whip until stiff and dry, add sugar gradually, then fold in the flour (the flour must be sifted 4 or 5 times).
Pour batter into an ungreased angel food cake pan and bake in a slow oven for 25 or 30 minutes. Care must be taken not to disturb the cake during the baking, or it will fall.
1470 calories
| ½ cup fine cereal | 1 tbs. butter |
| 1 cup milk (scalded) | ½ tsp. salt |
| ¼ cup molasses | ½ tsp. soda |
| 1 egg | ½ cup dates or other dried fruit |
Stir cereal into scalded milk and cook until mixture thickens, remove from fire, add rest of the ingredients [Pg 111] except eggs. When mixture has cooled somewhat, add the lightly beaten eggs, turn into a buttered baking dish and steam 3 hours. This pudding may be made without steaming by cooking the cereal and milk in double boiler for 1 hour, then add rest of ingredients and bake 30 minutes.
494-497 calories
| ½ cup powdered sugar | 1 tbs. sherry wine or 1 tbs. hot milk |
| ¼ cup butter | ¼ tsp. vanilla |
| ½ one egg yolk and 1 whole egg white | |
Cream butter and sugar (powdered sugar must be used in this recipe). Stir in the well-beaten yolk, add sherry and pour into saucepan over hot water; stir until thick and creamy, lift from hot water and cool as quickly as possible, fold in the stiffly beaten white of egg and serve over pudding at once.
381-434 calories
| 1 egg | 1 tbs. lemon juice |
| ½ cup powdered sugar | 1 tsp. hot milk |
| 1 wineglass sherry wine or whisky, or ½ glass orange juice | |
Beat yolk and white of egg separately, add sugar to yolk and beat until creamy, add wine or fruit juice, fold in the egg white and add the hot milk last; serve at once.
231 calories
| 1 tbs. butter | ½ egg white may be added if desired |
| 2 tbs. sugar | ½ tsp. vanilla, or ½ tsp. nutmeg |
[Pg 112] Cream butter and sugar together until there are no lumps or grains in mixture. Beat the egg white stiff and fold into the sugar and butter mixture. Flavor.
794-797 calories
| ½ cup powdered sugar | 1 tbs. sherry wine or 1 tbs. hot milk |
| ¼ cup butter | ¼ tsp. vanilla |
| ½ one egg yolk and 1 whole egg white | |
Cream butter and sugar (powdered sugar must be used in this recipe). Stir in the well-beaten yolk, add sherry and pour into saucepan over hot water; stir until thick and creamy, lift from hot water and cool as quickly as possible, fold in the stiffly beaten white of egg and serve over pudding at once.
758.4 calories
| 1 egg | 1 tbs. lemon juice |
| ½ cup powdered sugar | 1 tsp. hot milk |
| 1 wineglass sherry wine or whisky, or ½ glass orange | |
Beat yolk and white of egg separately, add sugar to yolk and beat until creamy, add wine or fruit juice, fold in the egg white and add the hot milk last; serve at once.
Meats.—The flesh of animals, poultry, and fish comes under the head of meat. These food materials form one of the most important sources of protein in the diet, the foodstuff being in concentrated form easily handled by the digestive apparatus and absorbed almost completely, leaving little residue in the intestinal tract. The chemical composition [Pg 113] of different meats is very much alike, as will be seen in the table, the bulk of the weight being water, while the proteins range from 18.3% (E.P.)[40] in beef to 9.9% in bacon. The fats range from 17.9% in beef to 64.8% in smoked bacon.
The mineral salts or ash, as they are found in meat: “Sodium occurs in the animal body chiefly as chlorid in the fluids and blood, and to a less extent in the other tissues.” “Potassium, on the other hand, is much more abundant in the soft solid tissues, in the corpuscles of the blood and the protoplasm of the muscles and other organs.” “Potassium sulphate in the blood reacts to some extent with sodium chlorid, forming potassium chlorid and sodium sulphate, both of which are rapidly eliminated by the kidneys.” The greater part of the sulphur with which we are concerned in nutrition enters the body by way of the protein, the percentage in lean beef being from 0.95% to 1.00%.[41] Phosphorus in meat occurs as phosphoprotein in the nucleoproteins of cell nuclei, and lecithoproteins in the brain and to a less extent in other tissues as phosphorized fats. Meat is poor in calcium, containing only about 0.01 gram per hundred grams of substance. Meat with eggs yields a considerable amount of what is known as acids in the body.
Quality of Meats.—The quality of meat depends upon several factors: age, sex, care, feeding, and the length of time it is hung. Cold storage beef is much more apt to be tender than that cut from a freshly killed animal. Animals that are not allowed to run over a large area, but are kept in a small inclosure and fed on fattening foods, produce meat of a high quality. This is because the muscular tissue has not been hardened with exercise. The worked muscle is always tougher than the quiet one. For this reason the tenderloin of beef is more tender than the flank. It is [Pg 114] situated in the part of the animal that is exercised the least. The tough parts, however, are not lacking in flavor or nourishment, but the manner in which they must be cooked to assure them of being tender deprives them of much of their original flavor. This is demonstrated in broths and soups made from the tough cuts of meat. The extractives from which meat derives its flavor and the soluble albumens are drawn out by the water, and if it is to be used as hash, croquettes, etc., needs to be seasoned, since the broth, while it has taken very little of the actual nourishment from the meat, has deprived it of practically all of its flavor. In making broth or soup, if the meat is covered with cold water instead of hot, more of the extractives will be drawn out and the broth will be more highly flavored and much more stimulating. The color, odor, and freshness of the muscular and fatty tissues of meat are all indicative of their quality. Fresh meat is firm in texture and free from offensive odor. Stale beef and that cut from an old steer exhales a pungent odor of butyric acid. The color of beef should be dark purplish when fresh cut but this changes quickly to a bright red; it should contain preservatives of no kind and must be cut from animals free from all disease. The fat should be of a yellowish white and be crumbly, and should be distributed throughout the muscular tissue and around the organs.
Veal, being the flesh of an immature creature, is not so highly flavored as the flesh of older animals, but the bones and cartilages are softer, and when this meat is used for broth, more of the gelatin (collagen and elastin from the bones and connective tissue) is dissolved out, giving a slightly higher percentage of nutriment in the broth.
Selecting of Chicken and Turkey.—In selecting chicken for the diet of invalids, use only the young birds for broiling, those a few months older for baking and roasting, [Pg 115] and the fowls for soup and broth. To test a chicken for broiling and roasting, select one in which the cartilage at the end of the breastbone is soft and pliable; the pinions (lower part of the wings) and the feet should be soft and readily bent. The breastbone of a fowl is firmer and the wings and feet harder than those of the younger chicken. The young chicken has an abundance of pin feathers while the old fowl has not. In fact, one of the means of differentiating between the old chicken and the young, even if they are practically of the same weight, is the presence of the long hairs instead of pin feathers. The fowl selected for broth should not be very fat, as this fat will melt into the broth, causing it to be greasy and unpalatable. Turkey, even when it is young, is not quite so digestible as young chicken; the fibers are longer and the connective tissue more abundant. Goose and duck are richer in fat and not so desirable as chicken in the invalid dietary. Squab, quail, and young squirrel are all palatable and readily digested. The squirrel must, however, be young, or the flesh will be tough and more difficult of digestion.
Fish.—Fish should be given consideration in the dietary of the invalid since it is a valuable source of protein and readily digested in the majority of cases. As a rule fish is not so well liked as meat, but since it contains a smaller percentage of extractives and purin bases it is exceedingly valuable in certain pathological conditions. The lean varieties of fish, halibut, flounder, trout, perch, haddock, turbot, whitefish, are more readily digested than the dark fish, which contain a higher percentage of fat. To this latter class belong the bluefish, mackerel, salmon, shad, and herring.
Shellfish.—Of the shellfish, the oyster and the clam are exceedingly useful. The soft parts of the oyster are palatable and easily digested. They are not highly nutritious, [Pg 116] but give a nice variety to the diet. When used in broth or for the juice, clams are particularly useful. Many cases of nausea are relieved by the taking of iced or very hot clam juice when they resist other remedies. The necessity of having both oysters and clams absolutely fresh is of the greatest importance, since a type of poison results from tainted shellfish which is exceedingly dangerous.
Pork in the Diet.—Fresh pork is rarely ever included in the invalid dietary save in diabetic diets. Meat from this animal must always be thoroughly cooked, not only because underdone pork is exceedingly indigestible but because there is an infectious bacterium sometimes found in pork which is only destroyed by thorough cooking of the meat. Well-cooked bacon is digestible if the surplus fat is poured off instead of allowed to soak into the cooked bacon. The most efficient method of cooking bacon is to place the strips upon a broiler under the flame. In this way the hot fat drips down into the pan beneath, leaving the bacon crisp and delicate.
The meats to be used for the invalid must be selected with care. The quality of this item of food is most important. It is not always necessary to purchase the most expensive cut. If it is to be broiled or roasted then it is necessary to select parts of the animal which are tender, but for broths, soups, scraped or ground meat, or the meat to be used for the juice only, it is wasteful to buy these tender, expensive pieces when those costing less will serve the purpose equally well. The names given to the different cuts vary slightly in different parts of the country, but those in general use only will be mentioned here. The following table shows the manner in which the beef is cut and the method in which it is generally used:
| Beef | Cut | Method of Preparation | ||
| Hindquarter | Round | more or less free from fat | Broth, soup, beef juice, scraped beef. | |
| round steak | Hamburg steak (ground meat). | |||
| Broiled (this is a cheaper and less tender cut than the loin steaks). | ||||
| steak | Broiled, cheaper cut steak. | |||
| Rump | roast | Roasted, cheaper cut roast. | ||
| lean meat | Broth, soup, beef juice. | |||
| 3 ribs, 1st, 2d and 3d cuts | Roasted. | |||
| Loin | sirloin steak | Broiled. | ||
| porterhouse steak | Broiled. | |||
| steak | Broiled. | |||
| Tenderloin | roast | Roasted. | ||
| fillet | Broiled or roasted, larded or plain. | |||
| Ribs (prime) | Roasted. | |||
| Ribs, chuck roast or steak | Roasted or broiled. | |||
| Forequarter | Brisket | Corning. | ||
| Broth, soup, scraped, meat juice. | ||||
| Hamburg steak. | ||||
| Salisbury steak. | ||||
| Lamb | Neck | Soup, broth, etc. | |
| Chuck (including shoulder ribs). | |||
| Shoulder chops are not so tender as loin chops. | Broiled. | ||
| Flank | Soup, broth. | ||
| Loin (chops) | Broiled. | ||
| Leg | Roasted. | ||
| Veal | Neck | Soup, broth. | |
| Chuck | Soup, broth, roast, broiled. | ||
| Cutlets | Broiled (breaded or plain). | ||
| Chops (rib) | Broiled. | ||
| Breast | Roasted, stuffed or plain. | ||
| Leg | Roasted. | ||
| Hind shank | (veal knuckles) | Soup, broth. | |
| Fore shank | |||
1 Pint, 80 calories, with rice or barley 105 calories
Two pounds of meat (beef, mutton, veal, or chicken); 2 quarts of water; 2 pounds of bones; 1 teaspoonful of salt; 2 tablespoonfuls of rice or barley may be added if desired and parsley or celery may be used to give the additional flavor.
Wipe meat with a clean wet cloth and cut into small pieces, break the bones, place all together in a deep saucepan, cover closely and allow to stand in a cool place for one hour; then place pan on the back part of the stove, or on an asbestos mat over a gas burner, and heat gently to the boiling point (broth must never do more than simmer), allow to simmer for three or four hours, skim, strain, and cool. When thoroughly cold, remove all of the fat, using blotting paper to absorb the fine particles of grease. If parsley and celery are to be used to flavor the broth they may be added during the last hour of cooking. Barley requires to be soaked overnight when it is used in broth; rice should be soaked one hour. When either are to be left in the broth it is better to cook the broth for three hours, strain, return to the fire, adding the rice or barley. Allow it to simmer for an hour or more and proceed as directed. When the broth is taken from the fire, it should be measured, and boiling water added to bring the amount up to the original quantity. This will give what is known as standard broth. Bouillon is clarified broth, most of the already small amount of nutrient material being thus strained and cleared from the broth, leaving a liquid of practically no fuel value.
11.5 calories without milk; 162.5 calories with milk
| 1 doz. clams or oysters | 1 pt. water or 1 cup each milk and water |
| 1 tbs. whipped cream | A dash of pepper |
Scrub clams and place in an iron spider and allow to heat gently until the shells open. (When oysters are used allow to heat until the edges curl.) Chop, cover with hot water, and allow to simmer 15 minutes, strain through cloth, add salt and a dash of pepper. If milk is to be used in place of part of the water, add it during the last 5 minutes of the cooking. Clam broth without milk may be served hot or cold; it will not jelly as other broths but may be frozen if desired.
Without milk, 55.6 calories; with milk, 113.4 calories
| ½ cup (4 oz.) clam juice | Salt and pepper to taste |
| ½ cup hot water or milk | 1 tbs. whipped cream |
Mix clam juice (bottled) with water; heat, add salt and pepper, pour into cup, place whipped cream on top, and serve at once.
One-fourth pound lean beef.
Wipe clean with damp cloth, cut in inch pieces and sear on a hot griddle, place in a meat press and remove all juice from meat. Care must be taken not to cook the meat. The juice may be reheated by placing in a hot cup in hot water, not allowing the temperature to exceed 155° F.
308 calories
1 serving, 75.8 calories
| ½ small chicken | 1 tbs. gelatin soaked in ¼ cup cold water |
| 3 pt. water | ½ tsp. salt |
| ½ cup celery | ¼ tsp. red pepper |
| 1 sprig of parsley | 1 egg white |
Cut the chicken in pieces, break the bones, place in a saucepan with all of the ingredients except the gelatin and egg white, cover with the water and boil until the meat falls from the bones. Press out as much of the juice as possible, strain and allow to cool, remove all of the grease, and return to the fire. Reduce to 1 pint, add the gelatin, stir in the beaten egg white, and allow to boil 5 minutes, strain again into molds and set aside to congeal.
376.6 calories
| 2 small calf’s-feet | 1 lemon |
| ½ small fowl | ½ stick of cinnamon |
| 1 cup of Rhine wine | 1 egg white (well beaten) |
Cut the fowl and the calf’s-feet into small pieces and place them in a saucepan with 3 pints of cold water and the cinnamon. Cook until the meat falls from the bones (the quantity should be reduced to 1 pint). Strain and squeeze out as much of the juice as possible, allow to cool, and remove all of the grease. Add wine and lemon juice (and sugar if desired) and reduce the amount of broth one-half, add the egg white and allow to boil 5 minutes. Clear and strain into molds.
418-543 calories
Split down the back and place on the broiler, cut surface uppermost. Or place upon a hot pan, cut surface next to the hot surface so that the cut side may sear quickly, thus keeping in the juices instead of having them wasted in the pan by slow cooking. The process requires about 15 to 20 minutes. Serve on toast, with butter, pepper and salt.
Quail or squab cooked inside the stove is often more palatable than that cooked on a broiler. The bird is split as for broiling, and placed in a small pan just large enough to hold it; a strip of bacon pinned about the breast; add 1 tablespoonful of butter in bits, dust the cut surface first with salt and pepper, then with flour; add ½ cup of hot water. Turn another pan over the bird (it must fit closely to keep in the steam), place inside the oven and cook about 10 minutes; turn the bird over and cook 10 minutes longer. Lift the bird from the pan and place it where it will keep hot, add a tablespoonful more water and a teaspoonful more flour to the gravy in the pan, stir briskly to remove any lumps, remove bacon and place the bird upon a slice of nicely browned toast; pour over it the gravy, garnish with a sprig of parsley, and serve at once.
| 1 small chicken, or bird | 1 tbs. parsley |
| 2 tbs. butter | Salt and pepper |
Split birds or chicken as for broiling, place one-half in a chafing dish or double boiler (bain-marie), dot the cut surface with butter, sprinkle over it the parsley, dust with pepper and salt; place the other half of the chicken or bird on top of this, add the rest of the butter, dust with salt and pepper, cover, and place the pan over the hot water [Pg 122] pan; allow to steam for about 1 hour, lift from hot water pan and place in oven or under the flames to brown lightly. Serve on buttered toast.
355 calories
Split small chicken (broiler) down the back, flatten the breast bone with knife before placing upon the broiler, proceed as in broiling birds, allowing from 25 to 30 minutes for the process. Chicken is very palatable and dainty if cooked after the manner described in cooking quail and squab inside the stove. The process is called smothering. Serve upon buttered toast, garnished with parsley.
Draw the fowl and wash thoroughly inside and out. (If it is purchased from the market, it is well to wash the inside with soda water to remove any stale flavor that may be present.)
Make a dressing from one-third of a small loaf of bread broken into small pieces; ¼ cup chopped celery, 1 tablespoonful of chopped parsley, 1 tablespoonful of butter and one egg beaten lightly. Stuff the cavity with dressing, sew up the opening and place in dripping pan. Place pan under the flame for a few minutes to brown, unless a regular roasting pan (savory roaster) is used; allow to bake from 45 minutes to an hour and a half for chicken and duck according to the size, and from an hour and a half to three hours for turkey according to size. A cupful of boiling water may be poured into the pan in which the chicken, etc., is being roasted and flour may be sifted over the top; dust with salt and pepper. When an ordinary pan is used for baking, the fowl will require frequent basting to keep it moist and tender. Just as the baking is finished, more [Pg 123] butter, flour, and seasoning may be added, with a cup or more of boiling water to make additional gravy.
209 calories
| ¼ set of sweetbreads | ½ tsp. of salt |
| 1 lemon | ¼ tsp. of pepper (red) |
Wash sweetbreads carefully and allow to stand 1 hour in ice water, allow the water containing the lemon juice, salt and pepper to come to a boil and drop in the sweetbreads, cook for 15 to 20 minutes or until tender when pierced with fork. Remove from hot water and pour ice water over them to blanch. Serve either in cream sauce or split in half and broil upon a slightly greased broiler until light brown; season with a dash of salt and pepper.
174 calories
| 6 oysters | 1 slice toast |
| 2 tsp. butter | Salt and pepper to taste |
Grease broiler or hot frying pan slightly, place oysters upon the heated surface and place under the flame or on top of the stove; cook until the edges curl (2 to 3 minutes), lift to a hot dish containing the butter, place toast upon small plate (toast and plate must be hot), dispose the oysters upon the toast, and pour over them the butter.
267 calories
3 inches long by 2 inches wide by 1½ inches thick (weighing about 3 ounces).
Wipe steak off with a wet cloth and dry before cooking. Slightly grease the broiler and place under the flame, count [Pg 124] ten as the clock ticks and turn the steak over, count ten again and again turn; continue this for about 3 minutes or until the steak is seared upon both sides, lift the broiler to a lower part of the oven and continue the cooking for 5 to 8 minutes; run a sharp-pointed knife between the meat and the bone (if the steak is a porterhouse or sirloin), and if the flesh is red, continue the cooking a minute or more. If it is pink, lift to a hot plate, place 1 teaspoonful of butter upon it, dust the surface with salt and pepper and serve hot. Pan broiling is done on the top of the stove in a flat frying pan. Wipe the pan with a clean wet cloth, place upon the stove and heat piping hot, and place the steak (without greasing the pan) upon the hot surface. Proceed as in broiling under the flame. After the first 3 minutes of cooking, place the pan on a cooler part of the stove to finish the cooking.
2 chops, 304 calories
1 to 2 inches thick will require from 10 to 15 minutes’ cooking. Scrape the bone clean and wrap in paper or dough to prevent the bone from becoming charred. Proceed as in cooking beefsteak.
2 cutlets, 275 (about) calories
Dip cutlets first in egg (mix one yolk with 1 tablespoonful of water) then in bread crumbs; pan broil (grease the frying pan slightly), or broil under the flame as directed in cooking beefsteak. Veal cutlets may be served plain, or with tomato sauce.
Cutlets or chops may be cooked in paper bags if desired. Wrap the chop in a thin slice of bacon, grease the paper (a piece of heavy brown paper), place the chop inside and secure the ends with paper clips or pins; place in a pan and [Pg 125] cook in the oven, or under the flame. It is wise to slip the bag containing the chop inside of another bag; in this way the meat will not taste of scorched paper if the outer bag should burn.
194 calories
Place bacon on a rack and place rack in a dripping pan, set in oven and bake until crisp and brown. Or, arrange bacon on broiler, place pan beneath to catch the drippings and prevent the fat from catching afire, broil as beefsteak.
When steak or chops are served, parsley or sliced lemon may be used as garnishes. Chops may be served garnished with green peas, and the beefsteak served with potatoes cooked in any way; all meats should be served very hot. It is best to cover with a plate.
Split down the back, and broil as beefsteak. Fish does not require more than from 10 to 15 minutes to broil unless very large. Serve with teaspoonful of parsley and butter.
3 ounces, 168.3 calories (about)
Halibut, trout, or any good baking fish, 235.8 calories (about)
| 2 slices of fish | 1 cup bread crumbs |
| 1-1½ in. thick | 4 tbs. butter |
| 1 doz. oysters | Salt and pepper |
Lay fish for one hour in a French dressing made from ½ cup of oil, ⅓ cup of vinegar, salt and pepper; drain and place upon slices of bacon, placed upon a fish sheet or dripping pan. Dip oysters first in melted butter, then in bread crumbs, and place upon the slice of fish, adjust second slice above, cover top with bread crumbs, dot with butter and bake 30 to 45 minutes in moderate oven. Serve with hollandaise sauce.
1 serving lobster, 157 calories
1 serving crab, 154 calories
| 1 lobster, | 1 tbs. butter |
| or 1 crab | 2 tsp. butter |
| 2 tbs. bread crumbs | ¼ tsp. salt |
| ⅛ tsp. pepper | |
Boil lobster or crab until bright red, lift from boiling water.
Split lobster down the back and carefully remove cord, gall sack, and sand bag before broiling or serving. Serve with melted butter.
Pick meat from shell of crab, and mix with salt, pepper and butter. Stuff into shell. Cover top with bread crumbs, and brown in the oven.
178 calories; 1 tablespoonful, 22 calories
| 1 egg (yolk only) | 1 tbs. butter |
| 2 tbs. lemon juice | ¼ cup boiling water |
| Salt and pepper to please | |
Beat egg yolk with lemon juice; add one-half the butter; place in double boiler over hot (not boiling) water. Stir until it begins to thicken and add remainder of butter; stir in boiling water, cook until of the consistency of boiled custard.
Among the plants known as vegetables, some are seeds, some leaves, some stems or bulbs, some roots or tubers, and some are the fruit surrounding the seeds. Under the head of seeds we find peas, beans and lentils, this class of vegetables being spoken of as legumes or pulses; they are rich in [Pg 127] protein (especially when dried) and contain an appreciable amount of carbohydrates as well, some contain fat. Green, or fresh legumes are more easily digested than the dried legumes. They are important sources of iron and phosphorus and contain a certain amount of calcium; in the body they act as neutralizing agents since the base-forming elements in these plants predominate over the acid-forming elements.[42]
Among the “leafy vegetables” we find, lettuce, cabbage, spinach, beet, turnip and mustard greens, chard and parsley. These vegetables are not only prized for their mineral content but furnish a recognized source of the fat soluble vitamine, “A.”
Tomatoes, squash, cucumbers and pumpkin are vegetables whose “fleshy fruit” surround the seed but are eaten as vegetables instead of as fruit.
Potatoes, carrots, parsnips, onions, beets and turnips are among those whose stems, roots or tubers are eaten as vegetables.
More and more are we coming to see the importance of this class of foods in the dietary, they are important on account of their mineral salts, their vitamine factors and for the bulk which they lend to the food mass which facilitates its passage along the digestive tract. The majority of vegetables furnish organic acids or their salts which function in the body, as potential bases, assisting in the neutralization of the acids formed in the body as a result of the breaking down of the proteins.
Fruits.—Fruits have practically the same value from a dietetic standpoint as vegetables, and the same care must be given to their selection. Some fresh fruit should be given to children every day to safeguard them against scurvy. And adults should have fresh fruit several times a week, the remainder of the time dried fruits may be used. [Pg 128] Canned fruits while good are not so valuable as fresh fruits and are more expensive than the dried fruit.
The fruits and vegetables will here be considered. Some of the fruits and vegetables contain high percentages of sugar, aside from the mineral salts, for which they are especially valuable. This class includes the sugar cane, sugar beet, raisins, dates, figs, etc., while others such as the potato, taro, banana, etc., furnish an appreciable amount of starch. All of the vegetables and fruits are rich in mineral salts, which are as important to the work of the body as the proteins, carbohydrates, and fats. Hence it is essential to add the foods containing these mineral salts to the daily dietary both in health and in disease.
Both fruits and vegetables should be free from blemishes. Those to be served raw, such as lettuce and other salad vegetables, must be purchased from reliable markets. Unscrupulous vendors have been known to sprinkle old wilted vegetables, to restore their freshness, with water from stagnant pools teeming with typhoid bacteria, thereby spreading infection broadcast. Vegetables which require cooking before they are eaten are, for this reason, safer.
Canned foods should be avoided in the diet of the invalid whenever it is possible; but, when it is not, care should be observed that no can is used in which there is the least sign of fermentation. Beans and peas are sometimes artificially colored, but this custom is not so prevalent now as it used to be.
121 calories
| ½ cup fresh peas | 1 tsp. butter |
| 1 pt. boiling water | ¼ tsp. salt |
[Pg 129] Add salt and peas to boiling water; allow to cook from 30 to 60 minutes, or until they are perfectly tender, drain and add butter and additional salt if necessary, or 1 tablespoonful of cream sauce. In gastro-intestinal disorders and with young children, it is best to press peas through sieve or remove the indigestible parts.
94 calories
| 1 cupful of string beans (measured after the strings are removed and the beans cut into small pieces) | |
| 1 tsp. butter | ½ tsp. salt |
Cover with boiling water and cook until tender, drain, and serve hot.
90 calories
| ½ lb. spinach | ½ tsp. salt |
| 2 tsp. butter | |
Wash thoroughly through about ten waters, until spinach is entirely free from grit, remove the tough stems, lift the spinach from water and place in a saucepan without additional water, sprinkle over with salt, cover saucepan and cook until tender (requires about 15 minutes). Cut very fine with sharp knife, or press through sieve, add butter and serve hot.
82-117 calories
Carrots, about ½ cupful after they are cut in cubes, or 3½ ounces. Serve with 2 tablespoonfuls of cream sauce, or with 2 teaspoonfuls of butter and a little salt and pepper. Scrub carrots and scrape off the skins; cut into slices or [Pg 130] cubes, drop into slightly salted boiling water and cook until tender; drain and add butter or cream sauce.
140 calories
1 potato weighing about 3 ounces; scrub well with a brush; dry and slightly grease surface, place in moderately hot oven and bake about 45 or 50 minutes. (The potato should feel tender upon pressure.) When done, make an incision of 1 inch in the skin and gently press out the steam; cover closely with cloth and keep in a warm place until ready to serve. Put teaspoonful (about ⅙ ounce) of butter in the cut and serve very hot.
182 calories
| ¼ tsp. salt | 2 tsp. milk |
| 1 medium size potato | 1 tsp. butter |
Pare and boil potato until tender when pierced with a fork; drain off the water and return the saucepan to the stove; shake the pan (to prevent burning) until the potato looks dry; mash with fork or potato ricer, add milk, butter, and salt. Beat briskly until creamy. Serve at once or brown in oven.
197.5 calories
| 1 potato (baked) | 1 tbs. cold chopped beef |
| ¼ tsp. salt | 1 tsp. butter |
| Dash of pepper | |
Bake potato, split in half and remove the contents, mix with the chopped meat, add salt, pepper, and butter; return to the two halves, set in oven to brown, then serve at once.
250.8 calories
| 1 potato | ¼ cup milk |
| 2 tsp. butter | |
Boil potato, not quite tender, and slice in moderately thin slices; arrange in layer in an individual earthenware baking dish (ramekin), add butter in bits between layers, pour the milk over; set dish in oven, cover and bake slowly for 15 minutes, until most of the milk is absorbed and the potatoes are nicely browned on top. In cases where the patient is allowed cheese, 2 teaspoonfuls may be sprinkled between the layers, giving 31 additional calories.
62.5 calories
| ½ cucumber (7 in. long) | 1 tsp. olive oil |
| ½ tbs. vinegar | ⅙ tsp. salt |
| Few grains of pepper | |
Slice cucumber in thin slices and allow to stand thirty minutes in ice water, drain and serve with French dressing.
with mayonnaise, 61 calories
with French dressing, 131 calories
Wash tomato carefully, cut in shape of flower by cutting almost through the tomato making six sections. Place on lettuce leaf and serve with dressing.
| 1 tsp. mayonnaise or | 1 tbs. French dressing |
63 calories
Remove skin from 1 medium sized tomato, remove pulp, fill cavity with following mixture.
| ½ medium stalk celery | The tomato pulp |
| 1 tsp. mayonnaise dressing | |
| 3 grapefruit | ¼ head of lettuce |
| 1 cup celery (chopped) | 1 cupful of mayonnaise |
Remove skin and inner membranes from grapefruit, mix with celery and mayonnaise. Serve on lettuce. This salad may be poured into a tin (baking powder can, or mould), packed in ice and salt and frozen. Then served in slices upon lettuce.
1217 calories (about)
| 1 cup of grapefruit | 1 green pepper (1 oz.) |
| 1 thick slice of pineapple (chopped) | 1 cup of celery |
| 1 cup of mayonnaise or French dressing | |
If mayonnaise is used the mixture may be frozen. If French dressing is used, serve on lettuce without freezing.
77 calories
| 1 cup tomatoes (canned) | ¼ cup vinegar |
| ¾ cup water | 1 tbs. of parsley |
| 6 cloves | ½ tsp. red pepper |
| ½ cup celery | 1 tbs. granulated gelatin soaked in ¼ cup cold water |
[Pg 133] One slice of onion may be added if there is nothing to contra-indicate it, but care must be taken in adding onion, as it is apt to disagree with many people. Boil all of the ingredients together (except the gelatin) for 20 minutes, press through a sieve, then through a cloth, return to the stove and allow to boil up; add the gelatin and boil 5 minutes; strain into wet molds.
167 calories
| 1 medium size tomato | 1 tsp. butter |
| 2 tbs. rice (uncooked) | Dash of pepper and salt |
Remove the center from the tomato, dust the inside with salt and a very little pepper and set aside. Boil the rice, when about half done (10 minutes) add the tomato pulp, from center of tomato. Cook 10 minutes longer, drain the water from the rice, add the butter, salt, and a little pepper. Fill the center of tomato with rice. Set the tomato upon a greased paper and bake in a moderate oven for 20 minutes.
353 calories
| Slice 1 tomato in three or four slices | 1 slice of bread (round preferred) |
| 1 tbs. butter | ¼ cup of cracker crumbs |
| Salt and pepper | |
Heat broiler or frying pan very hot, grease lightly; season crumbs with salt and pepper; dip slices of tomato in cracker crumbs, covering both sides well, and place upon the broiler; when one side is browned, turn over carefully, to prevent breaking, and allow the other side to brown. Lift the broiler to the lower half of the oven and let the [Pg 134] tomatoes cook gently for 10 minutes. Place bits of butter upon each slice, then arrange these on the buttered toast.
171 calories
| ½ cup canned tomatoes | 1 slice bread |
| ½ cup water | 2 tsp. butter |
| ¼ tsp. salt | |
Pour tomatoes and water in a saucepan and allow to cook slowly for 20 minutes, add salt and a dash of pepper. Toast and butter the bread, pour the cooked tomatoes over it and serve at once.
131 calories
| 1 tbs. oil | ⅓ tbs. vinegar, or lemon juice |
| Dash of pepper and salt | |
Have all ingredients cold; mix salt and pepper together; stir in the oil, add vinegar or lemon juice slowly, beating briskly to form an emulsion; use immediately or ingredients will separate.
Use as little salt as possible in nephritic conditions.
2109 calories
| 1 egg (yolk only) | ½ tsp. mustard (dry) |
| 2 tbs. lemon juice (or vinegar) | Dash red pepper |
| ½ tsp. salt | 1 cup olive oil |
Method of Mixture: Mix dry ingredients with yolk of egg thoroughly; add all the acid (use Dover beater). Now add, one teaspoonful at a time, the olive oil; beat continually until the mixture thickens (after 8 teaspoons of oil have been added). Put in oil by tablespoonfuls until [Pg 135] all is incorporated. This method shortens the time of making at least one-half, and the dressing rarely curdles as it often does in the old methods.
Whipped cream may be added to dressing before serving. Mayonnaise will keep if placed in a cool place, and the above quantities are more easily handled than smaller amounts.
150 calories
| 2 lemons (juice only) | 1 tbs. cold water |
| ¼ cup sugar | 1 egg white |
| 3 tsp. granulated gelatin | 1 cup boiling water |
280 calories
| 3 tsp. granulated gelatin | 6 tbs. lemon juice |
| 1 tbs. cold water | 3 tbs. sugar |
| ¼ cup boiling water | 2 drops orange extract |
| ½ cup orange juice | |
315 calories
| ¼ cup boiling water | 1 tbs. cold water |
| ½ cup boiling grape juice | 1 tbs. lemon juice |
| 3 tsp. granulated gelatin | 3 tbs. sugar |
Method for Fruit Jellies.—Soak gelatin in cold water about 2 or 3 minutes, then pour over it the boiling liquid; add sugar and fruit juice; strain through cloth into wet molds. Set in cold place to stiffen; when firm, unmold. Serve with whipped cream, or pour liquid into baskets made from oranges or grapefruit hollowed out and the edges [Pg 136] scalloped, or pour into shallow pans, and cut in ½-inch blocks when firm, and serve on a bed of whipped cream.
127 calories
| ½ cup boiling water | 1 tsp. lemon juice and the yellow rind from ¼ lemon |
| 3 tbs. sherry wine | |
| 1-inch piece of cinnamon | 3 tbs. sugar |
Method for Wine Jelly.—Put water, wine, lemon juice, peel, cinnamon, and sugar into a saucepan, allow to boil 5 minutes, pour over gelatin (which has been soaked in cold water). If jelly looks cloudy return to saucepan, and add ½ egg white beaten stiff, allow to boil 1 minute, stirring constantly, and strain into mold. Serve with whipped cream.
276.5 calories
| 2 lemons (juice only) | 1 egg white |
| ¼ cup sugar | 1 cup water |
311 calories
| ½ cup orange juice | 1 cup water |
| 1 lemon | ¼ tsp. orange extract |
| ¼ cup sugar | 1 egg white |
362.6 calories
| ½ cup grape juice | ¼ cup sugar |
| 1 tbs. lemon juice | 1 egg white |
Mix sugar and water and boil to a rich sirup (about 15 minutes), cool, and add fruit juice (and extract when it is used). Pour into freezer and surround with a mixture of 1 part salt and two parts ice. When sherbet is about half frozen, stir in the stiffly beaten egg white and continue the freezing until mixture is hard. In diseases where it is found inadvisable to give albumen, 1 teaspoonful of gelatin may be substituted.
384 calories
| ½ cup apricot purée | ¼ cup sugar |
| 1 cup water | 1 tsp. granulated gelatin |
| 1 lemon (juice only) | |
Make sirup of water and sugar, soak gelatin in a little cold water and add to the hot sirup; press apricots through a sieve and add to the sirup as soon as it is cool; freeze as directed in other ices.
346-393 calories
| 1 cup fruit juice | ⅓ cup sugar |
| Juice of 1 lemon and | 1 egg white |
Proceed as in other ices.
526 calories
| 1 cup fresh currants | ½ cup sugar |
| 1 cup water | 1 tbs. lemon juice |
Wash currants carefully and place in a saucepan on a warm but not hot part of the stove, allow to heat gently until the currants are soft, press through a cloth, and add [Pg 138] the water and sugar; stir until dissolved (or make a sirup of the water and sugar and add the currant juice and lemon and freeze as directed in other ices). The egg white may be added if desired.
| 3 cups (24 ounces) milk | 1 cup cream (8 oz.) |
| 4 lemons | ¾ cup of sugar |
Mix cream, milk and ¼ cup of sugar and pour into freezer; freeze until half frozen (mushy). Add juice of 3 lemons and 1 whole lemon (peel and pulp) shaved into very thin slices sweetened with remainder of sugar (if not sufficiently sweet add more sugar and make allowances for same in fuel value). Continue the freezing until sherbet is of the right consistency.
with wine 758 calories; without wine 745 calories
Two servings
| ½ cup 40% cream | 8 pecan or walnut meats |
| 2 tbs. sugar | ¼ tsp. vanilla or 1 tbs. sherry wine |
Dissolve sugar in the cream and beat solid, add flavoring or sherry and nuts.
631 calories
| ½ cup of orange jelly mixture (see directions for making under jellies) |
| ½ cup double cream |
| 1 tbs. sugar (the above quantity will require about 2 tsp. of granulated gelatin) |
[Pg 139] Pour jelly mixture into a bowl and surround with cracked ice; when it begins to stiffen, fold in the stiffly beaten cream.
Pour into molds or ice cream glasses and set aside in the ice-box to become set.
428 calories for orange pudding
Orange, lemon, grape juice, or pineapple may be used in preparing this pudding.
| ½ cup fruit juice | ¼ cup sugar |
| 2 tsp. gelatin | 1 egg white and |
| 1 tbs. cold water | ¼ cup soft custard |
Make jelly mixture as already directed and place the bowl in a pan of cracked ice; when the mixture begins to stiffen, fold in the well-beaten egg white (beat it in with an egg beater). Pour the mixture into a mold or individual glasses and set aside on ice to become set. When ready to serve, unmold and pour on the soft cold custard.
184.4 or 244.9 calories
| 6 prunes or 4 prunes and 1 fig | 1 egg white |
| 2 tbs. sugar | |
Cook the prunes and figs in sufficient water to cover them until they are perfectly soft, press through a sieve, add sugar, chill thoroughly, and fold in the stiffly beaten egg white. The above mixture may be put in individual cups and baked in a slow oven (in a pan surrounded with hot water) until they are firm in the center and a light brown. Serve with or without whipped cream.
[29] “Archives of Pediatrics,” Vol. XXII, p. 515, by Van Slyke.
[30] “Chemistry of Food and Nutrition,” by Henry Sherman.
[31] “Diseases of Nutrition and Infant Feeding,” by Morse and Talbot.
[32] Bulletin 56, Hyg. Lab., Public Health Service, 1908; Circular 153, U. S. Dept. Agric., Bureau of Animal Industry, 1910.
[33] “Diseases of Nutrition and Infant Feeding,” p. 173, by Morse and Talbot.
[34] Quoted from “Diseases of Nutrition and Infant Feeding,” p. 173, by Morse and Talbot.
[35] Rosenau: Bulletin 56, Hyg. Lab., Public Health Service, 1909; Circular 153, U. S. Dept. Agric., Bureau of Animal Industry, 1910.
[36] Sommerfield: Handbuch der Milchkunde, J. F. Bergman, Wiesbaden, 1909.
[37] Buttermilk Tablets may be purchased from the Chas. Hanson Co. Lab., N. Y., or from Parke, Davis & Co. The Buttermilk Starter is prepared by the first mentioned firm and is ready to use, directions coming with each sample.
[38] Recipes for coffee, egg, cocoa and chocolate junket will be found in junket recipes, from the Chas. Hanson Co.
[39] Egg white is frequently added to increase the nutrient value of ice creams and water ices.
[40] Edible Portion.
[41] “Chemistry of Food and Nutrition,” by Henry Sherman.
[42] “Food Products,” by Henry Sherman.
Put one pint of skimmed milk into a clean saucepan and heat to a temperature of 100° F. (lukewarm). To this milk add 2 teaspoonfuls of liquid rennet, essence of pepsin, or 2 junket tablets, stir until well mixed, and allow to stand at room temperature (70° F.) until firmly jellied. Break up with a fork until it is finely divided, strain through thicknesses of cheesecloth; return the fluid part to the stove and raise to a temperature of 150° F. to destroy the rennet left in the whey. The whey is then cooled before it is added to the milk or cream.
| 3% decoction starch[43] |
| 4 rounded tsp. barley flour |
| 1 pt. water |
Mix a small amount of the water with the barley flour and put the rest of the water into a clean saucepan and allow to heat; when boiling add thin barley mixture, stir thoroughly, and allow to boil 20 minutes; remove from stove, measure, and replace with hot water that which was lost through evaporation to make up the original pint; strain through two thicknesses of cheesecloth.
| 4 rounded tsp. oat flour |
| 1 pt. water |
Mix and proceed as in making barley water.
| 8 oz. water (cold) |
| 1 egg white |
| 1 tsp. brandy |
Mix egg and water and add brandy slowly to prevent coagulating egg white.
Composition: 0.60% fat, 2.90% protein, and considerable extractive matter.[44]
Place a piece of round steak upon a hot griddle and turn once or twice until the outside is seared and the meat is hot throughout. Remove from griddle and cut into small pieces and place in a small meat press made for the purpose. A lemon squeezer may be used when the press is not available. Salt lightly. Begin by giving one teaspoonful and increase the amount gradually to 1 ounce (6 teaspoonfuls). According to Morse and Talbot, it is never wise to give babies more than 2 ounces of beef juice even in their second year, as it is apt to disturb digestion. Also babies are often made restless or sleepless by taking beef juice.
347 calories
| 1½-2 tbs. malt soup extract (reduce if necessary) |
| 1 level tbs. sifted flour |
| 1 pt. milk |
| 18 oz. water (hot and cold) |
[Pg 142] Dissolve malt soup extract in ½ cup of hot water and measure in enough cold water to cool the mixture. With the remaining cold water mix the flour until it is free from lumps; and to the malt soup mixture, add milk. Pour all into a clean saucepan and bring slowly to the boiling point; simmer (not boil) for 20 minutes. Now increase the heat and allow the mixture to boil 5 minutes; strain and use as directed.
This is a fattening mixture and the amount of malt soup and whole milk may be increased as the child is able to handle it, taking care, however, not to increase the strength of the mixture too rapidly or too much, or digestional disturbances will result.
544.6 calories
1 tbs. wheat flour, 4 tbs. dextri-maltose, 8 oz. hot water plus enough hot water to replace that which is lost through evaporation (about 6 oz.). Buttermilk, sufficient quantity to make 1 quart of mixture. Mix flour with a little cold buttermilk. Dissolve sugar (dextri-maltose) in the hot water.
Stir two mixtures together and add enough buttermilk to make 1 quart. Place on stove and bring mixture quickly to a boil. Boil for 20 minutes, stirring constantly, strain, measure, and add enough boiling water to replace that which is lost in cooking. Place on ice and use as directed.
The nurse will soon be able to tell how much water is lost in evaporation and add the additional amount to the mixture before beginning the boiling.
| 1 quart fresh whole milk | 4 teaspoons essence of pepsin, |
| 1 pint of fresh buttermilk | |
[Pg 143] Heat whole milk to 100° F., add essence of pepsin and stir thoroughly. Allow to stand at same temperature until the curd is formed. Pour mass into muslin bag and drip the whey from the curd. When the mass is as dry as it is possible to have it, remove it from the bag to a fine strainer. Press curd through the strainer with a wooden spoon or potato masher (the author has found that a potato ricer with a piece of copper gauze, such as is used in a chemical laboratory, inserted, facilitates the breaking up of the curd). The mass must be passed several times through the strainer in order to make the precipitate sufficiently fine to look like milk. During the process of straining, the buttermilk is added. The composition of above formula is, according to Finkelstein and Meyer, as follows:
Protein 3%, Fat 8.5%, Sugar 1.5%, Salts 0.5%.
There are several prepared Eiweissmilch mixtures on the market, Beebe, Hoose and others. Larasan Roche is also a prepared mixture having a composition much like that of the original Eiweissmilch, it is easily prepared, and the results from feeding this milk have been found generally good.
| ½ lb. each prunes and dried figs |
| 1 oz. senna leaves |
Boil from 2 to 3 hours as directed in preparing prunes as above. Lift fruit from hot sirup, place in quart jars, strain the juice and pour over the fruit. Use as needed.
| ⅓ lb. prunes (pits removed) | ⅓ lb. figs |
| ⅓ lb. raisins (seeded) | 1 oz. senna leaves |
Boil prunes just enough to allow of the pits being removed. Cool and pass with the senna leaves, figs and raisins [Pg 144] through the food chopper. After passing through once return to chopper and pass through a second time. See that the senna leaves and fruit are thoroughly mixed and finely chopped. Place in a quart jar and give in doses of from 1 to 2 teaspoonfuls night and morning.
560 calories
| 2 tbs. molasses | 1½ cup bran |
| ½ tsp. salt | ½ tsp. soda |
| ½ cup milk | 1 egg |
Mix soda into bran, add salt, stir milk and molasses together and stir into bran; add well-beaten egg. Bake in 6 well-greased gem pans.
832 calories
| 1½ cups bran | 1 egg |
| 1 tbs. sugar | 1 cup milk |
| 2 tbs. melted butter | 2 tsp. baking powder |
Mix together and bake in 6 well-greased gem pans.
706 calories
| 1 cup of bran | 2 tbs. butter and lard mixed |
| ½ cup of flour | 1½ tsp. baking powder |
| ½ tsp. salt | ⅓ cup of milk |
Mix flour, salt, baking powder and shortening together. Add milk to make a soft dough. Mold into biscuits, and bake in a quick oven 10 to 12 minutes.
2187.5 calories
| ½ cup of sugar | 1 tsp. cinnamon |
| ½ cup of molasses | 1 tsp. ginger |
| ¼ cup of butter and lard mixed | ½ tsp. cloves |
| 1½ cups of bran | ½ tsp. nutmeg |
| 1 cup of flour | 2 eggs |
½ cup raisins or nuts may be added, due allowance being made for the additional fuel value.
Cream butter and sugar together, add molasses. Sift flour, salt and spices together. Add eggs (well beaten), to sugar mixture and stir in the remainder of ingredients. Drop from spoon on a well-greased pan, bake in moderate oven to a delicate brown.
(See Protein-free cookies, p. 340.)
| 6 oz. milk, 1 egg | ½ oz. normal saline solution |
| 1 tsp. pure peptone (this may be omitted) | 1 tube peptonizing powder dissolved in 1 tbs. water |
Mix thoroughly and peptonize at a temperature of 110° F. for 1 hour.
| 8 oz. milk | 3 eggs | 3 grains table salt |
| 8 oz. milk | 2 oz. glucose (grape sugar) |
| 125 gm. (about 4 oz.) milk | 1 or 2 egg yolks |
| 125 gm. (about 4 oz.) wine | Salt |
| 1 tsp. Witte’s peptone | |
| 250 c.c. (8 oz.) milk | 1 tbs. of red wine |
| 2 egg yolks | 1 tbs. “Kraftmehl” Health Flour |
| Small quantity of salt | |
| 6 oz. bouillon | 1 egg yolk |
| 4 oz. red wine | 1 to 2 tsp. dry peptones |
| 250 c.c. (about 8 oz.) milk | 70 grains starch |
| Dissolve 1 oz. of malted milk in 8 oz. of hot water |
| 1 egg and ½ tsp. salt or ½ oz. saline solution |
| 1 dram sodium chloride (common salt) | 1 pt. (16 oz.) water, (boiled) |
Makes 30 wafers.
| 2½ quarts washed bran (dry) | 1½ tsp. salt |
| 36 gms. agar-agar | 2 saccharin tablets (½ gr.) |
| 600 c.c. of cold water | |
[Pg 147] Mix agar-agar, saccharin, salt and water. Boil until dissolved. Pour over dry bran. Mix thoroughly and mold into muffin tins while hot. Bake in a slow oven about 20 minutes, or until wafer is dry and will whirl in the tin.
| 1 tsp. or 7 gms. agar-agar | ½ gr. saccharin |
| 1 cup cold water | ¼ tsp. flavoring |
| 1 tsp. mild citric acid | Coloring—as desired |
Dissolve agar-agar in water. Add citric acid and saccharin. Put over flame and boil. Remove from fire—add flavoring and coloring. Put in cool place to harden. This jelly has no food value.
| 3 gms. gelatin | 2 tbs. cold water, melt and swell over hot water. |
Add:
| 6 tbs. cold water | 50 gms. fresh cooked spinach |
| 2 tbs. vinegar | 1 hard cooked egg |
| Salt as desired | |
Surround mold with slices of hard cooked egg, placing the spinach in the center. Pour over this the gelatin mixture; allow to mold and serve on lettuce.
| 2 egg yolks | 60 c.c. vinegar |
| 360 gms. of salad oil | 8 gms. salt and pepper |
Beat egg yolks. Gradually add oil until all has been used (beating the mixture constantly). Then add the remainder of the ingredients. Put in a covered jar and keep in a cool place.
The percentage composition of this dressing is
Fat—83%. Protein—0.9%
| ½ cupful cellu flour | ½ teaspoonful salt |
| 1 cupful dry, washed bran | 3 tablespoonfuls mineral oil |
| 1 tablespoonful India gum | ½ grain saccharin |
| 1 teaspoonful baking powder | Hot water |
Makes 12 crackers about 4 inches by 4 inches and ⅛ inch thick (resembling Graham crackers).
Mix all dry ingredients. Add mineral oil and saccharin dissolved in a small amount of water. Then add sufficient hot water to make a soft dough. Spread on a baking sheet or in flat baking pans and cut into twelve wafers. Bake in a slow oven until dry.
These crackers have practically no food value.
Soya Manna may be secured from Vitae Health Food Company, 364 Roy Street, Seattle, Washington.
Soya Manna muffins may be substituted for hepco cakes in any of the following recipes:
(Recipe 41)
| 3 cupfuls bran, washed | 50 grams lard or crisco, melted |
| 2 eggs | 180 grams water |
| 2 egg yolks | ½ teaspoonful baking powder |
| ¼ teaspoonful salt | |
Mix ingredients in order given and bake in a moderate oven. This recipe makes 18 muffins. Food value of 6 muffins, 1 gram carbohydrate, 5 grams protein, 23 grams fat.
(Recipe 42)
| 2 eggs | 20 grams butter |
| 60 grams cream—20% | ½ teaspoonful baking powder |
| 140 grams Soya Manna | 100 grams water |
[Pg 149] Beat eggs, add cream and then flour, beating all the time. Add water and melted butter. Mold into 12 cakes and bake. Each cake contains 6 grams protein, 6 grams fat: approximately 75 calories.
(Recipe 43)
| ½ pint broth—clear | 5 grams butter |
| 1 egg noodle | Few grains salt and pepper |
Beat eggs until stiff and bake in 5 grams of butter as an omelet; let cool, cut into strips as noodles. Heat broth and add noodles. If desired, add vegetables, cut in cubes, using such variety and quantity as give flavor to soup adding their food value to diet. Food value 6 grams protein, 10 grains fat.
(Recipe 44)
| 50 grams chicken weighed cooked | 50 grams milk |
| ½ egg | 25 grams celery |
| Few grains salt and pepper | |
Beat egg slightly, add chicken, cut in small pieces, milk salt and pepper. Put in mold, set in pan of hot water and bake in moderate oven until firm. Food value 4 grams carbohydrate, 18 grams protein, 13 grams fat.
(Recipe 45)
| 75 grams steak—fat, weighed uncooked | 25 grams onion, uncooked |
| Few grains salt and pepper | |
Grind the meat, add seasoning and make into firm balls. Sear in hot mineral oil, then cook at a lower temperature. Food value, 2 grams carbohydrate, 17 grams protein, 22 grams fat.
(Recipe 46)
| 75 grams meat | 25 grams chopped celery |
| 2 Olmsted brancakes, crumbed | Few grains salt and pepper |
| 100 grams skim milk | |
Have meat cut in one thin slice. Use the trimmings chopped fine in dressing of crumbs, celery and seasoning moistened with water. Spread dressing on meat, roll and tie or skewer with toothpicks. Put in casserole and bake in milk until done. Food value, 6 grams carbohydrate, 23 grams protein, 19 grams fat.
(Recipe 47)
| 100 grams salmon | 2 tablespoonfuls vinegar |
| 1 egg yolk | Few grains salt |
| 5 grams butter | ½ teaspoonful gelatin |
| 50 grams skim milk | 1 tablespoonful cold water |
Remove the salmon from the can, weigh, separate in flakes. Add beaten yolks, melted butter, milk and vinegar and salt. Cook over boiling water, stirring constantly until mixture thickens. Soak gelatin, strain and add to salmon. Fill individual molds, chill, and serve with cucumber sauce. Food value, 3 grams carbohydrate, 26 grams protein, 23 grams fat.
(Recipe 48)
| 100 grams cabbage, cooked | 35 grams sour cream—16% |
| 15 grams lean meat, cooked, minced | 10 grams American cheese |
| 1 egg | Few grains salt and pepper |
Chop cabbage fine, add meat, cream, beaten egg, salt and pepper. Put into mould and sprinkle grated cheese [Pg 151] over top. Bake in a moderate oven until firm and brown. Food value, 5 grams carbohydrate, 15 grams protein, 17 grams fat.
| 50 grams milk | 1 egg |
| ½ hepco cake | 5 grams butter |
| 25 grams celery | Few grains salt and pepper |
Heat milk; add crumbed hepco cake, grated celery and seasonings, let come to a boil, add butter, remove from fire; add beaten egg yolk. Fold into beaten white. Put in ramekin and bake 20 or 30 minutes in slow oven until well browned. Food value, 3 grams carbohydrate, 11 grams protein, 15 grams fat.
| 50 grams onion, uncooked | 15 grams whole milk |
| 10 grams ground meat, lean cooked | Few grains salt and pepper |
Parboil the onion, scrape out the inside, leaving only shell. Weigh shell and scrapings to 50 grams. Add meat and return to shell. Put into casserole, add milk and bake until tender. Food value, 4 grams carbohydrate, 4 grams protein, 2 grams fat.
(Recipe 92)
| 1 egg | ½ teaspoonful cinnamon |
| 150 grams squash cooked | ¼ teaspoonful nutmeg |
| 50 grams cream—16% | Few grains salt |
| ½ grain saccharin | |
Beat egg, add mashed squash, cream, spice, salt and saccharin dissolved in 1 teaspoonful of cold water. Bake until firm in center, using cellu flour recipe for pie crust. Food value, 12 grams carbohydrate, 10 grams protein, 14 grams fat.
(Recipe 93)
| 2 eggs | 1 teaspoonful spices—cinnamon, cloves, nutmeg |
| ½ grain saccharin | 20 grams ground almonds |
| 10 grams cream—16% | |
Beat the yolks, add saccharin dissolved in cream, then spices and ground almonds. Add to the stiffly beaten whites. Drop from spoon on oiled pan and bake in hot oven. Food value, 4 grams carbohydrate, 16 grams protein, 25 grams fat.
| ¼ cup cauliflower purée | ¼ tsp. onion juice (if desired) |
| ⅔ cup chicken or beef stock | 2 tbs. 40% cream |
| Salt and pepper | |
Add cauliflower to stock, and allow to come to a boil, season and add cream. Serve at once.
| 1 cup creamed tomatoes | 3 cloves |
| ½ cup water | ½ tsp. salt |
| 1 sprig (1 tbs. chopped) parsley | ⅛ tsp. soda |
| 1½ oz. (3 tbs.) 40% cream | |
Cook tomatoes with cloves, parsley, and water for 20 minutes. Press through sieve and return to fire. Add soda; when effervescence ceases, add cream, and serve at once.
| 30 gm. cooked spinach | 15 c.c. 40% cream |
| 1 egg yolk | |
Cook spinach until tender and press through a sieve; add the broth; allow to cook about 5 minutes and add the well-beaten yolk and cream. Place the saucepan over hot water and cook 10 minutes. Season and serve at once.
[Pg 153] Other Cream Soups, except Tomato Bisque, are made by the same recipe.
The nurse must be governed in the selection of the vegetables by the physician, using those from the 5% group until otherwise ordered. These must be boiled in three separate waters to further reduce their carbohydrate content.
Cream or butter is added to them when diet permits; in the beginning (after starvation) only salt or (in case the vegetable is given in form of a salad) a little lemon juice with a little salt and pepper added.
Grated onion, a small quantity of celery seed, or a tiny bit of chopped green pepper may be added for additional seasoning. When some fats are allowed, butter, olive oil, and cocoanut cream may be used; the latter is prepared as follows:
1 small cocoanut grated; this is washed in cold water slightly acidulated with vinegar to remove the sugar, then washed to remove the vinegar. Over the washed cocoanut pour 1 pint of boiling water; allow to stand until cold enough to squeeze through a cloth; press as much of the water out as possible. Pour the water into a shallow dish and allow to stand until the cream rises; skim off and serve with lemon juice on salad as a dressing.
“A portion containing 50-75 grams meat and 100 grams of each vegetable makes an excellent meal.”
Horseradish (sauce) is recommended by Joslin as a seasoning, and some pickles made from group of 5% vegetables and without sweetening.
Curry powder, tarragon, bay leaves, capers may likewise be used in moderation to vary the monotony of the diet.
| 5 gm. butter | 1 tsp. chopped parsley |
| Salt, pepper, and ½ tsp. lemon juice, if desired | |
Cream butter, add lemon juice, salt, and pepper. Stir in parsley. Serve on meat or fish.
| ⅓ Neufchâtel cheese | 1 tbs. cream (40%) |
| ¼ green pepper | 1 tsp. lemon juice |
Season with salt and paprika and dress with cream dressing.
Mash cream cheese with fork; add tablespoonful chopped pecan nuts to ⅓ Neufchâtel cheese. Season with salt and pepper and dress with French dressing.
| ½ cup tuna fish | ½ cup chopped celery |
Dress with French Dressing.
Cook 1 egg hard. Cut into rings; arrange on lettuce leaf; dress with cream dressing.
| 1 cup canned tomatoes | ½ cup water |
| ½ cup celery (hearts) | ¼ cup vinegar |
| 1 tsp. celery seed | 3-4 cloves |
| ½ small onion | ½ bay leaf |
| 2 tsp. granulated gelatin, soaked in tbs. water | |
Boil all ingredients (except gelatin and celery hearts) 20 minutes. Measure. Add hot water or tomato juice to make one cup; add gelatin; allow to cool; cut celery fine, [Pg 155] place in mold; pour in the tomato aspic and allow to jelly in a cold place.
| 1 cup washed bran | 1 tbs. melted butter |
| 1 tsp. baking powder | 2 tbs. cream |
| 1 egg | ¼ tsp. salt |
Tie bran in cheesecloth bag and attach to cold water faucet; allow water to pass through bran, removing starch by squeezing the water through; using dry. Beat egg separately; add cream; mix with bran, add melted butter, salt, and baking powder. Grease muffin rings and pour in the mixture. Bake in moderate oven.
(The Equivalent of an Egg)
Recipe for Hepco Cakes, so arranged that one cake is equivalent to an egg:
| 140 gm. Hepco flour | Protein 60 | Fat 29 |
| 2 eggs | Protein 12 | Fat 12 |
| 60 c.c. 40% cream | Protein 2 | Fat 24 |
| 10 gm. butter | Fat 9 |
Make twelve cakes; each cake contains 6 grams of protein, 6 grams of fat, and approximately 75 calories.
So arranged that each muffin is equivalent to one egg:
| 60 gm. Lister flour (one box) | Protein 42 | Fat 0 |
| 1 egg | Protein 6 | Fat 6 |
| 45 c.c. 40% cream | Protein 2 | Fat 18 |
| 30 gm. butter | Fat 25 |
[Pg 156] Make 17 muffins; each muffin contains 6 grams protein, 6 grams fat.
(By F. M. Allen)
| 60 gm. bran | 6 gm. powdered agar-agar |
| ¼ tsp. salt | 100 c.c. (½ glass) cold water |
Tie bran in cheesecloth and wash under tap until water is clear. Bring agar-agar and water (100 c.c.) to boiling point. Add washed bran and salt and agar-agar solution (hot). Mold into ten cakes; place on oiled paper and let stand ½ hour, then when firm and cool, bake in moderate oven 30 to 40 minutes. The bran muffins are more palatable if butter and eggs are added. This may be done, provided the patient allows for them in the diet.
| 1 oz. (30 gm.) casoid flour | 1 egg white (whole egg may be substituted for 1 egg white) |
| 1 level tbs. (15 gm.) butter | |
| 1 oz. (30 c.c.) 40% cream | 1½ tsp. baking powder |
| ¼ tsp. salt | 1 cup washed bran |
Total food value: protein, 18 grams; fat, 24 grams; carbohydrates, 1 gram; calories, 300.
One muffin: protein, 3 grams; fat, 4 grams; carbohydrates, trace; and calories, 50.
The flours and meals used in this recipe are prepared by Cutlard, Stewart & Walt, Ltd., London (casoid flour). Theo. Metcalf & Co., Boston (soya bean meal). Lister Brothers, Andover, Mass. (Lister diabetic flour).
| 1 cup washed bran | 1 tbs. butter |
| 30 gm. Lister flour | 1 egg |
| 1 tsp. baking powder | ½ tsp. salt |
| 2 tbs. 40% cream | |
| Sufficient water to make a drop batter (about ¼ cup) | |
[Pg 157] Squeeze all the water from the bran, then add flour and melted butter, salt, well-beaten egg yolk and cream. Whip egg white stiff and fold into mixture. Add baking powder and enough water to make thick batter. Use less water if biscuits instead of muffins are desired, and knead into a dough. Roll out into a sheet one-half inch thick and cut with biscuit cutter.
After making muffin batter, grease muffin ring with melted lard, and pour half full of above mixture. Bake in moderate oven about 20 or 30 minutes.
| 1 oz. (30 gm.) soya meal | 1 cup washed bran |
| 1 level tbs. (15 gm.) butter | 1 egg white (one whole egg may be substituted for one egg white) |
| 1 oz. (30 c.c.) 40% cream | |
| ¼ tsp. salt | 1½ tsp. baking powder |
Mix soya meal, salt, and baking powder. Add to washed bran; add melted butter and cream. Beat egg white and fold into mixture; add enough water to make thick drop batter. Bake in six well-greased muffin tins until golden brown from 15 to 25 minutes.
Total food value: protein, 11 grams; fat, 27 grams; carbohydrates, 2 grams; calories, 304; one muffin, protein, 2 grams; fat, 4.5 grams; carbohydrates, trace; calories, 50.
| 1 cup almond meal | 1 grain (or less) saccharin, dissolved in 1 tsp. of water |
| 1 oz. cream | |
| 1 egg | 1½ tsp. baking powder |
| 3-4 drops vanilla | |
Beat egg yolk until light, add cream and saccharin; stir this into almond meal. Fold in the stiffly beaten white. [Pg 158] Drop on a greased paper and bake until golden brown in a moderate oven.
Almond meal or flour is prepared as follows:
Blanch 1 pound of almonds; dry and pass through grinder, or pound in mortar until powdered. Place in a muslin bag and immerse in a pan of water acidulated with vinegar to remove sugar; allow to stand 15 minutes. Squeeze dry and place in a warm (not hot) oven to remove all moisture. Grind or pound once more. Almond flour does not keep well; it must be made in small quantities and kept in a glass jar in a cool place.
Grate cocoanut and treat as almonds to remove sugar; dry thoroughly and grind or pound to fine meal.
| 1 cup cocoanut | 1½ tsp. baking powder |
| 1 egg white (or whole egg if desired) | ½ grain saccharin |
(A biscuit may be made without saccharin for bread substitute.)
| 5 tbs. coffee, or | 1 tbs. cold water |
| Infusion of cocoa nibs | 30 c.c. (1 oz.) 40% cream |
| 1 tsp. gelatin | 1 egg |
| Saccharin to sweeten | |
Pour coffee, or cocoa infusion, into a double boiler, beat egg yolk and saccharin dissolved in 1 tsp. of water, and stir into hot coffee. Cook gently until mixture coats the spoon (raw flavor of egg has disappeared); add gelatin and mix thoroughly. Whip cream and egg white. Place on ice to set.
This is made by pouring 30 grams of soft custard (diabetic) over 1 Lister biscuit.
| ½ cup cream | 1 egg |
| ¼ grain saccharin | 3-4 drops vanilla or almond extract |
Beat egg until it is well broken up, but not light; stir into the cream; dissolve saccharin in teaspoonful of water and add to mixture. If custard is to be baked, pour into molds and place upon a rack, or on a folded cloth in a pan half filled with hot water; bake in moderate oven until firm in center.
If soft custard is desired, pour mixture into double boiler and cook gently until mixture coats the spoon and the raw egg flavor has disappeared.
Make ½ cup gelatin, as directed below.
Whip in 1 egg white.
When gelatin is half congealed, mold and set on ice.
When ready to serve, unmold and serve with custard, or 1 tbs. whipped cream.
1 tbs. cold water to 2 tsp. granulated gelatin is used in making the following jellies:
16.6 calories
| ½ cup boiling water | ½ lemon or 2 tbs. juice and ½ rind sliced thin |
| ¼ to ½ saccharin tablet dissolved in 1 tbs. water | |
Carefully pick over and wash through several waters 1 tbs. Irish moss. Place in double boiler with ⅓ cup of water and 3 tbs. 40% cream and ¼ grain saccharin. Cook until mixture thickens when dropped upon a cold saucer. Pour over 1 stiffly beaten egg white; add 3-4 drops of vanilla extract. Mold and set on ice.
Irish moss may be used as a substitute for gelatin. The carbohydrates in this substance are not believed to be utilized for the manufacture of glucose in the human body.
54 calories
| ¼ cup boiling water | ¼ to ½ saccharin tablet dissolved in 1 tbs. water |
| ½ tbs. lemon juice | |
| ½ cup orange juice | 2 drops orange extract |
40.8 calories
| ½ cup boiling water | 1-inch piece of cinnamon |
| 3 tbs. sherry wine | ¼ to ½ saccharin tablet dissolved in 1 tbs. water |
| 1 tsp. lemon juice and the yellow rind from ¼ lemon | |
Soak gelatin in cold water about 2 or 3 minutes, then pour over it the boiling liquid; add saccharin and fruit juice, strain through cloth into wet molds. Set in cold place to stiffen; when firm, unmold. Serve with whipped cream, or pour liquid into baskets made from orange or grapefruit, hollowed out and the edges scalloped, or pour into shallow pans, and cut in ½-inch blocks when firm and serve on a bed of whipped cream.
Put water, wine, lemon juice and peel, cinnamon, and saccharin into a saucepan, allow to boil 5 minutes, pour over gelatin (which has been soaked in cold water). If the jelly looks cloudy, return to saucepan, and add ½ egg white beaten stiff; allow to boil 1 minute, stirring constantly, and strain into mold. Serve with whipped cream.
30 calories
| ⅓ cup water | ¼ to ½ saccharin tablet |
| Fruit juice, 1 lemon | 1 egg white |
75.5 calories
| ½ cup water | ½ lemon |
| 1 large or 2 small oranges | ¼ to ½ saccharin tablet |
| 1 egg white | |
Sweeten fruit juice with saccharin instead of sugar. Clip egg white with scissors, or beat with Dover egg beater, add mixture and freeze.
(1) Use recipe for soft custard, freezing after the custard has become thoroughly cold.
| (2) ⅓ cup cream | ¼ grain saccharin or enough to sweeten, dissolved in 1 tsp. water |
| 1 tbs. chopped nuts | |
| 3-4 drops vanilla, orange, or almond extract | |
Whip cream, add saccharin and nuts. Pour into a small ¼-pound baking powder can, seal the edges of mold or can [Pg 162] with a thin strip of buttered muslin. Pack in equal parts of salt and ice for two hours.
Sugar-free Milk.—A sugar-free milk has been advised by Williamson. It is made from washed cream as follows: 3 tablespoonfuls of cream are shaken in a pint of water and set aside until the cream rises, it is then skimmed off and mixed with the white of one egg and diluted with pure water. This furnishes a beverage not unlike milk in appearance and flavor.
| 60 c.c. (2 oz.) 40% cream | Saccharin to sweeten |
| 30 gm. chopped walnuts | 3-4 drops vanilla |
Whip cream stiff; add saccharin, nuts, and vanilla.
1 tbs. sherry wine and 1 tsp. gelatin soaked in 1 tbs. cold water and melted over hot water may be substituted for vanilla to vary the above recipe.
| 75 c.c. (5 tbs.) orange juice | 1 tsp. gelatin |
| 45 c.c. (3 tbs.) 40% cream | 1 tbs. cold water |
| ½ egg white | Saccharin to sweeten |
Soak gelatin in cold water; dissolve over hot water, add to orange juice; add saccharin; set aside until it begins to jelly. Whip cream and add to partially jellied orange juice; fold in the stiffly beaten egg white; mold. Serve 30 grams.
[43] When a 1.50% decoction is desired, use 2 rounded teaspoonfuls to the pint of water. “Diseases of Nutrition and Infant Feeding,” p. 222, by Morse and Talbot.
[44] “Beef juice is not the same as ‘dish gravy,’ since the latter contains a large amount of cooked fat and is often highly indigestible.” Morse and Talbot’s “Diseases of Nutrition and Infant Feeding.”
[45] Formula suggested by Finkelstein and Meyer.
[46] “Diet in Disease,” by Freidenwald and Ruhräh and other sources.
[47] Formulas marked with one star are those used in the Presbyterian Hospital, Chicago, Ill. Courtesy of Miss R. Straka, Dietitian. Formulas marked with two stars are used in the Olmsted Hospital, Mayo Clinic, Rochester, Minn. Courtesy of Misses Foley and Ellithorpe, Dietitians. Formulas unmarked are used by the author in Memphis General and St. Joseph’s Hospitals, Memphis, Tenn.
[48] “Treatment of Diabetes,” p. 538, by Joslin.
[49] “The Treatment of Diabetes Mellitus,” p. 531, by Joslin.
[50] “Starvation Treatment of Diabetes,” p. 43, by Hill and Eckman.
Chemical Composition of the Body.—It has been estimated by various writers that the human body has an approximate average chemical composition[51] of—
| Oxygen | about 65.000 per cent | |
| Carbon | about 18.000 per cent | |
| Hydrogen | about 10.000 per cent | |
| Nitrogen | about 03.000 per cent | |
| Calcium | about 02.000 per cent | |
| Phosphorus | about 01.000 per cent | |
| Potassium | about 00.350 per cent | |
| Sulphur | about 00.250 per cent | |
| Sodium | about 00.150 per cent | |
| Chlorine | about 00.150 per cent | |
| Magnesium | about 00.050 per cent | |
| Iron | about 00.004 per cent | |
| Iodine | ||
| Fluorine | very minute quantities | |
| Silicon | ||
Dependence of the body upon Food.—The human body, like any other piece of machinery, undergoes a constant wear and tear incidental to the work it performs, but in the human machine this is not all that must be included in its upkeep. The replacing of the dead and cast out cells with new ones, the repairing of the worn cells, the furnishing of heat, not only for the running of the engine but for the maintenance of the body temperature,—all of these must be considered and cared for if life is to continue. In man-made machinery, the renewal of the worn parts, and the replacing of those no longer useful must be accomplished by an outside agency. But in the body this work is [Pg 166] performed by the organism; and the material used for the purpose, as well as that which is used to furnish the heat necessary for the internal and external activities of the body is food.
Exceptions to this Rule.—Under normal conditions the body never uses its own structure either for fuel or to replace tissue losses. In starvation the body rebuilds its important tissues, such as the nerves and glands, at the expense of the less important ones, such as the connective tissues and the skeletal muscles (Taylor).
Science has proved that for the most part the body does not use the food materials in their original form, but carries them through a series of transformations into substances more easily handled by the organism.
Roughly speaking, we may say that the body carries the foodstuffs through practically four processes on the pathway through the body, namely, digestion, absorption, metabolism, elimination.
Processes Included in Digestion.—There are several processes concerned in this transformation of the food materials. Some are purely mechanical and have to do with the movement of the food mass through the digestive tract: others are of a chemical character and bring about distinct changes in the food materials themselves. These mechanical and chemical processes with the retarding and stimulating agents that influence them are called digestion.
Absorption.—After the food materials have undergone digestion, or simplification into more available substances, these substances are absorbed, that is, they are passed through the membranes lining the walls of the intestinal tract, and thence to the blood.
Metabolism.—The utilization of the transformed food materials and their final fate in the human body is included under the term Metabolism.
[Pg 167] Elimination.—After the food materials have been utilized to the extent of the body’s ability to handle them, their waste products are cast out of the organism by way of the skin, the lungs, the intestines and the kidneys.
A brief description of these processes seems desirable here.
Digestion.—Mechanical digestion begins in the mouth, where through the action of the teeth, the tongue and the muscles of the jaw, the food material is ground up and liquefied to a certain extent and made ready for the chemical action which takes place, to a limited degree only, as a result of the salivary enzyme in the mouth. The eating of food causes a flow of saliva from the three pairs of large salivary glands, and from the numerous secretory cells situated in the membranes of the mouth. As a rule the food stays for too short a time in this organ for any appreciable amount of chemical action to take place, but the liquefaction of the food mass with the salivary juices which contain the ferment (ptyalin), prepares for its passage into the gastric organ, and allows the digestion of the starch (the only foodstuff affected by salivary digestant), to continue in that part of the stomach until its action is checked by the hydrochloric acid in the gastric juice.
Arrangement of Food in the Stomach.—To simplify the study of the gastric organs it may be well to think of the stomach as being divided into three regions, i.e., “the fundus, the middle region, and the pyloric end,”[52] each of which differs slightly from the other. After being swallowed, the food enters the region situated at the cardiac end, known as the fundus.
Motor Processes in the Stomach.—There are no peristaltic waves in the fundus of the stomach, and the movement of the food mass is accomplished through the stretching and contraction of the muscular walls of the organ [Pg 168] which tends to churn and further mix it with the salivary juices as it is gently pushed out into the middle region. In this region the peristaltic waves begin and travel toward the pylorus and increase in force as digestion progresses, ceasing only with the emptying of the organ. When the first stratum of food reaches the middle of the stomach it is caught by these oscillating peristaltic waves and forced forward through the pyloric region and against the pylorus, from whence it is returned back through rings of constriction. This forward and backward movement continues as long as there is food in the stomach, thus thoroughly mixing the mass with the gastric juice and allowing the enzymes existing in the juices to have an opportunity for action (chemical digestion).
Passage of Food from Stomach.—The material prepared in the stomach, known as chyme, is passed into the duodenum through the pylorus. The opening of this sphincter is controlled, according to Cannon, to a certain extent by the liquefication of the chyme, but more especially by the presence of free acid in the stomach side of the pyloric orifice.
Behavior of Food in the Intestines.—The food does not pass at once along the canal, but waits in the duodenum until several portions have passed through. As the food mass is made alkaline in the presence of the intestinal juices, the pyloric valve closes, opening again as the contents nearest it on the stomach side are acidified.
Intestinal Movements.—The peristaltic waves in the small intestines begin in the upper part and start a course ever downward. These waves in the intestines are two-fold in character; the quick shallow wave which forces the food string forward, breaking it up into segments, and backward joining the segments together again, and the strong deep wave which carries the entire mass forward after each segmentation. This method of movement in the small [Pg 169] intestines is the best one possible under the conditions which prevail in this region of the digestional apparatus, since it not only mixes the food material with the juices necessary for its digestion, but likewise spreads it out over a wide space, insuring a greater contact with the absorbing walls of the small intestines.
The Effect of Muscular Constrictions.—The muscular constrictions occurring in the intestines producing segmentation of the food string have, according to Sherman, the effect of “(1) further mixing of the food and digestive juices, (2) bringing the digested food into contact with the absorbing membrane, (3) emptying the venous and lymphatic radicles in the membrane, the material which they have absorbed being forced into the veins and lymph vessels by the compression of the intestinal walls.”[53]
Movements in the Large Intestine.—The movements in the large intestine or colon are much like those in other parts of the digestive tract. The small and large intestine are divided by a valve known as the ileocecal valve, and any food which passes through it cannot return, since the valve is a competent one. The cells in the walls of the larger intestine secrete fluids of a lubricating character, containing no enzymes of digestion but aiding in moving the fecal matter toward the rectum.
Distribution of Secretory Cells.—Secretory cells are distributed in each of the three regions of the stomach, but are more numerous in the middle region than at either end. The third region includes the pyloric vestibule through which all foods must pass before they can enter the small intestine, and terminates in the pylorus, the valve which shuts off the stomach from the duodenum and the rest of the intestinal canal.
Chemical Digestion.—The chemical changes in the food materials, after they are eaten, are brought about [Pg 170] through the action of certain substances known as soluble ferments or “enzymes.” These enzymes exist in every tissue of the body, and their province is first to break down the food materials themselves into simpler compounds, and then to reconstruct the simpler substances into those of a more complex character, which are more available for the various uses of the organism.
Action of the Enzymes.—As Sherman has stated, “all fermentation is brought about either directly or indirectly by the activity of animal or vegetable organisms or cells. When the organisms or cells act directly and the chemical changes occur only in their presence, the fermentation is said to be due to an organized ferment. When the action is not brought about directly by the cell itself, but by means of a substance secreted by the cell but acting apart from it, this substance is called a soluble or unorganized ferment or ‘enzyme.’” The enzymes concerned in digestion and metabolism, their source and their action, may be found in the following table:
| Enzymes | Where chiefly found | Action | |||
| Act upon carbohydrates | Ptyalin (salivary amylase) | Salivary secretions | Converts starch to maltose | ||
| Amylopsin (pancreatic amylase) | Pancreatic juice | Converts starch to maltose | |||
| Liver diastase | Liver | Converts glycogen to glucose | |||
| Muscle diastase | Muscles | Converts glycogen to glucose | |||
| Invertase (sucrase) | Intestinal juice | Converts glycogen to glucose and fructose | |||
| Maltase | Intestinal juice | Converts maltose to glucose | |||
| Lactase | Intestinal juice | Converts lactose to glucose and galactose | |||
| Glycolytic enzymes | Muscles, etc. | Split and oxidize glucose | |||
| Acts on fats | Lipase (steapsin) | Gastric, and pancreatic secretions, blood and tissues | Splits fats to fatty acids and glycerin | ||
| Act on proteins | Pepsin | Gastric juice | Splits proteins to proteoses and peptones | ||
| Trypsin | Pancreatic juice | Splits proteins to proteoses, peptones, polypeptids and amino acids | |||
| Erepsin | Intestinal juice | Splits peptones to amino acids and ammonia | |||
| Autolytic enzymes | Tissue generally | Split body proteins to simpler substances | |||
| Act on purins | Guanase | Thymus, adrenals, pancreas | Changes guanin to xanthin | ||
| Adenase | Spleen, pancreas, liver | Changes adenin to hypoxanthin | |||
| Oxidases | Lungs, liver, muscles, etc. | Changes hypoxanthin to xanthin and to uric acid | |||
[Pg 172] Classification of Enzymes.—Sherman classifies the enzymes of the body according to their effects:
1. The hydrolytic enzymes:
(a) Proteolytic or protein-splitting enzymes.
(b) Lipolytic or fat-splitting enzymes.
(c) Amylolytic or starch-splitting enzymes.
(d) Sugar-splitting enzymes.
2. The coagulating enzymes, such as thrombin or thrombase (the fibrin ferment) and rennin, which causes the clotting of milk.
3. The oxidizing enzymes or oxidases (which, if the oxidation be accompanied by a splitting off of amino groups, may be called “deaminizing” enzymes).
4. The reducing enzymes or “reductases.”
5. Those which produce carbon dioxide without the use of free “deamidizing” oxygen, such as zymase of yeast.
6. Enzymes causing the breaking down of a larger into a smaller molecule of the same composition, as in the production of lactic acid from glucose.
Salivary Digestion.—The table shows that enzymic action begins in the mouth. Saliva, the characteristic secretion of this region, contains the enzyme ptyalin which exerts its influence upon the starches and dextrins. The food mass remains in the mouth for so short a time, however, that a very small percentage of the starch is changed to maltose under salivary digestion. The action of ptyalin, however, continues in the fundus of the stomach until stopped by the acid in the gastric juice.
Gastric Digestion.—The conditions existing in this region of the gastric organ of digestion are particularly favorable to the continuance of salivary digestion on account of the neutral character of the juices secreted by the cells there, and because there is so little movement taking [Pg 173] place. The cells in the middle region, however, secrete a fluid rich in acid, and as the food mass is gradually pushed forward by the contraction of the stomach walls into this portion of the stomach, further conversion of starch and dextrin to maltose is checked. Gastric juice is secreted by cells situated in all parts of the stomach. The character of the secretions differs in different parts of the organ. However, that in the fundus is neutral in character or even slightly alkaline, according to Howell, while that in the middle region is highly acid. The pyloric end of the stomach exhibits strong peptonizing powers and much of the hydrolysis of protein takes place here. As the food is pushed out of the fundus it is caught by the waves of peristaltic action and swept toward the pylorus. This movement of the food mass to and from the pylorus under the influence of the muscular constriction in the stomach tends to mix it thoroughly with the juices in all parts of the stomach, and in a measure to liquefy it to the “souplike” mixture known as chyme.
Rate of Carbohydrates, Proteins, and Fats.—Carbohydrates, for example, do not require any acid for their digestion, hence all of the acid with which they come in contact can go toward acidifying them, while the proteins require hydrochloric acid before the enzymes can begin to exert their activities. Consequently they leave the stomach much more slowly than the carbohydrates. The fats leave more slowly than any of the other food combinations. If carbohydrates and proteins are taken together they leave the stomach more slowly than if the carbohydrates were fed alone, but more quickly than they would if the meal consisted of protein alone. When the meal consists of fats and proteins, the stomach is emptied more slowly than is the case when either is fed alone.
Intestinal Digestion.—Digestion proceeds in an orderly manner throughout the intestinal canal. The [Pg 174] pancreatic juice, bile, and intestinal juice are poured upon the food mass on its entrance into the duodenum. The enzymes work simultaneously. Trypsin in the pancreatic juice takes up the hydrolysis of the proteoses and peptones and those proteins which have escaped gastric digestion. The amylopsin likewise in the pancreatic secretion acts upon the starch and dextrin, changing them to maltose. The lipases split the fats to fatty acids and glycerol.
The erepsin in the intestinal juice, “succus entericus,” brings about further change in the proteins, with the production of amino acids. The bulk of the carbohydrates are converted into monosaccharids in the small intestines. The lactose, maltose, and sucrose are changed through the activity of the lactase, maltase, and invertase into glucose. Sherman states that “it is possible that the splitting of the lactose (milk sugar) may occur in the intestinal wall rather than in the food mass.”[55]
Bile.—Human bile, the secretion most actively concerned in the digestion and absorption of the fats, contains water, bile salts, bile acids, bile pigments, cholesterin, lecithin, and a peculiar protein derived from the mucous membranes of the bile ducts and gall bladder.
Stimulation of Intestinal Secretions.—The flow of the intestinal juices is stimulated by a substance or hormone known as “secretin.” This hormone is the result of the action of hydrochloric acid upon some substance in the intestinal wall. Starling claims that the formation of hormones and their circulation through the blood to the reactive tissues is sufficient to account for the activity of the pancreas; he doubts if the nervous system plays any part in the activity of that organ.
Secretion of Water in the Stomach.—The secretion of water by the cells of the stomach is such, according to [Pg 175] Taylor, as to produce chyme of quite constant consistency, the solid particles being held in suspension in the fluid medium.
Factors Influencing Gastric Digestion.—The factors influencing digestion in the stomach constitute all those mechanical, electrical, chemical, and psychical factors which stimulate or retard the action of the gastric juices. The movements in the stomach are involuntary, but their activities may be stimulated by the flow of gastric juice. Sleep retards digestion in the stomach by retarding the movements in the organ itself.
Stimuli to Gastric Flow.—The division and liquefaction of the food in the mouth hastens gastric digestion by making the food better fitted for the action of the enzymes in the gastric juice. The type as well as the character of the food acts as a stimulus to the gastric secretion.
Water is probably the best of all the agents for stimulating the secretion of gastric juice, while dextrin (toast, zwieback) and the extractives of meat likewise exert similar powers.
Retarding the Gastric Flow.—The nervous system, on the other hand, at times checks or entirely inhibits a flow of these juices. Worry, excitement, anger, fatigue, chill; each plays its part in promoting poor digestion in the gastric organ. As chemical factors, water and salts are the two necessary substances for gastric digestion, since the enzymes in the juices cannot act except in their presence.
Alkaline carbonates and fatty foods both check the flow of gastric juice, and retard digestion. The psychic factors which result in a stimulation of the secretory cells in the stomach are exerted through the sight, smell, and taste. One often hears the expression: “The food looked, smelled, or tasted so good that it made my mouth water.” This actually occurs; hence the secretion has been named appetite juice. This appetite juice acts as a direct stimulant [Pg 176] to the cells in the mucous lining of the stomach, causing a flow of gastric juice. It cannot be said to cause digestion, but it certainly institutes that process, thus starting the whole digestional procedure.
Digestion in the Larger Intestine.—Science has proved that most of the nourishing part of the food ingested is digested and absorbed before it reaches the larger intestine. The two portions of the alimentary canal known as the small and large intestine are separated by the ileocecal valve. Cannon claims “that this valve is competent, that is, under normal conditions the food mass which passes through into the colon cannot be forced back into the small intestine.” The food mass sometimes contains materials which have escaped digestion, likewise some of the active enzymes which bring about their hydrolysis, in which case a certain amount of their digestion may continue in the large intestine.
So far, investigators have found no enzymes in the fluids secreted by the cells in the walls of the large intestine, but they have found an alkaline fluid which assists in completing the digestion of the foods which has started in other parts of the intestinal tract.
Absorption.—Absorption of food occurs in all parts of the intestinal canal, but the major portion of it occurs in the small intestines, the mucous membrane lining of which seems particularly adapted for this purpose. According to Taylor there is no absorption of fats, carbohydrates, or proteins in the stomach. Other investigators believe that some of the protein is absorbed and also some glucose in concentrated solution. However, the stomach cannot be considered of great value as an absorbing organ. Physiology teaches that the absorption of the products of digestion occurs by means of the millions of small projections or villi with which the intestinal wall is lined. These villi contain numerous capillary blood vessels and spaces known as [Pg 177] lacteals. The former converge into the portal vein, the latter into the lymphatic vessels and thence into the thoracic ducts.
The Absorption of Fat.—The fats, as has been described, are split into their two constituents, fatty acid and glycerol. The former is dissolved by the bile to form soap; the latter is readily soluble in water. These constituents thus dissolved pass through the walls and recombine in the form of neutral fat droplets, probably during the passage through the walls, since they appear in this form in the cells. They pass into the thoracic duct and thence into the blood stream.
Absorption of Carbohydrates.—The carbohydrates are chiefly absorbed in the form of monosaccharids. This has been proved by introducing cane sugar or lactose into the blood vessels and getting the greater portion of it back unchanged by way of the urine. As the monosaccharids are taken up by the capillaries lining the walls of the small intestines, they are passed on to the portal vein and carried by the portal blood into the liver, where they are stored temporarily as glycogen, and given out to the blood in the form of glucose as needed. After a meal rich in carbohydrates, the portal blood will be rich in glucose, while the blood in general circulation contains about the same amount as usual, about 0.1%.
Absorption of Proteins.—The absorption of the products of protein digestion occurs through the capillary blood vessels and passes on to the portal vein. The metabolism of protein is more complex than that of any of the foodstuffs. It is probable that each living cell contains enzymes which are capable of breaking down the body proteins with the production of amino acids just as the proteins of the food are broken down by enzymes of digestion, and according to Sherman “it is not improbable that protein synthesis also may be brought about by every living cell.”
The Absorption of Water.—This does not occur in [Pg 178] the stomach, as was formerly believed, but in the small intestines.
The Absorption of the Mineral Salts.—This occurs in conjunction with the other food material. Some of the mineral salts are much more soluble than others and are more readily absorbed. The function of the mineral salts in the body has already been described, and since they form a part of every tissue and fluid in the body their absorption and fate in metabolism must be studied with that of the other chemical combinations.
The digestion of the food as it is passed into the last portion of the alimentary canal has been largely completed. However, that part which has escaped digestion in the small intestine is finished and absorbed here. The important peristaltic waves occurring in this region are antiperistaltic in character and have the property of churning the food thoroughly and bringing a larger portion of it in contact with the absorbing walls. The water which is left in the food mass together with the products of the digestion of the foodstuffs is absorbed in the first part of the large intestine, leaving the remainder more solid. This residue is known as feces or fecal matter.
The diagram on page 179 shows the various processes through which the foodstuffs pass after absorption.[56]
Bacterial Action in the Alimentary Canal.—The changes in the foods so far mentioned have been chiefly the result of the activity of the enzymes existing in the various digestive processes throughout the body. But there are other changes which occur in the foods during their sojourn in the digestive tract which are not accountable to enzymic [Pg 179] action, but which, in fact, modify to a certain degree the changes wrought by the enzymes. These are the result of the activity of certain specific bacteria which inhabit the entire digestive tract of the individual from a few hours after birth until death. Some of these have so adapted themselves to the existing conditions that, unless present in overwhelming numbers, they are not only harmless, but they actually assist in protecting the organism from the inroads of more harmful species. Many experiments have been made to find whether or not bacteria are essential to human nutrition, and the results of these experiments prove that they are not. However, since they are so firmly established in the body it is well to study the various types and learn as much as possible of the products of their activity and the influence which they exert in human nutrition.
Types of Bacteria.—It would be impossible and unnecessary to consider the action of all of the bacteria in the body in this text, but it is necessary to consider those which are prominent in bringing about decomposition of the foods in the digestive tract. Sherman holds that there are three main types having this property: “(1) the bacteria of fermentation, such, for example, as the lactic acid bacteria; (2) the putrefactive bacteria, such as the anaërobic B. aërogenes capsulatus; (3) bacteria of the B. coli type, showing [Pg 180] the character of both the fermentative and putrefactive organisms but tending in general to antagonize the putrefactive anaërobes.”[57]
Fermentation in the Stomach.—In the stomach, fermentation of the carbohydrates with the production of organic acids, and at times alcohol, occurs. The types of fermentation taking place in the stomach are alcoholic, lactic, butyric, acetic, formic, oxalic, and cellulose. The bacteria inhabiting the gastric organs are dependent upon air for existence, while those in the intestines are not.
Factors Influencing Excessive Fermentation.—The factors influencing excessive fermentation in the stomach are lack of “tone” and motility in the organ, insufficient amount or absence of free hydrochloric acid in the gastric secretion, dilatation of the stomach, and an excess of carbohydrate foods in the diet. Of the latter, sucrose and glucose are especially susceptible to the action of fermentative bacteria. Under normal conditions, that is, in health, the conditions prevailing in the stomach are very unfavorable to the development of bacteria of the putrefactive type, the gastric juice exhibiting decided germicidal properties. Then, too, the presence of air acts against their development. Much of the so-called gastric fermentation does not occur in the stomach but rather in the duodenum.
Bacterial Action in the Intestines.—In the lower part of the small and in the large intestines, the bacteria of the anaërobic type increase, conditions more favorable to their development existing there than farther up in the intestinal tract. However, there are a great many bacteria in the whole of the small intestine. Those producing decomposition of the unabsorbed proteins are especially prominent in the colon.
Herter[58] states that “the presence in the colon of [Pg 181] immense numbers of obligate micro-organisms of the B. coli type may be an important defense of the organism in the sense that they hinder the development of that putrefactive decomposition which, if prolonged, is so injurious to the organism as a whole. We have in this adaptation the most rational explanation of the meaning of the myriads of colon bacilli that inhabit the large intestine. This view is not inconsistent with the conception that under some conditions the colon bacilli multiply to such an extent as to prove harmful through the part they take in promoting fermentation and putrefaction.”
Effect of Bacterial Activity in the Body.—In summarizing the effects of bacterial action in the body it is found that with the exception of oxalic acid, which is exceedingly injurious, and which, according to Herter, results from the eating of large quantities of meat and sugar, the products of fermentation are simply irritating in character, while those resulting from putrefaction are distinctly toxic. Among the substances deserving mention under this head we have indol, skatol, cresol, and phenol. These substances are very soluble and upon absorption combine with the sulphuric acid formed in the body and are excreted by way of the kidneys where they appear in the urine as “conjugated sulphates,” the chief of which is indican. The amount of indican in the urine is taken as a measure of the intensity of the putrefaction taking place in the body.
Metabolism.—Under the term metabolism we understand the series of processes through the foodstuffs and carried (a) in the conservation of the tissues of the body and (b) in the maintenance of body temperature and physical work (Taylor). The processes concerned in metabolism are chiefly those of building up, “anabolism,” and breaking down, “catabolism.” In the processes of anabolism the products absorbed are built into the tissues and cells of the body. In catabolism, the worn particles from the cells, [Pg 182] and the dead cells no longer useful are broken up and thrown out of the body. According to Taylor, “side by side with these processes are the reactions of combustion, whereby the temperature necessary for the life of the cells is maintained, and the energy needed for external work furnished.”
Behavior of Carbohydrates in Metabolism.—As Sherman[59] has said: “At least two kinds of enzymes are believed to be involved in the combustion of glucose in the tissue cells, (1) cleavage enzymes, which split the molecule into fragments more easily oxidized, and (2) oxidizing enzymes or oxidases which stimulate the oxidation of the cleavage products. Both kinds of enzymes are widely distributed through the body and are believed to be normal constituents of all active cells.”
Production of Energy.—It has been proved that the energy for external and internal work is produced largely from the glucose brought by the blood and oxidized in the muscles.
When a surplus amount of carbohydrate food is eaten, over and above the immediate needs of the body for fuel, it is stored in the liver and muscles as glycogen, which can be readily reconverted into glucose. When the supply of carbohydrate food is greatly in excess of the body’s needs, that is when the liver and muscles cease to store glycogen, it is built up into adipose tissue and furnishes a readily available source of emergency fuel.
Fate of the Carbohydrates.—After their oxidation the end products of carbohydrates, that is, the substances which are no longer available for use in the body, leave it in the form of carbon dioxide and water by way of the kidneys (urine), the skin, the lungs, and the intestines.
Fate of the Fats.—The fats upon absorption are taken [Pg 183] up by the lymph vessels instead of the capillaries and enter the blood with the lymph. According to various investigators, the fat which causes the turbidity of the blood plasma at the height of absorption will, as a rule, disappear after a few hours, part of it being burned as fuel, producing energy for the internal and external work of the body, and at least a part of the fats eaten being rebuilt into body fat. The end-products of fat metabolism, like those of the carbohydrates, consist of carbon dioxide and water, and leave the body by the same excretory channels.
When the normal oxidation of the fatty acids is interfered with or is overtaxed, a different reaction from that which usually occurs may take place, and this results in an excretion of acetone in the urine (see Chapter on Diabetes).
Protein metabolism is certainly more complex than that of either of the other active organic food groups. The amino acids which are the products of protein digestion are taken up by the capillary blood vessels in the intestinal walls and are passed by them into the portal vein, soon to become available for the needs of the body.
Fate of the Proteins.—After utilization in the body, the proteins, like the other foods, leave certain waste products which indicate to a greater or lesser extent the completeness with which the organism has made use of the food materials. The end-products of protein metabolism are: urea, ammonium salts, purin bodies, and creatinin. These products leave the body chiefly in the urine. The chief end-product in man is urea. This substance represents from 82-88% of the total nitrogen excreted by the kidneys. However, the less highly oxidized products represent the incomplete products of protein metabolism and thus indicate the changes through which these products must pass before being changed into urea. If for any reason there is [Pg 184] an impairment of the liver through which they must pass and where the change into urea is accomplished, there will be a rise of ammonia and a corresponding decrease in the output of urea in the urine. Thus, ammonia is formed at the expense of the urea. This occurs in fevers, diabetes, and certain structural diseases of the liver. According to Sherman:[60] “Normally about 2 to 6% of the total nitrogen eliminated is in the form of ammonium salts, the amount depending largely upon the relation between the acid-forming and base-forming elements in the food.”
Acid-forming and Base-forming Foods.—Mendel[61] states: “There are foods which act as potential acids and others which function as bases in the organism. When burned up either in the laboratory or in the body cells, they have a preponderance of acid or base, as the case may be, in their ash.” In this respect potatoes, apples, raisins, and cantaloupes, for example, are base-forming foods which depress the output of ammonia and increase the solubility of uric acid in the urine, whereas meal, cereals, and prunes (the latter with their content of benzoic acid) furnish acids in predominance.
Purin Bases.—These compounds are formed in the body as cleavage products of nucleoproteins or taken into the body in food. The chief of these products are adenin, guanin, hypoxanthin, xanthin, and uric acid. The latter is the most highly oxidized of all the purin bases and is the form in which they are chiefly eliminated in the urine.
Formation of Uric Acid.—The formation of uric acid can in a measure be controlled by attention to the diet, eliminating those foods known to be purin-bearing. Normally from 1 to 3% of the nitrogen eliminated will be in the form of uric acid. The normal human being [Pg 185] oxidizes about half of the purins eaten and excretes about half, mainly in the form of uric acid. According to Mendel, the formation of uric acid takes place throughout the body, and its partial destruction is accomplished by the kidneys, muscles, and liver. The formation of purins in the body and their elimination in the form of uric acid is especially significant in certain pathological conditions, gout, for example, in which the body has difficulty in eliminating these compounds.
The purin bodies are both endogenous and exogenous—that is, they may be brought into the body in food as such, or they may be formed as a result of the metabolism of the body tissues. For this reason the damage wrought by these substances may to a certain extent be controlled by eliminating the purin-bearing foods from the diet. Flesh-foods are high in purins, especially the highly nucleated glandular organs, liver, thymus (sweetbreads), etc., kidney, beef, mutton, veal, pork, chicken, turkey, goose, sardines, anchovies, all kinds of fish except cod. Among the vegetable foods asparagus, beans, peas, and spinach are highest in purins. Boiling extracts much of the purins from food. Meat especially should be prepared by this method, if used in the diet of individuals suffering from gout. Eggs and milk are purin free, and may be used freely. Certain substances increase the difficulty of eliminating uric acid. Alcoholic beverages for example are especially deleterious.
Creatinin.—This end-product of protein metabolism is, like uric acid, endogenous and exogenous. It is one of the normal constituents of the urine. The quantity is fairly constant for the individual, averaging about 0.02 gram per kilogram of body weight per day.
Mineral Metabolism.—A study of the organic foodstuffs reveals the fact that many of the mineral salts concerned in nutrition enter the body in organic combination with those constituents. Certain of the mineral salts, [Pg 186] however, enter, exist in and leave the body in the same organic form in which they occur in the food materials. This is true of chlorine, which for the most part, functions in and leaves the body in the form of chlorides (chiefly sodium chloride). A small part of the chlorine is used in the production of the hydrochloric acid of the gastric juice.
Sulphur and iron, both enter the body as essential constituents of proteins, and their metabolism occurs with that of these foodstuffs; the sulphur being converted largely into sulphuric acid must be neutralized at once, and it leaves the body by way of the urine as inorganic sulphates. Part of the sulphates are excreted as ethereal (conjugated) sulphates; the amount excreted in this form depending largely upon the extent of purification in the intestinal tract.[62]
Phosphorus.—This mineral salt is found to be present as an essential constituent of certain proteins, fats and carbohydrates. It also enters the body in the form of inorganic phosphates. During the digestion and metabolism of the organic foodstuffs the phosphoric acid radical is split off and eventually nearly all of the phosphorus leaves the body in inorganic form (inorganic phosphates).
Calcium.—Being the chief constituent of the bones, large quantities of calcium salts are stored in the skeleton of the child both before and after birth. The functions of calcium have already been discussed. That part not stored, which has finished its work in the body is excreted through the intestinal wall and leaves the body by way of the feces, only a small part of the calcium concerned in metabolism being excreted in the urine.
The Process of Osmosis in the Body.—The influence exerted upon the process of osmosis in the body is one of the most important parts played by the mineral salts in [Pg 187] metabolism. The fact that these chemical substances are indispensable to the metabolic processes makes it necessary for the nurse to know where they can be found in food and how best to use them.
Metabolism of Body Tissues.—The constant breaking down and building up of the tissues of the body and the evolution of heat as a by-product of the energy expended may be summed up in the term “metabolism.” The metabolism of the body is normally supported by the food ingested. However, it is a known fact that were no food eaten the processes would continue just the same, the difference only being the use of the body structure instead of food materials. According to Sherman, the chemical changes and energy transformations are of course inseparable. It has become customary to speak of the metabolism of matter and the metabolism of energy, and to regard the extent of the metabolism of any material substance as measured by the amount of its end products eliminated, and the extent of the energy metabolism as measured by the amount of heat or of heat and external muscular work which the body gives off.
In summarizing the important factors in the utilization of food by the body several distinct points are made evident:
1. The composition of the body, and the composition of food, are practically the same.
2. Food must make good the losses resulting from metabolic processes and physical activity.
3. Utilization of food by the body necessitates:
(a) Transformation through a series of processes:
(1) Digestion.
(2) Absorption.
(3) Metabolism.
(4) Elimination.
[Pg 188]
(b) Factors influencing use of food:
(1) Stimulation of secretory cells through appetite
juice (stomach); hormone secretin
(intestines).
(2) Factors retarding use of food:—Fear,
worry, anger, nervous excitement, fatty
foods and alkaline carbonates (bacterial action
causing fermentation and putrefaction).
(a) Outline the processes through which a slice of bread and butter must pass, from the time it is eaten until it reaches the blood stream.
(b) Outline with a diagram the manner in which the foodstuffs are utilized in the body.
(c) Show in the form of a table the effect of the enzymes on proteins, on fats, on carbohydrates.
[51] “Chemistry of Food and Nutrition,” by Henry Sherman.
[52] “Chemistry of Food and Nutrition,” by Sherman.
[53] “Chemistry of Food and Nutrition,” by Henry Sherman.
[54] Compiled from “Textbook of Physiology,” by Howell, and “Chemistry of Food and Nutrition,” by Sherman.
[55] “Chemistry of Food and Nutrition,” by Henry Sherman.
[56] This scheme applies to the protein, fat and carbohydrates with quantitative variations only. Courtesy of Dr. A. R. Taylor, Leland Stanford University.
[57] “Chemistry of Food and Nutrition,” by Sherman.
[58] Herter’s “Bacterial Infections of the Digestive Tract” (1907).
[59] “Chemistry of Food and Nutrition,” by Sherman.
[60] “Chemistry of Food and Nutrition,” by Sherman.
[61] “Newer Points of View Regarding the Part Played by Different Foodstuffs in Nutrition,” by Lafayette Mendel, Ph.D. Read at the Sixty-fifth Annual Meeting of the American Medical Association, June, 1914.
There are many traditions in regard to the food requirements of the prospective mother. Many of these have been proved fallacies. As a matter of fact it is the woman more than the developing child who is likely to suffer if the diet is insufficient or badly balanced.
Factors Affecting Diet during Pregnancy.—In formulating a dietary for the pregnant woman, then, not only must the needs of the child be considered but those of the mother also, since the developing embryo draws from the body of the woman materials necessary for its growth, and if these needs are not covered by an increase in the diet, her body and that of the child also will show evidences of lack of nourishment.
Phosphorus and Calcium Requirements.—If, for example, the mother’s diet is lacking in those materials which produce growth, or is deficient in those mineral salts, such as those of phosphorus and calcium, which are requisite and necessary for the growth of bones in the infant, the mother’s bones and teeth will show this loss and in all probability the baby will sooner or later also show a like deficiency. However, it must be remembered that the pregnant woman is under a strain, both physical and mental. She must not be encouraged to eat beyond her needs or the digestion will be disturbed.
Nutritional Disturbances in Early Months.—The nutritional disturbance manifested by nausea and vomiting in the morning is due, not to the stomach or any disturbance therein, but to the fact that a mild form of poisoning [Pg 192] occurs, resulting from the substances produced through the formation of the placenta reaching the general circulation on account of the incomplete establishment of the connection between the embryo and the mother. As soon as this connection is complete and fetal circulation is established this “morning sickness” disappears.
Food Requirements of Prospective Mother.—The food requirements of the prospective mother are not materially affected during the first four months of gestation, and even after this, when the infant is developing rapidly, and up to the date of its birth, the mother’s requirements are only increased about 20%. The amount of food necessary to cover the body needs, for maintenance and energy of a woman living a sedentary or moderately active life, plus 20% for building materials for the growing child, will be adequate for the pregnant woman. Thus, if her needs are ordinarily from 2,000 to 2,400 calories per day, after the fourth month they will probably be increased to 2,400 or 2,800 calories a day and will rarely ever be more than 3,000 calories a day.
Dietetic Treatment of Normal Pregnancy.—The peculiar conditions surrounding the woman at this particular time must be taken into consideration in arranging her diet. The building foods which are necessary for the developing child must be given in the simplest form, milk and eggs being used liberally and meat sparingly to obviate any unnecessary tax being placed upon the kidneys. The use of fruit and green vegetables to supplement the milk and eggs is urged. It has been found advisable at such times to give small meals frequently rather than the regular meal three times a day. The feeling of “fullness” which often occurs during the last two or three months of gestation makes it more comfortable for the pregnant woman to eat less at a time and oftener. If, for example, she be given a glass of rich milk or a nutrient beverage, either of [Pg 193] enforced malted milk, albumenized orange juice, buttermilk, zoolak, or koumiss, at about eleven o’clock in the morning and again about four o’clock in the afternoon, she will have taken sufficient nourishment to meet the new requirements without taxing her digestion or imposing extra work upon the kidneys.
Abnormal Symptoms.—The chief point to keep in mind is any abnormal symptom which may develop. The chief of these is albumen in the urine. The urine must be examined frequently and measures taken immediately to overcome albuminuria should it occur. It is wise, as has already been stated, to restrict the meat in the diet, and in cases where albumen is found in the urine even when the meats are restricted, it may be necessary to place the patient upon a milk diet for a time until the urine clears up.
Supplementary Feeding.—Cereals, especially the whole cereals, must be used liberally. Gruels made with milk are often found valuable additions to the dietary. The prospective mother must be urged to take a regular amount of gentle exercise, not to become over-tired, or excited, to eat sparingly at night, and to drink plenty of water. She must avoid becoming constipated by eating plenty of green vegetables and fruit.
Sample Diet Sheets.—The following dietary is suggested: Breakfast should consist of thoroughly cooked cereals, wheatena, cream of wheat, malt breakfast food, cracked wheat, rolled or cracked oats, served with cream or sugar or both, whole wheat bread, muffins, or biscuits, with butter, raw or stewed fruit, coffee, tea or cocoa with milk. Luncheon may consist of milk or vegetable soups, eggs in any form, boiled potatoes, sweet potatoes, string beans, greens, or any green vegetables, simple desserts such as custards, rice or tapioca puddings, bread pudding, etc., milk, tea, cocoa, buttermilk, zoolak or koumiss as beverages. For dinner, if albuminuria is not present, a small piece of [Pg 194] meat may be taken, together with green vegetables, rice, potatoes, simple salads, and a simple dessert, milk or coffee with milk as a beverage.
Selection of Food.—The following foods may be used to formulate the diet sheet: Wheat, oat, or corn cereals, rice, tapioca, made into simple puddings or served as breakfast foods; fruits, oranges, prunes, apples, raisins, dates, figs, or grapefruit, stewed or raw. The fruit juices may be used instead of the whole fruit if the latter disagrees. Vegetables: peas (green or dried), beans (string beans or dried beans), spinach, greens (turnip, mustard, or beet), cabbage, onions, celery, lettuce, served as vegetables or in soups, potatoes. Meat: lightly broiled beefsteak or stewed or boiled meat or chicken served not more than once a day or three times a week. Eggs, prepared in different ways. Cheese dishes. Breakfast bacon or ham in moderate quantities, butter, olive oil (or other salad oils) in moderation, whole wheat, graham or bran bread, Boston brown bread and crackers, milk, cocoa, chocolate, buttermilk, malted milk, koumiss, or zoolak; coffee and tea in moderation.
The diet, as has already been stated, may be supplemented by nutrient beverages or milk gruels.
The diet of the nursing mother, as has been explained in a previous chapter, must not only cover her own requirements but must likewise be adequate to furnish the extra requirements imposed by the nursing infant.
Food Requirements of Nursing Infant.—When the baby is a month old he should be growing rapidly, and his food requirements at this period and until he is about three months old will be approximately fifty calories per pound of body weight in the twenty-four hours. As he grows older his requirements grow gradually less in proportion to his weight. This is because the rate of growth is less, so that [Pg 195] for the next three months the requirements are from 43 to 40 calories per pound of body weight per day, and 35 calories per pound during the last three months, or by the end of the first year of life.
It has been estimated, as before stated, that the average infant will take 2⅓ to 2½ ounces of mother’s milk per day[63] to each pound of body weight and that every ounce of mother’s milk will yield on an average 20 calories. Hence a month-old baby weighing ten pounds will be taking about 23 ounces a day, yielding 460 calories. Scientists have estimated that for every calorie produced by the milk two extra calories must be provided by food, so that for the baby requiring 460 calories per day, to cover his requirements the mother will be obliged to consume extra food to yield 920 calories, or the regular amount to meet her normal requirements plus the extra food to make sufficient food for the baby.
Diet of Nursing Mother.—The diet of the nursing mother need not be different from that to which she is accustomed. She should be warned against overwork or over-fatigue, nervous excitement and worry, since these factors affect the digestion of the nursing baby. She must be careful not to eat indigestible foods or foods which disagree with her, as such things will undoubtedly affect the digestion of the infant. When an article of food does cause digestional disturbances in the baby, it should be carefully omitted from the mother’s diet.
Factors Retarding and Stimulating Milk Secretion.—Constipation in the mother reacts quickly and unfavorably upon the secretion of milk. The same has proved to be the case when she becomes excited, nervous, worried, or over-tired.
The average diet for the normal woman is safe for the nursing mother. If her supply of milk is deficient, it may [Pg 196] be at times increased or stimulated by the drinking of a glass of milk between meals or by taking a cup of hot cereal milk gruel. It was formerly believed that beer, ale, or stout acted directly upon the mammary glands, stimulating the secretion of milk, but there is little proof of this and the drinking of alcoholic beverages need not be encouraged on this account, since often more nourishing beverages fulfill the purpose more efficiently and without bad results.
Gastric Disturbances.—The nausea and vomiting so often a part of early pregnancy is not believed to be the result of a disordered stomach but primarily a mild form of poisoning resulting from the incomplete establishment of the fetal circulation.
Adjusting the Diet.—The adjustment of the diet to cover the needs of the prospective mother and those of the developing child is essential. The amount of food taken by the mother is not materially changed during the first three months of gestation. An average normal diet is all that is necessary. After this time a twenty per cent. increase in the woman’s diet will furnish adequate means both for her maintenance and for the growth and development of the child.
Type of Food.—The kind of food which is necessary for the pregnant woman to take during this period is very similar to that taken ordinarily. It is necessary to furnish food materials rich in calcium and phosphorus, with an adequate supply of proteins in their simplest form in order to meet the requirement of the growing organism. Milk and eggs furnish the most efficient foods in this respect and the prospective mother should see that they form the chief items of her daily dietary. Milk furnishes calcium in its most available form for the developing skeleton of the growing infant, hence it is necessary to provide the mother with [Pg 197] food to replace the mineral which is withdrawn from her body.
Meat in the Diet.—Meat should be eaten sparingly by the prospective mother, as it imposes needless work upon the already taxed kidneys and, if eaten in excess, will give rise to dangerous complications. Milk and eggs will provide ample protein for all purposes.
Albumen in the Urine.—Albuminuria is one of the most frequent complications in pregnant women. It should be combated and controlled as soon as possible. The allowance of meat should be cut down or entirely eliminated from the diet until the urine clears up. When albuminuria is persistent in spite of efforts to overcome it, the patient must be placed upon a strict milk diet as used in acute nephritis, to prevent dangerous complications arising.
Diet of Mother.—Her dietary need not differ materially from that to which she is accustomed. She must avoid indigestible foods or any article which has been proved to disagree with either the infant or herself.
Factors Regarding Secretion of Milk.—Constipation, worry, nervous excitement, and over-fatigue all have an unfavorable effect upon the secretion of milk and must therefore be avoided by the nursing mother.
The Bowels.—Constipation of the mother reacts quickly and unfavorably upon the health and comfort of the baby, hence it should be avoided by eating coarse breads, green vegetables, and fruits, when they do not disagree with the baby, by drinking plenty of water and taking a certain amount of outdoor exercise to keep her own health in good condition.
Stimulating the Milk Production.—When the milk supply is deficient it will be advisable for the mother to drink a glass of milk or a bowl of cereal milk gruel between [Pg 198] meals. Alcoholic beverages are not necessary to insure an adequate secretion of milk. The milk or milk gruels answer the purpose more efficiently and without bad results.
Energy Requirements of Infant.—The average baby requires fifty calories per day per pound of body weight to cover his energy growth and development needs for the first three months of life, after which the rate of growth is less and his requirements decrease from forty-three to forty, then to thirty-five calories per day per pound by the end of his first year.
Amount of Milk Needed for Infant.—Approximately two and one-third ounces to each pound of body weight per day covers the needs of the average baby.
Fuel Value of Mother’s Milk.—Each ounce of milk yields twenty calories.
The Making of Milk.—It has been estimated that for every calorie yielded by milk, two extra calories must be provided by food.
(a) Formulate a dietary for a pregnant woman, allowing for a twenty per cent. increase over her normal requirements.
(b) Show how the diet may be made to cover the need for additional iron, calcium and phosphorus.
(c) Formulate a diet for a nursing mother with an infant two months old and weighing twelve pounds.
[63] “Feeding the Family,” p. 93, by Mary Swartz Rose.
In taking up this part of our study on nutrition, there are several points to be kept in mind by the nurse: (1) that it will be difficult, if not impossible, to understand the metabolic changes taking place in abnormal conditions unless those occurring in the normal human body are understood; (2) that certain diseases are due directly to errors in diet; (3) that in other diseases, diet plays the chief part both in the bringing about and in the relieving of the conditions; (4) whereas there are certain other diseases not affected by diet, save in so far as well or poorly selected and prepared food always affects the individual, whether normal or abnormal, and that in the latter conditions the organism is more susceptible to bad influences.
This being the case it behooves the nurse to examine herself to find whether or not she understands the fundamental principles underlying the nutrition of the human body, that she may efficiently deal with the changes which occur more or less when the body is attacked by disease.
We include normal infant feeding in this section, because in no other age is it quite so necessary for care to be observed in formulating and carrying out a diet. Errors during this period may only appear to exert a local influence, causing disturbance which may readily be relieved, but the danger is in laying too little stress upon these disturbances, forgetting that the delicate organism of a child may be permanently injured by a constant disregard of nature’s mandates. In the words of the old adage, the pitcher may go once too often to the well, and an injured digestive apparatus is even more difficult to mend than the proverbial pitcher.
[Pg 200] In this section, then, the metabolic changes due to pathological conditions and the dietetic treatment thereof will be discussed.
Age and Weight.—As has already been stated, there are certain points to be kept in mind in attempting to provide an adequate diet for the human machine; First, the age and weight. The gain during infancy should be steady—an allowance of 40 calories per pound of body weight to cover the energy requirements and 4 protein calories per pound to cover the nitrogen needs. During the second and third years the energy requirements will be covered by 30 to 40 calories per pound and the nitrogen needs by 3 to 4 protein calories per pound. From the fifth to the eighth year the nitrogen needs continue to be covered by 3 to 4 protein calories per pound and the energy requirements by 35 to 37 calories per pound during the fifth year; 32 to 34 calories per pound during the seventh year. After the body has reached its full development its requirements will be met if sufficient protein is provided to cover its maintenance needs and if the energy calories are regulated according to the amount of exercise taken, keeping in mind that the energy requirements of a man at rest (sitting) will be about 2,000 calories per day and that exercise, especially that taken in the open air, raises the energy needs of the body.
Daily Gain.—In estimating the relative daily gain in body weight of children of different ages, Mendel[64] gives the following table:
| In the first month, about | 1.00 per cent |
| At the middle of the first year | 0.30 per cent |
| At the end of the first year | 0.15 per cent |
| At fifth year | 0.03 per cent |
| Maximum in later years for boys | 0.07 per cent |
| Maximum in later years for girls | 0.04 per cent |
[Pg 201] Retention of Nitrogen in Infancy.—When the baby is gaining in weight and strength there is a retention of both nitrogen and salts, and when the baby is not gaining there may be a loss of both of these bodies; when one is retained in the body the other is apt to be retained.[65]
Much has been written in the past few years on the care and feeding of infants and children. This is well, since statistics show an alarming increase in the rate of infant mortality during the early years of life, and anything which can be done to check this lamentable and often avoidable waste of valuable life should be resorted to with care and attention.
Food for Infants.—The natural food of all young mammals is the milk of their own mother. The rate of growth and development differs in every species; the calf, for example, doubles birth weight much more quickly than does the baby of the same age. However, the milk of the cow, which meets the needs of the calf perfectly, falls short of meeting the requirements of the infant, whose rate of growth is not nearly so rapid. For this reason if for no other, it would be advisable to give the baby its natural food rather than to attempt a substitute which is, at best, a poor one.
Weight.—The average infant weighs from six to seven pounds at birth. This weight should be doubled in the first five or six months of life and tripled by the end of the first year. The most important business, then, in the life of the child during the early years is growth and development. To achieve this properly the baby’s habits must be adjusted to his needs.
Regularity in Feeding.—He must have the proper food and enough of it, and have it given at regular intervals, [Pg 202] “by the clock,” for guesswork is fatal in infant feeding. He must be given water between meals. Babies often cry from thirst when they are thought to be doing so from hunger or temper, or both. The healthy baby sleeps about twenty-two hours out of twenty-four during the early months, and even during the latter six months of the first year more time is spent in sleeping than in waking.
The Bowels.—The bowels should move several times a day, the stools being smooth and of a yellowish color, of the consistency of pea soup. After the first month, twice a day is about the normal number of stools for the healthy baby. The infant should be placed upon a vessel held in the lap of the nurse at regular times, preferably right before the morning bath, and in the evening. In this way regularity in evacuating the bowels is obtained, and a habit formed which will prove valuable through life.
The Bath.—The daily bath is likewise necessary for the health and comfort of all babies; so, too, are fresh air and sunshine.
As has already been stated, breast milk is much better for babies than cow’s milk or any artificial food. There is something in the mother’s milk which gives strength and resistance to the baby which is absolutely lacking in any other food no matter how carefully it is selected and prepared, and for this reason young mothers must be prevailed upon to nurse their babies whenever it is possible for them to do so. When circumstances, such as having to be away all day at work, make it impossible for a mother to nurse her baby at regular intervals, she can be taught how necessary are two or three breast feedings a day to the future welfare of her child. When social reasons or lack of desire on the part of the mother make her unwilling to nurse her baby, it is the part of the nurse to lay the case before her and let her judge whether or not she is willing to accept the responsibility of bringing into the world a [Pg 203] life for which she is unwilling to provide weapons with which to fight the good fight.
Habits of Mother.—The mother must be taught how to efficiently nurse her baby; she must keep in mind that upon her good health and temperate habits depend the health and comfort of her baby. It devolves upon her to provide food efficient in quality and quantity. To do this, her own diet must be simple and wholesome. The nursing mother must remember that she has to provide, not only for her own maintenance and energy requirements, but also for the infant whose fuel requirements are ever demanding more food to provide for its rapid growth.
Food and Its Relation to Milk.—It is believed that two calories of food extra are necessary to produce one calorie of milk, and since a month-old baby requires 2⅓ ounces of mother’s milk to every pound of his body weight, and one ounce of mother’s milk will yield 20 calories, it is clearly seen that the mother will have to increase her diet to cover the requirements of the baby. For example, if the baby weighed 12 pounds, he would require 28 ounces of milk in 24 hours, or 560 calories. Thus if it requires two calories of extra food to make one calorie of milk, the mother’s diet would have to provide 1,120 calories extra, or about as much food as would fulfill the needs of a laboring man, 3,000 to 3,500 calories, even if she were doing practically no actual work; while if she were actively employed and doing a certain amount of physical labor, her rations would have to approximate those of a man doing heavy muscular work (about 3,500 to 4,000 calories per day).[66]
Breast Milk versus Cow’s Milk.—Consensus of opinion shows that breast-fed infants require less energy than the ones who must be nourished artificially. This is probably due largely to the fact that the constituents of human milk are in a more available form than those in cow’s milk, the [Pg 204] former requiring a lesser expenditure of energy on the part of the organism to become available than the latter. Very active babies, ones who kick and throw themselves about or cry violently, have a greater energy requirement than the more placid baby who sleeps more and is more quiet in movement and who cries less when awake. Breast-fed babies are generally more quiet than their less fortunate artificially fed brothers. It has been demonstrated that the artificially fed baby has a much harder fight for existence than the baby who receives his natural food; hence the necessity of using every available means to make the food digestible, and to lessen the danger arising from the additional work put upon the entire apparatus. Cow’s milk contains practically the same chemical elements as are found in human milk, but these elements are combined in a slightly different manner, and are not so easily handled by the immature organs. The proteins of milk consist of casein, which is insoluble, and albumen, which is soluble. According to Van Slyke the proportion of insoluble to soluble protein in cow’s milk is 3.6:1, while in human milk the proportion is only 1:1. The ash constituents in cow’s milk are in excess of the needs of the infant organism, but since a great part of these salts is in an inorganic form they are not retained to the same extent as those contained in human milk, which are in an organic form.
Rules and Regulations.—It is not possible to lay down hard and fast laws to cover the subject of infant feeding. The food must be adapted to the individual needs of the baby in question. The nurse must see that the milk is obtained from a responsible dealer, certified milk being of course the safest. The bottles of milk should be wiped off carefully and placed directly on the ice as soon as they are received. The milk generally used in infant feeding has a fat content of 4%. That having a higher percentage of fat is technically cream. The following table showing the [Pg 205] fat, sugar, and protein composition of whole milk, cream, skimmed milk, and whey was arranged by Morse and Talbot:[67]
| Fat | Milk Sugar | Protein | |
| Whole milk | 4.00 | 4.50 | 3.50 |
| 7% cream | 7.00 | 4.45 | 3.40 |
| 10% cream | 10.00 | 4.40 | 2.25 |
| 16% cream | 16.00 | 4.20 | 3.05 |
| 32% cream | 32.00 | 3.40 | 2.50 |
| Skimmed milk | 1.00 | 5.00 | 3.55 |
| Separated milk (fat-free) | 0.25 | 5.00 | 3.65 |
| Whey | 0.25 | 5.00 | 0.90 |
Seven per cent. (7%) cream is obtained from the upper 16 ounces of a quart bottle of milk which has been allowed to stand undisturbed for six hours. The upper third of the bottle contains 10% fat, while the whole fat layer from the quart bottle, regardless of the number of ounces, contains about 16% of fat.
Methods of Artificial Feeding.—The use of whole milk, top milk, or skimmed milk, diluted with water, and either milk sugar, malt sugar, or sucrose (cane sugar) added, is the method of feeding most commonly used, and upon it are based the formulas universally advised by infant specialists. There are cases in which simple dilution is not advisable. In premature or very young infants, for example, the whey mixtures have been found to give the best results. In toxic diarrheas, where the putrefactive bacteria make the use of all but the minimum amount of protein inadvisable, the above method is contraindicated, as it is likewise in cases where vomiting of casein curd is a prominent feature.[68]
The Use of Alkalies.—There are many cases in which [Pg 206] the physician deems it advisable to add an alkali to the milk mixture. The one generally selected is limewater. However, sodium citrate and sodium bicarbonate are also used. The reasons for adding alkalies to the milk mixtures are: (1) to check the coagulation of the casein, (2) to hasten the emptying of the stomach, or (3) to chemically change the formation of the curd. In certain cases it is only necessary to delay the coagulation of the casein in the stomach, in which case a certain amount of limewater is used. Its action is to swell the protein of the milk and in this way effect the precipitation of the casein. In other cases it is found advisable to prevent the formation of curd and hasten its departure from the stomach. Cannon[69] claims that milk before it coagulates leaves the stomach quickly like water in gushes. Hence, if an alkali like limewater, bicarbonate or citrate of soda is added to the milk this coagulation will be checked and the digestion be facilitated.
Amount and Type of Alkali Used.—The amount of alkali[70] necessary to bring about any change in the general effect of the formula must be determined by the amount of milk and cream in the mixture, since these constituents alone determine the acid content. However, it is impossible to judge exactly the amount of alkali to add, but an approximate estimate is made from the work done by the various investigators. It has been estimated that from 25 to 50% of limewater must be added to milk to change it to any marked degree. In using bicarbonate of soda, a much less quantity brings about the desired result, 1½ grains of bicarbonate of soda being equal to one ounce of limewater. The action of these two alkalies is different. The soda acting upon the milk causes the curds to be more porous, and therefore more easily acted upon in digestion.
[Pg 207] Sodium citrate likewise tends to prevent the formation of tough curds. It is added in amounts of 1 to 2 grains to each ounce of milk or cream in the mixture whenever it is found necessary to use it at all.
The addition of any alkali to the formula is resorted to if the symptoms indicate the need for it, but the type and quantity is entirely within the province of the physician, not the nurse.
The Addition of Sugar.—Lactose is the form in which the carbohydrates are found in milk, and it has been a general rule to employ this sugar in making up the sugar content of a formula, using from 6 to 7% of the mixture in this form to cover the necessary energy requirements of the infant. Other sugars are used, however; and of late years malt sugar has been widely employed for this purpose. The form now generally accepted is known as dextri-maltose, which is a combination of dextrin and maltose, both of which are readily acted upon by the sugar-splitting enzymes of the digestive juices. In digestion, lactose or milk sugar is split to dextrose and galactose and utilized in the body, both as a source of energy and as a food for the lactic acid bacteria which are active in the small intestine.
Malted Foods.—The addition of malted foods or malt sugar to the food of infants tends to bring about a more rapid gain, both in energy and in body weight, than is generally the case where other sugars are used. This sugar is used as a substitute for milk sugar in many formulas, especially in those cases in which the casein of cow’s milk needs to be made more digestible in form. Malt sugar is indicated in the following conditions:[71] (1) in severe atrophies, (2) in cases of fat indigestion before the atrophic stage is reached, (3) in cases where there is slight curd indigestion, indicated [Pg 208] by some vomiting and slow gain in weight, (4) in cases where excessive intestinal fermentation is manifested by gas and colic.
Malt sugar (dextri-maltose) is contraindicated to a slight degree in cases “of simple acute diarrhea where lactose, by supplying fermentative media, more easily restores the normal bacterial balance.”
Diluents.—Barley and oatmeal water are used as diluents to the amount of one-fourth or more of the mixture. Oatmeal water or jelly is used more during the winter months than in the hot summer months. As the fat content of the oatmeal gives it a more laxative effect, it is undesirable to use it at the season in which the summer diarrheas are prevalent. Barley water has something of a colloidal action upon the casein, causing the curds to be finer and less tough in character. Both barley and oatmeal water are used in place of plain water for babies when this colloidal effect upon the curd of the milk is desired, also where the weight of the infant shows a disposition to remain stationary, especially where there are no other symptoms to account for the lack of gain.
Whey is used with babies who cannot digest the insoluble protein of cow’s milk. This is often the case in premature babies and is manifested by a persistent vomiting of curd. The energy requirements are obtained by the addition of cream and lactose to the whey.
Buttermilk Mixtures and “Eiweissmilch.”—It is often found desirable to use some other form of milk than whole, top, or even skimmed milk, and for this purpose lactic acid, milk and the albumen or “Eiweissmilch” are substituted. In the buttermilk mixtures the precipitation of the casein is brought about by lactic acid bacilli (Bulgarian culture). This prevents the coagulation of the casein into tough curds. Lactose buttermilk or lactic acid milk is used in the feeding of infants who have persistent green stools, and in cases of [Pg 209] acute toxic diarrhea brought about through the action of gas bacillus.
Buttermilk is more difficult to administer to babies than formulas made from plain milk by reason of its flavor. However, the results are remarkable in the above-mentioned conditions.
“Eiweissmilch” is used in atrophic cases where there are bad green stools.
“Homogenized Milk.”—Dr. Ladd of the Children’s Hospital in Boston has presented many cases of infants who showed an intolerance for butter fat. These cases he has treated with formulas containing foreign fat, usually olive oil. This milk is subjected to a treatment which brings about a more complete emulsification of the fat than is possible in cow’s milk, causing it to resemble in character the quality of the mother’s milk. Homogenized milk has been used with success in cases where it was impossible to supply the infant with breast milk.
The process is accomplished by the use of an apparatus known as an “homogenizer”[72]; in this machine the fat globule is crushed and so finely divided as to prevent its re-formation. The greatest drawback to the use of this process lies in the scarcity of available machines. Cod liver oil is now used in many cases where the infant shows a failure to gain or is in possible danger of developing rickets, with the homogenizer it is possible to add the oil to the formula, thus facilitating its use.
Technique of Milk Modification.—The absolute necessity for cleanliness has already been dwelt upon in respect to milk, and in infant feeding the vigilance which must be observed in the preparation of the food cannot be too strongly emphasized. The milk itself must be of known purity. Where there is any uncertainty about its source, it [Pg 210] must be sterilized or pasteurized according to the doctor’s orders. The bottles and nipples should be washed as soon as they are used, first with plain water to remove the milk, then with soapsuds and a bottle brush. The bottles should then be filled with boric acid or bicarbonate of soda solution until needed, when they should be emptied and placed in a deep pan filled with cold water and allowed to boil for a few minutes. They should not be taken from the water until they are to be filled with the milk mixture. The nipples are washed thoroughly and boiled once a day and dropped into a solution of boric acid or bicarbonate of soda when not in use. The plain black rubber nipples are best as they can easily be turned inside out and cleaned. If the milk drops too slowly from the bottle, the nipple may be pierced in one or two places with a darning needle.
The morning is the best time in which to prepare the baby’s food; the milk has not stood too long and it is easier to regulate the feedings if a fresh start is made each morning. Let the bottles and the rubber corks with which they must be stopped be boiled and cooled while the milk mixture is being prepared.
Preparation of Diluents.—If barley or oatmeal water is to be used as a diluent, let that be prepared first, that it may be cool before adding it to the milk. Cover the table with a clean cloth or oilcloth, upon this place the pitcher in which the milk is to be modified, have the funnel, milk dipper, and spoon which are to be used boiled with the bottles, cover the mouth of the pitcher with a clean square of gauze or cheesecloth, read the formula carefully and measure the sugar, dextri-maltose, lactose, Mellin’s Food, or cane sugar as directed and place it in a clean glass; now measure the diluent, water, oatmeal water, barley water, or whey; use part of this diluent to dissolve the sugar.
Measuring Milk according to Percentage of Fat.—Now dip off the required layer of top milk, that is, the layer [Pg 211] containing the desired percentage of fat and protein. Mix this thoroughly and dip out the requisite number of ounces into the pitcher. If there is not sufficient cream in one quart bottle to fill the formula, the cream must be dipped from a second bottle and mixed with that of the first before it is measured into the pitcher. The dissolved sugar and rest of the diluent, together with the correct amount of limewater, are strained into the pitcher, mixed thoroughly, and strained through the absorbent cotton lining the funnel into the bottles, allowing the correct number of ounces for each feeding in every bottle.
Pasteurizing the Milk.—The corks are then adjusted, the bottles placed in the pasteurizer[73] and pasteurized for the desired number of minutes. The water in the pasteurizer must be cold in the beginning and the rise of temperature recorded on the thermometer, which is adjusted at a convenient place in the pasteurizer where the scale can be read easily. If the temperature of the water is too high, add cold water and lower the flame beneath the pasteurizer. When the desired number of minutes has elapsed, lift the bottle rack above the water for a few minutes and allow a stream of cold water to flow into the pasteurizer, taking care not to chill the bottles too suddenly or they will crack. Cool the bottles as quickly as possible and place on ice until needed, warming the bottle of milk as needed in warm water.
Amount Given at Each Feeding.—At birth a baby will usually take from one half to one ounce at each feeding, this amount is increased at the rate of a quarter of an ounce each week until the baby is receiving eight ounces at each feeding. Or the food is measured to allow of from one ounce to an ounce and a half more than the child’s age in months. For example a baby six months old would receive from [Pg 212] seven to seven and a half ounces at each feeding. Some babies are bigger and stronger than others and require the maximum amount, while others are less vigorous and the amount of food which they can handle at a feeding may fall slightly short of the above amounts, but the quantities indicated above will serve as a guide in measuring the formula.
Method of Calculation of Formula.—The calculation of a formula consists in determining the amount (in grams or ounces), of the various constituents contained in the formula when the percentage of each is known. Or, in determining its percentage composition when the amount of fat, protein, carbohydrate and diluent is given. There are certain inaccuracies in all simple methods of calculation and the use of the Babcock tester to determine the fat content in the milk to be used, is advised in all milk or formula rooms. The following method of calculation has been found satisfactory, and the nurse must master it in order to intelligently carry out the directions of the pediatrist.
Determining the Composition of Formula.[74]—Gravity cream and skimmed milk are used in this method, the cream is estimated as containing 16% fat, and consists of the entire cream layer from a quart bottle of milk which has been allowed to stand without being disturbed for six hours or longer. The cream must be dipped off with a cream dipper, or poured off. If there is not a sufficient number of ounces in one bottle of milk, a second must be used, the entire cream layer taken, then mixed with that obtained from first bottle, before the required number of ounces are measured off. Skimmed milk is estimated as being fat-free (although this is not entirely accurate). Both gravity cream and skimmed milk are estimated as containing 3.2% protein, and 4.5% sugar. In this method, [Pg 213] one rounded tablespoonful of milk sugar is estimated as weighing one half ounce (dextri-maltose may be estimated in the same way). With this brief explanation of the terms used we will proceed with the method itself.
It is always essential before beginning the calculation of the formula, to know what percentages of fat, sugar, and protein it is to contain, and the amount to be given in twenty-four hours; it is also necessary to know how much lime water is to be added if this substance is to form a part of the formula.
Suppose a thirty-two-ounce mixture is to be made containing 3% of fat, 6% of sugar, 2% of protein, and lime water sufficient to equal 25% of the cream and skimmed milk in the mixture. The fat in the food must be derived from cream, since it is the only substance containing fat to be used in the formula. If the food was composed entirely of gravity cream it would contain 16% of fat. Since it is to contain but 3% of fat it is evident that only 3/16 of the mixture must be gravity cream, 3/16 of thirty-two ounces is six ounces. Six ounces of gravity cream will, therefore, provide the 3% of fat desired in the mixture. The gravity cream contains protein as well as fat. There are six ounces of gravity cream in the thirty-two-ounce mixture. The protein content of gravity cream is 3.2%. The protein content of a thirty-two-ounce mixture containing six ounces of gravity cream is evidently 6/32 of 3.2% or 0.60%. Two per cent protein is, however, desired in the mixture. The gravity cream has provided only 0.60%. One and forty hundredths per cent of protein, the difference between the percentage of protein desired and that furnished by the gravity cream, must be obtained in some other way. It must be obtained, moreover, from some substance which does not contain fat. Skimmed milk is such a substance. Skimmed milk contains 3.2% protein. In order to get 1.40 per cent in the mixture by the [Pg 214] use of skimmed milk, it is evident that 140/320 of the mixture must be skimmed milk. 140/320 of thirty-two ounces is fourteen ounces. Fourteen ounces of skimmed milk will, therefore, provide the additional 1.40% of protein desired.
Both gravity cream and skimmed milk contain 4.50% milk sugar. Twenty ounces of gravity and skimmed milk are required to furnish the desired percentages of fat and protein. These twenty ounces in a thirty-two-ounce mixture must add 20/32 or 4.50% of sugar to the mixture. Twenty thirty-seconds of 4½ or 20/32 of 9/2 = 180/64, or practically 3% of milk sugar. It is, however, desired to have 6% of milk sugar in the mixture. That is, 3% more of milk sugar is required. This additional sugar must be added in the form of dry milk sugar. Three per cent of thirty-two ounces is 3/100 of thirty-two. This will give the amount of sugar desired in ounces. The sugar is to be measured in rounded tablespoonfuls, or half ounces. If the figures given above are multiplied by two, the result will be the number of rounded tablespoonfuls needed. That is, 3/100 of 32 × 2 = 192/100 rounded tablespoonfuls, or for all practical purposes, two rounded tablespoonfuls.
It is also desired to have the amount of lime water in the mixture equal to 25% of the cream and milk in the mixture. There are twenty ounces of cream and milk in the mixture. Twenty-five per cent of twenty ounces is five ounces. Five ounces of lime water must therefore be added. The total quantity of the mixture is to be thirty-two ounces. The milk sugar goes into solution and, therefore, does not add to this quantity. The difference between thirty-two and twenty-five ounces is seven ounces. Seven ounces of water must, therefore, be added to make up the quantity desired.
Changing the Formula.—It is often found necessary to change the formula when using artificial feeding for [Pg 215] infants, and under these circumstances it is necessary to know the percentages of the food constituents contained in the formula already in use. For this purpose the following method, quoted from “Diseases of Nutrition and Infant Feeding,”[75] is included:
Morse and Talbot’s Method.—Suppose that a baby is taking a food made up of—
| Gravity cream | 12 ounces |
| Skimmed milk | 18 ounces |
| Limewater | 6 ounces |
| Barley water | 12 ounces |
| Milk sugar | 4 rounded tablespoonfuls |
“The barley water is made with two teaspoonfuls of barley flour in a pint of water. The total quantity of the mixture is 48 ounces. Gravity cream contains 16% fat. Twelve ounces of gravity cream in a 48-ounce mixture will give, therefore, 12/48 of 16% of fat, or 4% fat. Both gravity cream and skimmed milk contain 3.20% protein. There are 30 ounces of gravity cream and skimmed milk in the mixture; 30 ounces in a 48-ounce mixture will give 30/48 of 3.20% of protein, or 2.00% of protein. Both gravity cream and skimmed milk also contain 4.50% of sugar. Thirty ounces of gravity cream and skimmed milk in a 48-ounce mixture will therefore furnish 30/48 of 4½ which is the same as 30/48 of 9/2 or almost 3.00% of milk sugar. Four rounded tablespoonfuls of milk sugar are equal to two ounces. Two ounces of sugar in a 48-ounce mixture is equal to 2/48 of 100% or 4%. The total percentage of sugar is, therefore, 7%. Two teaspoonfuls of barley flour in a pint of water makes a 1.50% decoction of starch. Twelve ounces of barley water of this strength in a 48-ounce mixture will give 12/48 of 1.50% or about 0.35% starch. There are six ounces of limewater in the mixture and 30 ounces of gravity cream and skimmed milk. 6/30 of 100% is 20%. The [Pg 216] limewater is, therefore, 20% of the milk and cream. The mixture thus contains 4% fat, 7% sugar, 2% protein, and 0.35% starch, while the limewater is in the proportion of 20% of the cream and milk.”
If, therefore, the nurse will follow out the plan suggested by Drs. Morse and Talbot, it should be a simple matter to change the percentage of any of the food constituents in any formula.
The following schemes for feeding well babies are included to facilitate the work in the home. A nurse may teach the mother the manner in which these schemes are used, keeping in mind that there can be no iron clad rule for feeding all babies. No nurse should recommend a formula without directions from a physician. And no formula should be changed without his permission.
The following milk formulas are used in the Nathan Straus Pasteurized Milk Laboratories of New York:
Formula No. 1.—Infants from 1st to 4th week, by A. R. Green.
24 ounces of mixture divided into 8 feedings of three ounces each, fed at intervals of 2½ hours:
¾ oz. 16% cream
3 oz. full milk
19 oz. water
1¼ oz. limewater
1½ oz. milk sugar
Formula No. 2.—Infants 1st to 3d month, by Dr. R. G. Freeman.
1½ oz. 16% cream
3 oz. full milk
13 oz. water
½ oz. limewater
1 oz. milk sugar
Divided into 6 feedings of 3 oz. each, fed 3 hours apart.
[Pg 217] Formula No. 3.—Infants 2d to 6th month, by Dr. R. G. Freeman.
18 oz. full milk
16½ oz. water
1½ oz. limewater
1½ oz. milk sugar
Divided into 6 feedings of 6 ounces each, fed at intervals of 3 hours.
Formula No. 4.—Infants 3d to 7th month, by Dr. A. Jacobi.
18 oz. full milk
18 oz. barley water
1 oz. cane sugar
20 grains salt (less than ¼ tsp.)
Divided into 6 feedings of 6 ounces each, fed at intervals of 3 hours.
Formula No. 5.—Infants 7th to 9th month, by Dr. A. Jacobi.
2½ oz. full milk
7½ oz. oat or barley water
1½ oz. cane sugar
30 grains (about ¼ tsp.) table salt
Divided into 5 feedings of 6 ounces each, fed at intervals of 3½ hours.
(First Year)
Scheme based on Holt and Shaw’s “Save the Babies.” Pub. by Am. Med. Ass’n.
| Time | Milk Ounces | Water Ounces | Sugar | Intervals of Feeding | Number of Feedings |
| 1st and 2d days | 1 to 3 tbs. every 3-4 hours | ||||
| 3d and 4th days | 3 | 7 | 2 tsp. | 3 | 7 |
| [Pg 218]5th and 7th days | 4 | 8 | 3 tsp. | 3 | 7 |
| 8th day | 5 | 10 | 1½ tbs. | 3 | 7 |
| 8th day to end of 3d month | Increase ½ oz. every 4 days | Increase ½ oz. every 8 days | Increase ½ oz. every 2 weeks | 3 | 7-6 |
| End of 3d month | 16 | 16 | 4¼ tbs. | 3 | 6 |
| Beginning of 4th month to end of 6th month | Increase ½ oz. every 6 days | Reduce ½ oz. every 2 weeks. (Cook barley in water if food disagrees)[76] | 4 | 4 | 6-5 |
| End of 6th month | 24 | 12 | 4 | 4 | 5 |
| Beginning of 7th month to end of 9th month | Increase ½ oz. every week if food is well digested and child seems hungry | Reduce ½ oz. every 2 weeks | 4 | 4 | 5 |
| [Pg 219]End of 9th month | 30 | 10 oz. (in which 3 tbs. of cereal is cooked) | 2 tbsp. | 4 | 5 |
| Beginning of 10th month to end of 12th month | Increase 1 oz. per month | Cereal gruel as above | Reduce 1 tbs. per month | 4-5 | 5-4 |
At the beginning of 7th or 8th month, or earlier if necessary, it is advisable to add orange juice, giving from 1-2 tablespoonfuls between the two morning feedings.[77]
After the 4th month it is well to eliminate the night feeding between 10 P.M. and 6 A.M.
At end of 11th month add 1-2 pieces of stale bread, toast or zwieback. Part of soft-cooked egg may be given every other day at noon meal by end of 11th month. The orange juice may be increased to 3 tbs. if bowels are not loose.
The strained cereal should be given twice daily by the end of the first year, and the milk should be undiluted at this time unless the digestion of the infant forbids.
Cooled boiled water should be given several times each day between feedings. Babies cry from thirst as well as from hunger.
Scheme based on Dr. Richard M. Smith’s “The Baby’s First Two Years.”
A full-term baby will usually take a formula made as follows:
| Cream | 2 ounces |
| Skimmed milk | 2 ounces |
| Boiled water | 12 ounces |
| Sugar of milk | 6 level tsp. |
After 3d day increase cream and milk at the rate of 1 ounce each week, and sugar 1 tsp. every other day until at one month the baby will be receiving a formula such as—
| Cream | 5 ounces |
| Skimmed milk | 5 ounces |
| Boiled water | 22 ounces |
| Sugar of milk | 3½ level tbs. |
[Pg 220] At two months—
| Cream | 6 ounces |
| Skimmed milk | 6 ounces |
| Boiled water | 20 ounces |
| Sugar of milk | 4 level tbs. |
From this point the formula may be increased by adding 2 ounces of skimmed milk each month until the baby is eight months old. For each ounce of milk added, an equal amount of water should be omitted. The sugar in the formula should be reduced one half tbs. every three months.
At six months the baby would be taking—
| Cream | 6 ounces |
| Skimmed milk | 14 ounces |
| Boiled water | 12 ounces |
| Sugar of milk | 3½ level tbs. |
At eight months—
| Cream | 6 ounces |
| Skimmed milk | 18 ounces |
| Boiled water | 8 ounces |
| Sugar of milk | 3 level tbs. |
This amount will not be found sufficient in quantity for a twenty-four-hour mixture for children of this age. Increasing the amount of the last formula in the same proportion, it will be—
| Cream | 9 ounces |
| Skimmed milk | 27 ounces |
| Boiled water | 12 ounces |
| Sugar of milk | 4½ level tbs. |
At this age the formula usually may be changed so as to be made from whole milk instead of cream and skimmed milk. The formula may be made as follows:
| Whole milk | 36 ounces |
| Boiled water | 12 ounces |
| Sugar of milk | 4½ level tbs. |
From this point on the formula may be increased by replacing the boiled water with whole milk, two ounces each month up to thirteen months. At this age the boiled water may be omitted from the formula one ounce each week. Beginning at the age of eight months the sugar may be eliminated from the formula, one tablespoonful each month.
Barley Water.—At the age of five months, or at any time thereafter, barley water may be substituted for boiled water in the formula. [Pg 221] This should be substituted when the baby is not gaining in weight. It may be substituted in many instances when the movements are not well digested.
Lime Water.—It is frequently found to be advisable to add lime water. It is not necessary in every instance, but should be given if the baby is inclined to spit up, or in cases where the stools are too frequent in number and are slightly green in color.
Determining the Fuel Value of a Formula.—The computation of the fuel value of a formula is very essential since the growth and development of the infant depends largely upon whether or not its energy expenditures are well covered. The method is simple, requiring the same methods used in the computing of other dietaries. Take the formula just calculated, its fuel value would be estimated as follows: Thirty-two ounces are equal to 960 grams. In each 100 grams there would be 3 grams of fat, 2 grams of protein and 6 grains of sugar. Hence in 9.6 one-hundred-calorie portions there would be 9.6 × 3—28.8 grams of fat, 9.6 × 2—19.2 grams of protein, and 9.6 × 6—57.6 grams of sugar, in a thirty-two-ounce mixture.
To determine the fuel value of the formula, these results must be multiplied by their physiological fuel factors, 9 and 4 and 4 respectively. Thus:
| 29 × 9 | = | 261 | calories from fat |
| 19 × 4 | = | 76 | calories from protein |
| 58 × 4 | = | 232 | calories from sugar, or a total of |
| 569 | calories for the entire mixture. |
Scheme for Adding Solids to Infants’ Diet.—
From 9th to 15th month:
| 6 A.M.— | Milk formula (bottle). |
| 8 A.M.— | Orange juice ½ ounce, or prune pulp or prune juice. |
| 10 A.M.— | Bottle, cereal (strained) and bread and butter or zwieback. |
| [Pg 222]2 P.M.— | Mutton, chicken, or veal soup cooked with cereal; small portion of baked potato, small portion of strained spinach or carrots; orange gelatin or cornstarch pudding. |
| 6 P.M.— | Bottle. |
From 15 months to 2½ years:
| 8 A.M.— | Stewed fruit or orange juice; cereal, crisp bacon, alternated with soft-cooked or poached egg; bread and butter or toast, milk or weak cocoa. |
| 12 or 1 P.M.— | Meat or vegetable soup thickened with cereal; lamb chop, scraped beef or chicken or beef juice; baked or mashed potato; strained spinach; carrots; turnips or celery; gelatin, custard, or cornstarch pudding. |
| 3 P.M.— | Crackers and milk. |
| 6 or 7 P.M.— | Bread and milk or cereal; baked apple or apple sauce. |
From 3 to 6 years:
| 8 A.M.— | Stewed fruit or orange; cereal; bacon or egg (soft-cooked or poached); bread and butter; milk or cocoa. |
| 12 or 1 P.M.— | Soup; lamb chop, scraped beef, chicken, or roast meats; potato; all vegetables; celery, lettuce; light desserts: custards, gelatin, lady fingers. |
| 3 P.M.— | Milk; fruit and crackers. |
| 6 P.M.— | Milk or cocoa; stewed fruit; bread and butter; cereals; eggs. |
| ¼ lb. beef, lamb or chicken | 1 tablespoonful pearl barley |
| 1 potato | 2 tablespoonfuls rice |
| 1 carrot | 2 qts. water |
| 2 stalks celery | 1 pinch salt |
Finely divide the vegetables. Add the vegetables, barley and rice to 2 qts. of water. Boil down to 1 qt., cooking 3 hours. Add pinch of salt. Pass through fine sieve.
Morse and Talbot advise baked potato, plain boiled macaroni, rice and wheat germ, bread and butter, baked custard, plain blanc-mange, and plain boiled tapioca to be given when the child is 1½ years old. When the child is nearly two years old they add meat in the most digestible forms, such as the white meat of chicken, lamb or mutton chops, and scraped beef.
The following dietary is suggested for a child two years old:[78]
“Whole milk, butter, mutton broth, chicken broth, beef juice, soft-cooked eggs, dropped eggs, white meat of chicken, lamb or mutton chops, scraped beef, French bread, stale bread, toasted bread, whole wheat bread, milk toast, zwieback, plain white crackers, plain Educator crackers, barley, jelly, oatmeal, cream of wheat, wheat germ, Ralston’s Farina, rice, baked potato, plain boiled macaroni, orange juice, baked apples, stewed prune pulp and juice, junket, baked custard, cornstarch pudding, plain blanc-mange, plain tapioca. It is not advisable, as a rule, to begin green vegetables until the baby is 2½ years old.”
It will be seen in the foregoing dietaries how authorities differ in their beliefs as to the requirements of the child. The dietaries included in this text are selected from those used in different parts of the country by physicians who [Pg 224] have successfully cared for the infants and children under their charge.
The digestion of premature infants is naturally not as strong as that of infants born at term. Very little is positively known, but the consensus of opinion goes to show that in the majority of cases the tolerance for sugar is greater than that of either the proteins or fats. The loss of heat is relatively greater in proportion to its surface area in small than in large bodies. This is a well-known fact, hence the premature baby must require more food in proportion to its weight than the baby who is born at the normal time. Then, too, as the premature infant is thinner he does not keep warm like the older infant, and this must be taken into consideration in feeding him. Breast milk is of course by far the best food for such babies, not only because its constituents are in a more available form for the feeble digestive organs, but because the mother’s milk furnishes a resistance which is lacking in even the most carefully modified of milk formulas.
Energy Requirements of Premature Infants.—Experiments made upon premature infants have proved that the caloric needs of these babies are greater than in the case of full-time babies; that is, they require more per kilogram of body weight. According to Morse,[79] “most premature babies need 120 calories per kilogram of body weight. But there are many exceptions, some thriving on as little as 70 calories per kilogram. No attempt should be made to reach 120 calories per kilogram during the first few days. Thirty calories per kilogram is as much as is wise to give in the first 24 hours of feeding. This amount should be gradually increased each day, watching carefully for symptoms of [Pg 225] indigestion and diminishing it if these appear. One hundred and twenty calories per kilogram can be given in about 10 days.”[80]
Necessary Dilution.—Even breast milk must be diluted with an equal amount of water or a 3% sugar solution. The amount of milk should be increased and the amount of dilution decreased until the undiluted breast milk is given in four or five days. Like older babies, the next best food for premature babies is the properly modified cow’s milk, but the utmost care will have to be observed, as these babies are more easily upset than older and stronger ones.
Premature Infant Feeding.—The following method of feeding may be suggested, keeping in mind that it is an easy matter to increase the strength of a mixture if the baby shows the need of such an increase. The premature baby is rarely strong enough to take the breast.
Method of Administering Milk.—The most satisfactory method of administering the food in such cases is by means of the Brick feeder, which consists of a graduated glass tube, open at either end. On the small end is placed a small nipple like those seen on medicine droppers; this one is perforated and goes into the mouth of the baby. A large rubber finger cot is attached to the other end of the tube. The milk is forced into the mouth by pressing the finger cot. In case the infant is too feeble even for this method of feeding, the desired amount is dropped into the mouth from a medicine dropper; 5 c.c. (about 1 dram or 1 teaspoonful) of diluted milk being given at each feeding. This amount is increased gradually from day to day.
Whey Mixtures.—Whey mixtures have been found to meet the needs of premature infants more efficiently than ordinary mixtures. As the proteins in whey are in a more digestible form, they throw less work on the immature [Pg 226] digestive apparatus. As a rule the casein and whey are in proportion of 1:1.
The following formulas[81] show the amounts in which the food constituents are combined and are suitable for premature babies:
| Fat | 1.00% |
| Milk sugar | 4.00% |
| Total proteins | 0.25% |
| Lime water | 25% of cream and milk mixture |
or
| Fat | 1.00% |
| Milk sugar | 4.50% |
| Total proteins | 0.50% |
| Lime water | 25% of cream and milk mixture |
A word as to the use of Proprietary Infant Foods: These prepared foods may be classified under four heads, as follows: (1) condensed milks; (2) malted foods, those consisting chiefly of carbohydrates in the form of maltose and dextrins; (3) those consisting almost entirely of starch, and (4) those composed partly of soluble and partly of insoluble carbohydrates.
(1) Condensed milk may be sweetened or unsweetened. These milks are never given undiluted, the directions calling for one part condensed milk to nine parts water, which gives a mixture containing 0.90% fat, 5.49% sugar, and 0.80% protein if “Eagle Brand” Condensed Milk is used.[82]
(2) Malted Foods: Mellin’s Food and malted milk are examples of this group. These foods contain the carbohydrates in soluble form and when added to milk make an acceptable addition, as they furnish the carbohydrates in the most digestible form. When fed alone, diluted only [Pg 227] with water, they result in a mixture deficient in both fat and protein.
(3) Imperial Granum is an example of this group, and there are several others with similar compositions. These foods are very much like wheat flour which has been subjected to heat, changing to a small extent the starch to dextrose and dextrin.
(4) Nestlé’s Food, Eskay’s Albumenized Food, and Allenbury’s Food are examples of this group, each containing sugar and a percentage of starch. Upon dilution with water, the amount of fat in the mixture is just a trace.
Incomplete Foods as a Source of Danger.—The ease with which the majority of these foods are prepared and the way in which they agree with the baby constitute the chief danger of their use. If they are added to milk, with the exception of the condensed milk, they result in a modified milk containing the carbohydrates in a more or less digested form. But they are expensive, and give no better result as a rule than a carefully modified milk containing a cereal gruel.
The giving of foods like malted milk alone is dangerous because they are deficient in some of the most necessary constituents, and babies fed in this way, while growing fat, are apt to have soft or brittle bones and muscular tissue higher in fat and water than in protein, so that they do not grow and develop in a normal way, and when they are attacked by the diseases so prevalent in the early years of life, they succumb rapidly, because the resistance given by a properly modified food is lacking.
Condensed milks act in a like manner. That is, in the sweetened milks the carbohydrate content is far in excess of the needs, and the proteins and fats are deficient, so that while the baby fattens he does not receive the building foods commensurate with his body requirements.[83]
[Pg 228] Many mothers adopt the use of these foods because they mean less work than in modifying the milk properly, but the nurse should point out the facts just mentioned, explaining that while these proprietary infant foods are undoubtedly valuable at times to fill a place when the milk formula has not proved satisfactory, the use of these foods as a regular custom is expensive, not only from a financial standpoint but from a standpoint of health, since their disadvantages far outweigh their advantages in the long run.
Breast Milk as a Food.—The superiority of breast milk over any other known food cannot be too strongly emphasized.
Regularity in Feeding.—The absolute need for regularity in feeding—“feeding by the clock” and not by guess or when the baby cries.
Indications of Health.—The normal growth and development to be used as guides as to the physical well-being of the infant; also as an indication of the use of the proper modification of milk for the individual needs of the child.
Dilution.—The amount of dilution necessary—cereal waters, whey, etc.—to increase the digestibility and nutrient values of the formula.
The Addition of Alkali.—The addition of alkalies to milk formulas to accomplish a like purpose.
Milk Sugar, Malt Sugar, Cane Sugar.—The use of the different sugars, namely, dextri-maltose, lactose, or cane sugar under various circumstances as the condition of the infant demands.
Substitutes for Whole Milk.—The substitution of different milk, such as lactic acid milk, Bulgarian culture buttermilk, Eiweissmilch, cream and whey mixtures, as the individual needs of the infant demand.
Technique of Milk Modifications.—The absolute need [Pg 229] for the nurse to understand the technique of milk modification before attempting the care of an artificially fed infant.
Percentage Computation.—A knowledge of percentage, that an accurate computation of a formula may be accomplished.
Preparation of Food.—A sufficient knowledge of food preparation to enable the nurse to prepare any food which may be deemed necessary by the physician for the welfare of the child.
Water.—The importance of giving the baby water aside from that used in modifying the milk. Many babies cry from thirst when they are believed to be crying from hunger or temper.
Increasing the Diet.—The necessity for increasing the amount and strength of the formula with the age, growth, and development of the child by the addition of solid food as soon as the physician deems it advisable.
Feeding Premature Infants.—The method of feeding a premature infant differs from that employed in feeding an infant born at term: (a) because its development has not progressed so far; (b) because its digestive apparatus being more or less immature, food handled with ease by an older baby will be totally unfit for the premature one, both as to quality and quantity.
Wet Nurse.—The advisability of procuring a wet nurse when the mother is unable to nurse the infant, (a) on account of the more digestible character of the food constituents, especially the proteins, in mother’s milk over those of cow’s milk; (b) on account of the resistance furnished by the natural food which has been proved to be very much greater than that furnished by any other food, no matter how carefully the modification of the milk is made.
Premature Infants.—Their caloric needs are greater than in full-term babies, hence their food must be adjusted to meet these needs.
[Pg 230] In fact the nurse must have an understanding of the behavior of foods in the metabolism of infancy and the laws which govern their use in the organism of the child.
(a) Write a formula for a two months’ old infant weighing twelve pounds, which contains 3% fat, 2% protein, and 6% sugar.
(b) Change this formula so that it will contain 3% fat, 1.5% protein, and 6% sugar.
(c) Write a formula for an eight months’ old baby, using whole milk instead of cream and skimmed milk.
(d) Write a formula for a premature baby containing 1% fat, 4% sugar, and 0.25% protein (allowing 30 calories per pound of body weight).
[64] “Childhood and Growth,” p. 18, by Lafayette Mendel.
[65] “Diseases of Nutrition and Infant Feeding,” by Morse and Talbot.
[66] “Feeding the Family,” by Mary Swartz Rose.
[67] “Diseases of Nutrition and Infant Feeding,” p. 218, by Morse and Talbot.
[68] “Generally Accepted Methods for Artificial Feeding of Infants with Indicatives and Contra-Indicatives,” by Orville R. Chadwell, M.D. Reprinted from “New England Medical Gazette,” June, 1916.
[69] “Mechanical Factors of Digestion,” by Cannon.
[70] “Diseases of Nutrition and Infant Feeding,” p. 204, by Morse and Talbot.
[71] “New England Medical Gazette,” June, 1916. Reprint by Orville Chadwell.
[72] The best substitute for the homogenizer is found in an electric mixer; a formula prepared with a fat other than cream can be made by means of this mixer to approximate very closely that of homogenized milk.
[73] There are a number of pasteurizers on the market; one sold by the Walker Gordon Laboratory and one designed by Dr. R. G. Freeman of New York are both satisfactory.
[74] Method suggested by Morse and Talbot, “Diseases of Nutrition and Infant Feeding,” pp. 234-235.
[75] “Diseases of Nutrition and Infant Feeding,” pp. 225 and 226, by Morse and Talbot.
[76] One-half tbs. barley flour may be cooked in the water used as diluent; it should be boiled 20 minutes, strained and cooled before adding to formula.
[77] When babies are fed upon pasteurized, sterilized, or dried milk it is advisable to use orange or prune juice earlier than the seventh month. Dr. Hess suggests the use of canned tomato juice as substitute for orange juice.
[78] “Diseases of Nutrition and Infant Feeding,” p. 236, by Morse and Talbot.
[79] Morse: “American Journal of Obstetrics,” 1905. Hess: “American Journal Diseases of Children,” 1911.
[80] “Diseases of Nutrition and Infant Feeding,” p. 238, by Morse and Talbot.
[81] “Diseases of Nutrition and Infant Feeding,” p. 239, by Morse and Talbot.
[82] “Diseases of Nutrition and Infant Feeding,” by Morse and Talbot.
[83] The proprietary foods on the market are many, but those given above as suggested by Morse and Talbot represent the best known infant foods.
Digestive Disturbances.—It is a well-established fact that artificially fed infants are more subject to disturbances due to diet than breast-fed infants, the digestional disturbances of the latter yielding more readily to treatment. As a rule, with the breast-fed baby it is largely a question of adjusting the diet of the mother, of increasing the fluid in her diet, of seeing that she takes the requisite amount of exercise in the open air, and of lengthening the intervals between feedings or of giving the baby water just before putting him to the breast. With the artificially fed infant it is an entirely different proposition.
Causes in Artificially Fed Infants.—The digestive disturbances may arise from any one of half a dozen or more causes. The constituents in the milk may be in the wrong proportion. The amount given at a feeding may be too great or too little. The dilution may be too great or too small to meet the needs of the infant. Or the milk may contain the microörganisms which bring about fermentation or putrefaction. Any or all of these causes may assail the artificially fed baby. Consequently, all the care that can be exercised must be resorted to in the feeding of these babies, not only after digestional disturbances arise, but as a means of their prevention. In the preceding chapter the methods generally used in the feeding of normal infants were discussed. We now proceed to the feeding under abnormal or pathological conditions.
[Pg 232] Errors in Diet.—The majority of the ills from which the baby suffers can be traced primarily to errors in diet and in most of these cases the treatment consists chiefly in adjusting the formula to suit the condition. As a rule, these errors may be placed under two heads: those that are brought on by under-feeding and those induced by over-feeding. The pathological conditions arising from under-feeding are due not only to a lack of food, but chiefly to the improper balancing of the different food constituents in the formula. As has already been stated, so much food is required to cover the energy expenditures, so much for maintenance, and so much for storage for the growth and development necessary during the entire period from birth to maturity. These constituents must be regulated to the individual needs of the infant.
Over- and Under-dilution.—If the dilution is too great, the infant, while receiving the correct amount of the mixture, may have the necessary food constituents so reduced as to have them fail completely to do their appointed work in the body. Or if the amount of diluent is too small the baby may be receiving too strong a mixture, and develop nutritional disturbances therefrom. Under the first head the child suffers from under-feeding; the appetite is satisfied before enough of the actual food is ingested to meet his various needs. However, it is probable that the artificially fed infant suffers from the results of over-, rather than of under-feeding.
Gastro-intestinal disturbances, colic, enterocolitis, colitis, etc., rickets, scurvy, nephritis, and diabetes are among the diseases most apt to develop from injudicious feeding, and in these cases the dietetic treatment plays the most important part in combating the condition. The disturbances caused by food are recognized by the general symptoms: [Pg 233] vomiting, rise of temperature, subnormal temperature, and the stools, the latter being the chief point of observation.
Fats as Cause.—When the fats are causing the disturbance, the rise of temperature is apt to be high, but not of long duration. The baby vomits frequently, the vomitus being acid in reaction and odor, the latter due to the presence of fatty acids, butyric acid, etc. Diarrhea often develops in a more or less acute form. In these cases there is a loss of sodium and other alkaline salts in the feces, and a consequent excess of ammonia in the urine, resulting in acidosis. Acid intoxication has been known to develop as a result of this loss of alkaline salts. The chief symptoms of this condition are rapid and deep respiration, stupor or restlessness, and cherry-red lips.[84]
Symptoms of Excess Fat in Diets.—The general symptoms in infants receiving an excess of fat in their food take the form of loss of appetite, with more or less loss of weight, or failure to gain. When the cases are not chronic, soft curds may often be seen, which are at times mistaken for casein curds, but may be distinguished from them by their translucent appearance and their solubility in ether. The color of the stools due to the excess of fat under the above-mentioned conditions is shiny and gray. In the majority of cases, especially of a more chronic character, the stools are apt to be large and dry, at times hard and crumbly. The fat in such stools is combined with magnesium and calcium salts, forming the characteristic “soap stools.”[85] The combined loss of these salts in the feces has a definite effect on the general metabolism and nutrition, giving rise to rickets.
Regulating the Fat.—The treatment consists chiefly of regulating the amount of fat in the formula, and of cutting it out altogether in the beginning when the symptoms [Pg 234] show acute acid conditions. In many cases, if the baby is given breast milk, the trouble disappears. At other times it is necessary to substitute a foreign fat such as olive oil for the butter fat. Dr. Ladd in the Children’s Hospital in Boston treated many babies who manifested an intolerance for butter fat with “Homogenized Milk,” which consisted of skimmed or separated milk and a certain percentage of olive oil, placed in an apparatus which brought about a more complete division of the fat, causing it to mix with the milk as an emulsion closely resembling human milk.
Fat intolerance is most difficult to overcome, the baby being apt to relapse into the acute stage unless the utmost caution is observed in adding the fats to the formula. It is not safe, however, to feed the baby upon a fat-free milk for any great length of time.
Excess Protein in Food.—The digestional disturbances arising from too much protein in the food are as a rule readily overcome in breast-fed infants. When it is due to nervousness or worry in the mother, it disappears as soon as the mother ceases to worry or does something to remove the cause of the nervous condition. When the breast milk is high in protein, more exercise in the open air at times adjusts the percentage of protein, provided the mother does not become over-tired, in which case the percentage of protein in breast milk increases.
Evidences of Excess Protein.—The symptoms of excess protein in the diet of the breast-fed baby are colic and flatulence, which are often persistent and difficult to overcome. Vomiting is not so common in these babies as in those who are artificially fed. The stools are increased in number, are either brown or green, and generally loose and watery. In artificially fed infants the symptoms are much the same, except that the vomitus often contains large curds which are tough and leathery. The baby suffers from gas formation and colic. The stools are at times normal, except [Pg 235] for the presence of large, hard curds; at other times they are increased in number, and are of a watery consistency and alkaline in reaction.
Regulating the Protein in Formula.—When the stools are watery and brown and musty in odor as the result of disturbed protein digestion, the treatment consists of taking out the proteins from the formula and of substituting cereal water, to which dextri-maltose or milk sugar is added, the milk being added as soon as possible to prevent too great a loss of body protein. As a rule the whey proteins do not cause the disturbances so often as the casein proteins; and at times it is possible to use whey mixtures with babies who cannot tolerate the casein at all.
Buttermilk also is used in cases of protein indigestion, as is Eiweissmilch and peptonized milk.
Regulating the Carbohydrates.—When the disturbances are due to the carbohydrates in the formula, they may be digestional or nutritional. In this form the milk sugar is more apt to be the cause of the trouble than the dextri-maltose preparations which are at times used. In the latter, when the disturbance becomes nutritional, the cause of the trouble can usually be traced to an excess of starch. When the percentage of milk sugar is greater than can be handled by the digestive apparatus of the baby, it is manifested by frequent attacks of colic, with the passage of watery green stools, highly irritating, in character on account of their acidity. In acute cases the loss of weight is often marked, and symptoms of intoxication may develop. The outlook is grave in the very severe cases, but if the baby can survive forty-eight hours after the acute symptoms develop, he is apt to pull through the attack.
Adjusting the Sugars.—The treatment in these conditions consists of eliminating the milk sugar from the formula; in less severe cases dextri-maltose may be substituted. As a rule, coincident with indigestion caused by [Pg 236] sugar there will be found to be an intolerance for much fat, so that this must be adjusted as well as the milk sugar. Skimmed milk mixtures, containing a certain amount of barley or oatmeal water, are generally found to be suitable in these cases. Dextri-maltose may be added after a few days in order to maintain the fuel needs of the body. Eiweissmilch is at times used, but whey mixtures are contraindicated on account of their high sugar content.
Dextri-maltose also disagrees at times. The baby has colic and flatulence, the stools are usually loose or watery and dark brown in color. The dietetic treatment consists of an immediate withdrawal of the dextri-maltose preparation and a substitution of milk sugar after a few days.
Evidences of Excess Starch in Formula.—The disturbances arising from an excess of starch in the diet are, as has already been stated, more apt to be of a chronic than an acute character. Vomiting is not a common symptom under these conditions, although colic is frequent. The stools are at times loose and brown, at other times dry and small. The baby at times suffers from diarrhea and at others from constipation. When the disturbance is acute the starch must be entirely eliminated from the formula. If proprietary foods are being used containing starch, whether it is dextrinized or unchanged, they must be at once abandoned, and a formula made up of protein with sugar and fat.
| Fat | 1.00% | or | Fat | 2.00% |
| Milk sugar | 4.00% | Milk sugar | 5.00% | |
| Protein | 0.75% | Protein | 1.25% |
They likewise advise whey and whey mixtures under these circumstances.
Fermentation.—Fermentation is often the cause of infantile indigestion. At times it is acute and may cause a decided elevation of temperature owing to the absorption [Pg 237] of the toxic substances formed as a result of the bacterial action. In almost every case of indigestion brought on by fermentation there will be an accompanying diarrhea. As a rule the carbohydrates are more liable to the attacks of bacteria in the stomach than the other food constituents.
Treatment.—The treatment consists first of starvation, no food being given for at least twenty-four hours. Then water or weak tea, sweetened with saccharin, may be given, but nothing else. The medical treatment must be left to the discretion of the physician. When the condition warrants a return to food the formula must be made weaker than that which has caused the disturbance. Malt soup mixtures, buttermilk mixtures, whey and albumen water may be added as the condition of the baby improves. In older children the period of starvation may have to exceed that of infants, but a gradual return to normal diet is made. Weak tea and toast may be given after the first twenty-four hours and well skimmed meat broths, soft-cooked eggs, liquid peptonoids, and malted milk added to the diet as the condition of the child improves.
The dietetic treatment for enterocolitis must be adjusted according to the principal symptom. In some of these cases diarrhea is most prominent, while in others constipation is the most marked symptom. Hence the diet must be such as not only to do no harm to the child, but one that will aid in his ultimate recovery.
The treatment for diarrhea, whether it is from fermentation or putrefaction of food, has already been explained. The grave danger in the putrefactive diarrhea is the absorption of the toxic substances which result from bacterial action upon the unabsorbed food material in the small and [Pg 238] large intestine. In these cases auto-intoxication may develop and the baby may die before the condition yields to treatment. The entire intestine must be cleansed as a rule. The stomach of the baby may be reached with little trouble by using a small rubber catheter attached to a glass funnel and a solution of bicarbonate of soda. The bowels may be emptied by means of a soapsuds enema. Older children may be given oil, but this of course comes under the jurisdiction of the physician.
Constipation is one of the most frequent troubles visited upon people of all ages. “It is not a disease, it is a condition in which the number of stools is less or the consistency of the stools is greater than is normal for the individual at the given time.”[86] It may be caused by neglect of the bowels, which should be evacuated once or twice every day during infancy and once a day after that period. If the habit of emptying the bowels every day is established in infancy it adds much to the health and comfort of the individual during the entire remainder of life. Babies are sometimes constipated as the result of the opium administered in soothing sirups. Others inherit constipation, while still others are constipated by the taking of the wrong kind of food or too little food. In any case it is decidedly bad to resort to drugs, since the habit of taking cathartics is so easily acquired and so difficult to overcome.
Factors Inducing Constipation.—With artificially fed babies a formula which contains too high a percentage of diluent and too low a percentage of solids will cause constipation, chiefly because the solids are so completely absorbed that they have no residue to form feces. A formula with too low a fat content in proportion to its protein and [Pg 239] carbohydrates may cause constipation because the latter two constituents are almost entirely absorbed, and the feces, which is largely made up of the fat, is correspondingly small. Excess of fat, however, has been proved to be one of the chief causes of constipation in infants, as has also been the case with excess starch. Boiling the milk for the baby at times results in constipation. Hence sterilization is more frequently to blame for the condition than the pasteurization of milk.
Constipation during Second Year.—During the second year, if the child is given too much milk and too little solid food, constipation is very apt to be the result. A maximum quantity of from thirty-two to forty ounces may be given. In many diseases brought on by malnutrition, constipation is an obstinate condition to be overcome. This is especially the case in rickets and anemia.
Use of Laxative Foods.—After the baby is a few months old, orange juice is given between the morning feedings. Malted foods likewise exert a laxative effect. The higher the percentage of maltose, the more laxative the food. The nurse must keep this point in mind in feeding babies. With older children and adults, the question of diet for constipation is quite as important as it is for infants. Prunes or figs cooked with senna leaves and thoroughly strained furnish an excellent adjunct to the diet under such conditions. The coarse breads such as bran and Graham or wholewheat bread should be used instead of white flour breads. Care should be taken in advising a cereal diet for children, since cereals, with the exception of oats, are apt to be constipating. Fresh fruits, stewed fruits, and fresh vegetables are all good under the above-mentioned conditions. Young children require the vegetables strained or cut fine. Adults should include one coarse vegetable a day in their dietary to obviate the development of constipation. Children should be taught to drink plenty of water, and [Pg 240] babies should not be neglected in this respect. As a rule very few adults drink as much water as is necessary for the general welfare of their bodies.
There is probably no disease of infancy which has come in for more study in the past few years than scurvy.
Cause.—The disease is believed to be directly due to a deficiency in the diet of the antiscorbutic vitamine, known as “Water soluble C.”
Treatment.—For many years it was known that lime juice exerted a curative effect upon scurvy. But recently the efficiency of this fruit juice has proved to fall far short of that effected by either orange, or tomato juice.
Feeding experiments have proved that animals, fed upon rations consisting of dry food without the addition of green, will develop scurvy. And that the milk of such animals will show a deficiency in the “C” vitamine which will lead to a development of the disease in infants fed upon such milk.
Milk is, in fact, by no means a perfect food, so far as its vitamine content is concerned. First, because the presence of the vitamine in milk is so dependent upon the diet of the mother or the animal, second, because the pasteurization temperatures used to insure cow’s milk of purity from a bacterial standpoint, destroys in it the greater part of its antiscorbutic power. Either of which makes it necessary to supplement the formula of the artificially fed infant, and, in case of the former, the mother’s milk of the breast-fed baby, with orange, or canned tomato juice.
The amount of either of the fruit juices which is necessary to insure the child of a freedom from scurvy, is small, ranging from one-half to one ounce of strained juice daily, this amount is increased gradually until the child is taking from one and one-half to two ounces each day. It has been [Pg 241] found advisable to administer the fruit juice between the two morning feedings. As a rule, the fruit juices are given at the beginning of the seventh month, but they may be given at a much earlier date, the time being adjusted by the physician.
Rickets, like scurvy, is being discussed by scientists both in America and abroad. The disease is widespread, particularly in its subacute form, and its effect upon the health of the child is so serious that no amount of effort to prevent its development should be considered too great.
Calcium Retention in Rickets.—The disease is characterized by a failure of the bones to lay down lime salts, this failure causes a softness and flexibility in the structure of the bones which permits them to bend into deformities. Then, too, it is a well established fact that any interference with the calcium metabolism in the body, will inevitably bring about disaster. (See Mineral Metabolism, page 185.)
Factors Inducing Rickets.—According to Dr. Eddy, “It is impossible at present to determine whether rickets is a true avitaminose or a consequence of deficiency in a series of factors.”
Treatment.—For breast-fed babies it is necessary to adjust the diet of the mother to include more of the vitamine bearing foods, since milk contains vitamines only in proportion to the amount eaten in food. For artificially fed children, the giving of cod liver oil has recently been adopted as the surest and safest method of curing and preventing the development of the disease. Like treatment is used with breast-fed infants if the need arises.
The value of cod liver oil in this respect has only been recently recognized. Mellanby of England claims that the oil owes its curative and preventive properties to the presence of the “A” vitamine. But scientists in this country [Pg 242] have not fully accepted this view. Eddy states, “It may be that the power of the oil is due to its ‘A’ vitamine content, in which it is known to be rich, or it may be due to a new vitamine, but the fact that the oil is a preventive in this respect gives the pediatrist another agent to insure normal growth.”
Sunshine as a Factor.—It has been found that the disease rickets is more prevalent in winter than in summer; this is believed to be due to the fact that sunshine during the summer months exerts a distinctly beneficial influence over the disease. Dr. Hess’s report of the good results which he has found to be derived from the use of the ultra violet rays as a substitute for sunshine in winter, would seem to confirm this view.
Malnutrition is not confined to the children of the poor, though it is more common with infants of parents who have not the means to secure the best milk and give them the benefit of wholesome surroundings and plenty of sunshine. But babies of people in moderate circumstances, and even of wealthy parentage, are at times badly nourished, and require the same exacting care, the same attention to the food, the fresh air, and the sunshine that the poorer babies need in order to survive. Malnutrition may be the result of insufficient food, and it may also be due to the lack of one definite food element. Again, it may be brought on by some deformity of the mouth or stomach, which make it impossible for the baby to get all the food which he requires for his maintenance and growth. He may be born prematurely and his digestive apparatus not be sufficiently developed to care for the amount or type of food necessary for his needs, or he may have some congenital weakness which interferes with the absorption and assimilation of his food. All of these points must be considered.
[Pg 243] Evidences of Correct Feeding.—If the baby shows a steady gain, both in weight and growth of stature, without digestional disturbances, the food given him is probably correct, but it must be kept in mind that nutritional disturbances, such as rickets and scurvy, are slow in developing, and do not manifest themselves with anything like the rapidity of digestional disturbances. Hence the nurse must take care as far as she is able, not only to prevent the food from causing indigestion, but also to see that it is not given in such a form as to induce those graver and more lasting nutritional disturbances which affect the entire system from infancy throughout the life of the individual.
Breast Feeding versus Artificial Feeding.—There is no doubt about the fact that the breast-fed baby suffers less from digestional disturbances and has more resistance to disease than the baby fed even upon a perfectly prepared artificial food. The majority of diseases manifested by artificially fed infants have their origin in the following errors in diet.
Over-Feeding.—Resulting in acute gastro-intestinal disturbances (colic, enterocolitis, colitis, constipation).
Under-Feeding.—Resulting in chronic, and acute deficiency diseases (scurvy, rickets, malnutrition).
Evidences of Dietetic Errors.—The stools, showing characteristic evidences of excessive quantities of, protein, fat, or carbohydrates in the formula. Loss of weight or failure to gain. The development of deficiency diseases (scurvy, rickets, xerophthalmia, rickets and malnutrition).
Evidences of Correctness in Feeding.—Normal gain, freedom from gastro-intestinal disturbances, and deficiency diseases. Rosy cheeks, bright eyes, and a vigorous body.
Treatment in Abnormal Conditions.—The treatment [Pg 244] consists in adjusting the diet to meet the needs of the particular disturbance manifested. Plenty of fresh air, sunshine and sleep.
Relapse.—One danger which the nurse must always be on the lookout for is the relapse into the acute stage. The diet is the chief treatment. In acute gastro-intestinal disturbances rest from food is essential for at least twenty-four hours. Some infants can easily endure starvation for this short period. However, when malnutrition has already been established, it is not wise to carry out the starvation treatment over-long. A cautious return to a normal diet may be made as soon as acute symptoms disappear.
Fevers in General.—It requires very little deviation from the normal to raise the temperature of a child. A slight attack of indigestion, a slight soreness of the throat, will bring up the temperature of some children out of all proportion to the seriousness of the disorder.
Diet in Fevers of Short Duration.—As a rule, in the fevers of short duration, such as intermittent fever, malarial fever, etc., the diet is a simple matter. Milk is given when it agrees, with buttermilk, koumiss, broths, and albuminized beverages to vary the diet.
Diet in Infectious Diseases.—When, however, the fever is induced by specific bacteria, such as in the case of typhoid and scarlet fever, the diet is a different matter altogether. The disease may be one in which the diet is the chief item of importance; such is the case with typhoid and scarlet fever, with the former because of its long duration, the increased rate of metabolism due to both the fever and the action of the bacteria making it necessary to increase the normal amount of food to meet the new requirements of the body; and with the latter on account of the kidney complications which must be guarded against, and which can only be handled by regulating the diet.
Infant Feeding.—The feeding of infants under febrile conditions resolves itself into an adjustment of the milk [Pg 244a] formula to meet the existing state of affairs. The digestion is always more or less disturbed by fever, especially during the early stages.
Restricting the Food.—It is not always possible to diagnose the disease immediately, so that the safe thing to do is to lengthen the intervals between the feedings for the breast-fed baby and to stop food entirely for twelve to twenty-four hours for those who are artificially fed, when there is any doubt as to the cause of the rise of temperature. Some mothers find it difficult, if not impossible, to institute this period of starvation. In these cases barley water or albumen water may be given at stated intervals. Many physicians give very weak tea, slightly sweetened, under the above conditions; it does no harm to the baby and relieves the mother from the belief that her child is being starved to death. In twenty-four hours, if the fever arises from disturbed digestion, some manifestation of the condition will be observed.
Bacterial Activity.—In cases of intestinal putrefaction the fever is apt to rise at an alarming rate and is controlled only by removing the cause. The proteins which have escaped digestion and absorption in the intestines furnish the best medium for the growth of putrefactive bacteria. Hence this food constituent must be given in its most digestible form.
Dietetic Treatment.—Milk in most instances is the best form in which to give protein food, especially to young children and babies. At times, however, it will be found that milk disagrees; it must be peptonized, or one of the fermented milks, such as buttermilk (Bulgarian culture), Eiweissmilch, or koumiss must be substituted. In cases where the putrefactive bacteria make it unwise to use milk at all, for a time the proteins should be furnished in the form of cereal gruels, and the juice of an orange strained and diluted given once or twice a day between the morning and evening feedings.
[Pg 244b] Whey is contraindicated in cases where the fever is brought on by putrefaction in the intestine, chiefly because it furnishes one of the best mediums known for the growth of the offending bacteria.
Patience is required in handling the diet for fevers in infancy. As has already been stated, it requires a very slight cause to raise the temperature of a child, but for this very reason especial care must be observed that no enlightening symptom escapes the notice of the nurse.
Complications.—Tuberculosis or scurvy may be in an incipient stage, and may be overcome if recognized in time. The nurse has a better opportunity for observing changes in an infant or child under her care than the physician who comes once a day or less. The nurse should make note of these changes, that the physician may have a chance to regulate the diet accordingly.
Fluid Diet.—With children, as with adults, the energy output in fever is greater than in health, hence the need for plenty of fluids to help eliminate the waste products due to the increased metabolism. These fluids may consist of water, fruit beverages, cereal water, whey, and broth. It is well for the nurse to remember that when the child is confined to bed, he will not need so much food as he would if he were up and about, but that if the fever is of long duration, as in typhoid, the increased rate of metabolism must be met by an increased amount of food, as the ordinary requirement standards for a child in health cannot be applied to the diet of a child under these conditions.
Scarlet fever is an acute infectious disease, characterized by high fever, sore throat, a red rash, and a tendency to nephritis. The disease usually begins suddenly with an attack of vomiting; the temperature rises to 104° or 105° and on the first or second day a rash appears, first on the chest and neck, and spreads over the entire body. This lasts [Pg 244c] from three to seven days, desquamation begins soon after the rash disappears and lasts from two weeks to six, the palms of the hands and soles of the feet peeling last. The appearance of the tongue is very characteristic, being coated, and through this coating are seen a few bright red points, producing the well-known strawberry tongue. After a few days the coating disappears, leaving the tongue bright red. In mild cases the tonsils are enlarged and the throat very red. In severe cases there may be difficulty in distinguishing the disease from diphtheria without a culture being taken. The tendency of the child to develop nephritis during the second or third week makes the treatment largely dietetic in character.
Dietetic Treatment.—Milk is the chief diet for the first three weeks. If it disagrees, it should be modified or peptonized to suit the condition. Koumiss and buttermilk may be substituted when it is impossible to prepare the milk so that it will not cause digestional disturbances. This, however, is seldom found to be the case during infancy. Malted milk and even condensed milk, or some of the dextrinized and malted foods at times prove valuable when whole milk disagrees. But the nurse must remember that a baby runs a risk of developing nutritional diseases of a grave character if fresh milk is eliminated from the diet for any great length of time.
Older children may have plain vanilla ice cream and plain junket, oyster or clam broth made with milk, the oysters and clams carefully strained out. Lemonade and orange juice may be given, but no meat broths or albumenized beverages or egg dishes can be admitted to the dietary.
Development of Nephritis.—Nephritis must be guarded against. The skin, being covered with a rash, is put out of commission as an excretory organ; in consequence all of the work of this description is placed upon the kidneys. In the first part of this text the work of the kidneys was defined; [Pg 244d] it was found that they were the chief organs for the excretion of the end-products of protein metabolism. It can be readily understood that when these organs are given not only their own work but that of the other organs to perform, unless the food requiring the greatest amount of effort on the part of the kidneys is confined to those types which can be most easily taken care of, such as milk, the kidneys stand a great chance of becoming impaired. Such is the case in nephritis.
Convalescent Treatment.—The return to normal diet must be made with the greatest caution. Specimens of urine must be taken often, for in this way alone can the development of nephritis be reckoned with.[87] Should nephritis develop in spite of efforts to prevent it, a farinaceous diet[88] such as is given in these conditions must be resorted to.
After three weeks, if the patient shows no disposition toward nephritis, and if convalescence is progressing satisfactorily, the diet may be increased day by day, adding milk toast, cereals, cream soups, rice, baked potato, then custards and soft eggs, the soft part of oysters, broiled or baked fish, broiled breast of chicken, and, still later, rare beef and lamb chops. Meat, however, must not be given until all danger from nephritis has passed.
Diphtheria.—The feeding in diphtheria follows the régime given in acute fevers. The body must be kept in good condition. At the same time it is necessary to understand the complications which make the dietetic treatment of this disease assume a place of importance.
Complications.—It may be complicated by broncho-pneumonia, albuminuria, carditis, endocarditis, and dilatation of the heart. Anemia must be combated, but care should [Pg 244e] be used not to push the diet to such an extent as to impose too great a tax upon the already weakened heart.
Dietetic Treatment.—While the fever lasts the diet must be fluid, milk, buttermilk, malted milk, and some of the proprietary infant foods such as Mellin’s Food, Eskay’s Food, and like preparations. Milk gruels, made with milk and some cereal such as farina, barley flour, fine cornmeal, arrowroot, strained oatmeal, etc., are at times more easily swallowed than the unthickened liquids. Liquid beef peptonoids, panopeptone, and like predigested beef preparations prove valuable in many cases.
Convalescent Diet.—As convalescence progresses, or in cases where the patient finds it easier to swallow a semi-solid than a liquid, soft custards, gelatin, well-cooked cereals, and ice cream may be given. Eggnog and milk punch are at times given, but only upon the advice of the physician in charge.
Rectal Feeding.—When the condition of the patient makes it necessary to nourish in other ways than by mouth, nutrient enemas[89] may be given. In certain cases of diphtheria, young infants can be fed more successfully through a tube inserted by way of the nose into the stomach than by feeding in the ordinary way. The formula is prepared in the same way as for bottle feeding, and is poured into a glass funnel and through the soft rubber catheter into the stomach. Care must be observed to prevent the patient struggling on account of the heart weakness which invariably complicates this disease.
In the early months of life it is probable that whooping cough is one of, if not the most fatal of the diseases to which the infant is subjected. The period of incubation of this disease is from one to two weeks, the cough at first not appearing different from those accompanying colds of all [Pg 244f] sorts. However, in from ten days to two weeks the characteristic whoop occurs, differentiating this disease from all others. The symptoms aside from the whoop are the difficulty of taking breath and the great prostration after the paroxysm and the frequent vomiting of the food, brought on by the violent coughing.
In very young infants the whoop does not always occur. But the child coughs and holds its breath until it is blue in the face. At times young babies may have convulsions. The so-called spasmodic stage, during which the child may have from a few to a great number of paroxysms of coughing a day, lasts from a month to six weeks, and in some cases even longer. As the disease declines the cough gradually disappears and the child appears to be suffering with ordinary bronchitis. The characteristic whoop may return at any time during the ensuing six months or year if the child has an attack of bronchitis and is inclined to cough.
Complications and After-effects.—The complications and after-effects of whooping cough give it a serious character. Hemorrhage may occur from the nose. According to Ruhräh: “Paralysis may follow from meningeal hemorrhage, broncho-pneumonia, acute emphysema, and collapse of the lung may occur. Diarrhea, convulsions, and albuminuria are also met with. Tuberculosis and chronic bronchitis may follow.”[90]
Dietetic Treatment.—The diet plays an important part in whooping cough. The serious complications and after-effects of this disease upon children necessitate a rigid observance of dietary laws. With infants it is always best, when it is possible, to give breast milk. As this is the natural food it requires less effort on the part of the digestive apparatus to become available. It has been proved that even during the time when the baby is nursing the milk is projected in spurts into the duodenum without waiting to be attacked by digestive enzymes in the stomach, and [Pg 244g] for this reason the breast-fed infant is more apt to be efficiently nourished than the artificially fed baby, who loses his dinner by vomiting before absorption has had a chance to occur.
Diet under Ten Years of Age.—For children under ten years, a fluid diet is necessary, at least in the beginning of the disease while there is a fever, and later, if the vomiting is persistent. Milk, buttermilk, koumiss, broths, albuminized beverages, and cereal gruels such as barley and oatmeal gruel and arrowroot gruel can be given. Later, if the fluids are retained, cream of wheat, farina, junket, soft custards, and soft-cooked eggs may be added. Care must be taken in giving toast, unless it is softened with milk or broth, for the crumbs may bring on a paroxysm of coughing and vomiting. The best results in feeding with whooping cough are obtained by giving the food in small quantities and oftener. A few ounces given every two hours are less apt to be vomited than a larger quantity. It is also easier for the child to take the small amount after an attack of coughing and vomiting than it would be for him to attempt a larger meal.
Use of Stimulants.—In many cases where weakness is great, it has been found advisable to add some stimulant to the diet. With infants this is best given in albumen water, a small amount of good brandy acting better than other stimulants. With young children some of the predigested liquid beef preparations, such as liquid peptonoids, are found valuable. These foods are given alternately with the other fluid foods.
Hygiene and Sanitation.—Infants and children suffering with whooping cough require plenty of fresh air and sunshine. They must be kept out of doors as much as possible and sleep in well-ventilated rooms or sleeping porches. They must be protected from drafts and excitement, and never allowed to become over-tired. In this way the anemia which so often results from prolonged attacks of whooping cough is in a measure held in check. At times it is found [Pg 244h] necessary to give some kind of an iron tonic, but this comes under the jurisdiction of the physician instead of the nurse. When bad effects do occur in spite of all the care exercised during the attack of whooping cough, they must be accorded the treatment especially devised to meet the situation.
This is an acute, infectious disease characterized by a red eruption which appears on the fourth day. Measles is one of the most contagious of all the diseases of childhood. It may be acquired by direct contact with another case or by being in the room with a case. The infection may also be carried through the air and occasionally by a third person. Measles is more prevalent in the winter than in summer. In cities it often occurs in epidemics. The period of incubation is from ten days to three weeks, occurring generally at about two weeks after exposure.
The attack may begin with the child showing a languid attitude, complaining of headache. Then a cough develops, with nausea and fever at times. The fever is often high, reaching 104° F. on the second day. As a rule the fever gradually falls after the second day and becomes normal in almost a week. However, the temperature varies in different cases.
Complications.—Measles is not considered dangerous in itself, but the after-effects sometimes prove fatal. This is especially the case in broncho-pneumonia, which frequently develops during or after the attack.
The gastro-intestinal, as well as the respiratory, tract is attacked in measles, diarrhea being especially common. Very weak children have been known to develop gangrenous stomatitis; paralysis and tuberculosis[91] likewise develop in some cases as the direct result of measles.
Thus it is demonstrated that measles is not to be lightly treated. Even if it is not in itself fatal, the results of the [Pg 244i] disease are so dangerous that the care of the nurse is especially necessary. The great trouble is that so often a nurse is not in attendance and the child suffers through ignorance of the mother.
Dietetic Treatment.—The dietetic treatment of measles is important. For infants milk is the exclusive diet, the formula for bottle-fed babies having to be weakened on account of the catarrhal condition of the gastro-intestinal tract. For older children it is necessary to confine the diet to fluids as long as the fever lasts, and at times longer if the stomach gives evidence of digestional disturbances. Milk is the chief food, with milk soups, buttermilk, and koumiss used to vary the diet. Orangeade and lemonade may be given to allay thirst. A return to normal diet must be made gradually, giving cereal gruels, milk toast, and broth before the more solid articles of diet suitable to the age of the child. When there are complications they must be treated, as in whooping cough, according to their symptoms.
Gastro-intestinal Disturbances are responsible for much of the fever manifested during infancy and childhood.
Infectious Diseases are all more or less accompanied by an elevation of temperature.
Incipient Diseases, especially tuberculosis and scurvy, may likewise cause a rise of temperature. The relief of either disease or the fever depends largely upon how quickly the conditions are discovered and the means instituted to overcome them.
Metabolism in Febrile Conditions of children, as well as of adults, is rapidly increased, hence the energy output is greater, and for this reason the fluid intake must be augmented in order to eliminate the toxic substances produced as a result of the rapid breaking down of the body tissues.
The Kidneys are more or less strained to eliminate the products of the increased metabolism and for this reason it [Pg 244j] is especially necessary to adjust the diet in order to limit, as far as possible, the foods which add to the burden already imposed upon the organs of excretion.
The Skin is an organ of excretion which, under normal conditions, shares the work of the kidneys. In infectious conditions, accompanied by eruptions which more or less cover the entire surface of the body, this organ is temporarily out of commission, hence its work, as well as their own, must be accomplished by the kidneys.
Dietetic Treatment in the majority of infectious diseases may be divided into three periods: Starvation, Fluid Diet, and Convalescent Diet.
Starvation, during which time no food is given for twenty-four hours or longer, in order to allow the digestive apparatus to rest and to give time for any substance which may be causing the elevation of the temperature to pass from the body. This treatment is also wise because it furnishes an opportunity for the symptoms of the disease to manifest themselves; Fluid Diet, given when acute symptoms subside, and Convalescent Diet when danger from relapse is over.
Scarlet Fever is treated with two main ideas in view—preventing the development of nephritis and relieving the condition should it develop.
Dietetic Treatment is logically the only means of treating or relieving nephritis. For the first three weeks, during which time this complication is apt to develop, a milk diet is necessary. This may be in the form of whole milk, milk soups, malted milk, etc. At the end of this time, if there are still no symptoms of nephritis, a convalescent diet, beginning with cereals and soft toast and progressing through the simple digestible foods such as rice, baked potatoes, soft eggs, etc., may be given. This is continued until the patient is well on the road to recovery. Meat should not be added until practically all danger of nephritis is passed.
Nephritis.—If, during the course of the disease this [Pg 244k] complication, should develop, the treatment described for acute nephritis on page 336 should be immediately instituted.
Diphtheria.—Dangerous complications at times develop as a result of diphtheria, making the treatment of this disease of the utmost importance. Heart symptoms, pneumonia, albuminuria, and anemia are among the complications to be dreaded and combated.
Dietetic Treatment in diphtheria is most important. It consists of a fluid diet made up of milk, malted milk, or buttermilk. At times the condition of the throat makes a slightly thickened mixture more easily swallowed than one which is distinctly fluid in character, and for this purpose farina, arrowroot, or barley flour may be used.
Increasing the Diet.—As convalescence advances the semi-solids, soft toast, soft custards, gelatin, and cereals may be given. Should the heart show symptoms of being affected, the intake of fluid must be restricted.
Gavage and Rectal Feeding are at times necessary. Infants may be successfully fed by passing a small rubber tube through the nose into the stomach and administering the milk formula to which they are accustomed. Rectal feeding is likewise valuable in cases of extreme anemia accompanying diphtheria.
Care must be observed by the nurse in giving gavage to babies, since any struggling on the part of the child may result in death from heart disease.
Whooping Cough.—On account of the character of the disease and the proneness of the stomach to eject the food during paroxysms of coughing, dietary measures are more or less necessary in order to enable the child to receive sufficient food to cover his daily needs.
Complications.—Hemorrhage, pneumonia, albuminuria, diarrhea, and convulsions may occur during the disease, while tuberculosis and chronic bronchitis may follow as after-effects.
Dietetic Treatment.—Breast milk is by far the best food [Pg 244l] for the baby, in this as in all conditions. In whooping cough the fact that this fluid leaves the stomach almost as soon as it enters lessens the chances of the baby losing its meal by vomiting it.
Older children do well with frequent small meals, since they are not so apt to give rise to pressure which brings on the paroxysms of coughing and vomiting. When the meal is vomited, a second should be given in order to keep the child from suffering from malnutrition.
Stimulation is found to be necessary in certain cases. Albumen water containing a spoonful of brandy or some of the prepared beef preparations, such as liquid peptonoids, may prove valuable under the circumstances.
Measles.—Complications and after-effects developing as a result of measles make the dietetic treatment of this disease important. Gastro-intestinal disturbances, especially diarrhea, are apt to occur, and tuberculosis has been known to develop as a result of measles.
Dietetic Treatment.—The fluid diet as used in any acute febrile condition is used as long as the temperature is elevated. Milk, buttermilk, malted milk, and milk soups constitute the chief items in the diet. Orangeade and lemonade are found valuable in relieving the thirst.
(a) List the evidences of errors in the diet of infants; show how they may be corrected in the formula.
(b) Outline the processes in the preparation of Eiweissmilch (protein or albumen milk). What constituent is particularly low in this milk, and how was its reduction accomplished?
[84] “Diseases of Nutrition and Infant Feeding,” by Morse and Talbot.
[85] Ibid.
[86] “Diseases of Nutrition and Infant Feeding,” p. 307, by Morse and Talbot.
[88] Consisting of cereal gruels, rice, and other starchy foods.
[90] “Diseases of Infants and Children,” p. 326, by Ruhräh.
[91] “A Manual of Diseases of Children,” p. 319, by Ruhräh.
Predisposing Factors.—The majority of diseases affecting the stomach have as their predisposing factors, and owe their development to, one or all of the following conditions: (1) errors in diet; (2) disturbed secretory processes; (3) disturbed motility and tone.
It is probable that in the beginning the first factor was the chief offender in the case, bringing about the development of one or both of the other conditions. The other factors to be considered in this respect are heredity, occupation, poverty, and diseases which involve to a greater or lesser degree the digestion of the stomach and intestines. A child may inherit a weakened organism through excesses or disease on the part of the parent. If this weakness is not overcome while the child is growing, the probabilities are that the digestion steadily declines until in adult life it becomes a pathological condition. Lack of fresh air, poor and dirty food, unwholesome surroundings, crowded and badly ventilated sleeping rooms, insufficient water, and overwork, all act in making the digestion bad. These must be overcome if permanent good is to result.
Errors in Diet.—Errors in diet arise more often through ignorance than from any other cause. A child may be allowed to eat any and all kinds of unwholesome and unsuitable food. When the stomach rebels, showing the serious danger signals of nature, medicines are given but the diet is unheeded, until the time comes when even the medicines [Pg 246] fail to give temporary relief, and the organs of digestion are in some instances permanently impaired.
Disturbed Secretory Processes.—Consensus of opinion goes to show that the majority of cases of acute and chronic gastritis (catarrhal) and gastric ulceration are due primarily to a disturbance of the secretory processes, while the impaired motility and lack of tone in the stomach probably influence their development and aggravate the disease already present.
Composition of Gastric Juice.—In a former chapter the processes of gastric digestion were explained. The gastric juice, composed of from 0.2 to 0.3% free hydrochloric acid and several important enzymes and lipases, which act upon the proteins and emulsified fats, must be sufficient in quantity to assure good digestion, and when anything arises to interfere with the secretion of this fluid a deviation from the normal is bound to occur.
Disturbed Motility and Tone.—Again, it has been proved that good gastric digestion, like good intestinal digestion, depends more or less upon the way in which the food mass is mixed with the digestive juices and moved along the alimentary canal. Anything which interferes with the secretion of the juices or delays the food over its normal length of time in the stomach surely exerts unfavorable influences on the general metabolism of the food, for while, as we have already found, gastric digestion is not essential to the final utilization of the food in health, in disease it undoubtedly exerts a marked influence upon the general nutrition of the individual.
The lack of hydrochloric acid in the gastric juice lowers the resistance to bacterial action, for this constituent exerts a decided germicidal influence in gastric digestion, preventing fermentation with the production of organic acids and [Pg 247] probably alcohol. In conditions due to hypochlorhydria (lack of hydrochloric acid) foods which leave the stomach quickly must be given with enough of the other necessary constituents in their simplest and most easily digested form to balance the diet and prevent the occurrence of the other disorders as troublesome as the original disorder.
Dietetic Treatment.—The following points must be kept in mind in formulating a dietary for patients suffering from a deficiency of hydrochloric acid: (1) boil the drinking water to destroy any bacteria which may be present; (2) use carbohydrates in the form of starch rather than sugar, since starch is less liable to fermentation from bacteria than sugar; (3) limit the foods which delay the passage of the food mass from the stomach; fats pass into the duodenum more slowly than other foods and when fed with other foods delay their passage materially; (4) avoid the use of soda bicarbonate, as it tends to reduce the normal acid content of the stomach, thus preventing its germicidal action upon the fermentative bacilli; alkaline carbonates likewise inhibit the flow of gastric juices; (5) give especial attention to the attractiveness of the food served; let it be appetizing and savory, for by such means is the appetite juice and incidentally an increased flow of the gastric juices stimulated; (6) condiments and spices, meat broths high in extractives, and salt foods such as caviar and endives may be given at the discretion of the physician; it is seldom advisable to give the foods which are indigestible, even when they act as stimulants to the secretory cells of the stomach.
(Excess secretion of acid in the stomach)
The Effect of Excess Acid.—An excessive flow of hydrochloric acid has been found to be the cause of much of the acute and chronic gastritis, in fact more of the cases are traceable to an excess than to a lack of hydrochloric [Pg 248] acid. This acid is more or less irritating in character, and the tender mucous membranes lining the gastric organ being constantly bathed in a secretion composed chiefly of acid must necessarily in time suffer a certain amount of irritation and inflammation, causing the development of a pathological condition which may be temporary or permanent, that is, it may result in acute or chronic gastritis, according to the amount of acid secreted and the length of time the hypersecretion is allowed to continue.
Determining the Acid Content of Stomach.—The difference between the cases brought about by an excess flow of hydrochloric acid are more or less difficult to distinguish from those caused by a lack of this constituent in the gastric juice, chiefly because in the latter case the organic acids formed as the result of bacterial action upon the food exert an equally irritating effect upon the membranes of the stomach, and the only sure method of determining the cause of the disturbance is by an analysis of the stomach contents, by which means the percentage of hydrochloric acid is determined.
Lavage.—It has been found advisable, in some cases of acute gastritis which do not yield readily to rest and liquid diet, to wash the stomach and allow a certain period of rest before giving any food; in this way the organ is rid of all of the offending material and thus has a better chance of a quick recovery.
Dietetic Treatment.—The following dietetic treatment for acute gastritis is advised: As the stomach is the chief seat of disturbance, all unnecessary work must be taken from this region for a certain period:
(1) That any obscure cause may manifest itself and the diagnosis may be rendered more accurately and more quickly.
[Pg 249] (2) That by resting the organ the offending materials may pass out of the body and thus prevent further trouble.
Starvation Period.—Twenty-four hours of total abstinence from food may seem extreme, but as a rule in acute cases of gastritis it is the only sane and safe method of instituting a diet and thus beginning to overcome the cause of the disturbance. After the period of starvation the diet is begun with caution.
Fluid Diet.—Fluids should be given first in the form of well-skimmed broths, which may be reënforced with egg or cereal flours when the patient is very thin or anemic. Buttermilk, made with the Bulgarian cultures, koumiss and other fermented milk foods, liquid beef preparations such as peptonoids or panopepton, albumenized orange juice, cereal gruels treated with Taka diastase when it is found necessary, and peptonized milk. These may be given in from four to six ounces at a time, every two hours on the second day.
Increasing the Diet.—On the third day if the attack is slight the diet may be increased by adding toast, softened with peptonized milk, an ordinary serving (3 ounces) of farina, cream of wheat or rice, reënforced meat broth with two crackers, a cup of tea and a slice of toast, and one or two soft-cooked eggs. If the acute symptoms are still present on the third day, the diet advised for the second day must be continued until they disappear.
Convalescent Diet.—On the fifth day, if progress is satisfactory, lightly broiled chicken or a small piece of rare broiled beefsteak may be added to the diet and the meals reduced in number from six to four.
Relapse.—The patient must be warned against overeating or eating any of the articles which are known to cause an acute attack in his individual case, since one attack predisposes to another, and chronic gastritis may develop as the result of the continual gastric disturbance.
The treatment in chronic gastritis is very like that in the more acute form; that is, it must be combated by removing the cause. Lack of fresh air and exercise have much to do with the development of chronic gastritis, but even they combined with a judicious amount of rest would be wasted without a proper adjustment of the diet to cover the main points of the disturbance. As has already been mentioned, the cause may be a lack of gastric juice or it may be an excess of it; it may be intensified by an atonic condition of the organ or from the food passing too quickly into the duodenum.
Test Meals.—As a rule it is not safe to make a snap diagnosis as to the cause of this disorder. Since in many instances the more serious disorders may be traced to a disregard for nature’s danger signals, the physician as a rule advises a test meal, this meal consisting of a glass and a half of water or a cup or two of tea without cream or sugar and from one to two slices of toast or water rolls. In from three-fourths to one hour or longer this is removed from the stomach by means of a stomach pump and analyzed, the result of the chemical and bacterial analyses forming the basis for diagnosis. This meal is generally given in the morning before any other food has been eaten.[92]
Dietetic Treatment.—The foods constituting the diet in chronic gastritis must be of the simplest character and prepared in the simplest manner. No fried foods are permissible. Pastries, griddle cakes, rich puddings and sauces, candies, and alcoholic beverages must be omitted from the diet as well as the following articles of food: pork, veal, shellfish except oysters, sardines, canned meats and canned fish, highly seasoned and spiced dishes, twice-cooked meats, vinegar, [Pg 251] pickles, olives, cold slaw, pickled beets, catsup, mustard, coarse fibered vegetables such as cabbage, old onions, old turnips, and cucumbers, strong tea, coffee, or chocolate, rich cream or dishes made entirely of cream. In cases of excessive acidity due to a hypersecretion of HCl the extractives of meat are contraindicated, hence all gravies and outside parts of roasted meat must be omitted or limited in the diet.
Gastric ulcer may develop without an apparent cause. As a rule, however, it manifests itself in individuals between the years of fifteen and forty, particularly after prolonged digestional disturbances, especially those accompanied by a hypersecretion of acid. As the disease progresses, anemia is more or loss severe, adding difficulty to the feeding problem. Many of the symptoms are like those of chronic gastritis, such as pain. However, the character of this pain may be different, beginning soon after eating and radiating toward the back. This point may be affected by position. As a rule there is a tenderness over the seat of the ulcer. This is detected by palpation. Vomiting is one of the most general symptoms in gastric ulceration. This may begin from one to two hours after eating when the pain is at its height, or it may start as soon as food enters the stomach. As a rule the latter condition is found more often in very nervous women whose mental attitude affects the stomach to such an extent as to make it difficult to give them sufficient food to nourish them.
Hemorrhage.—Hemorrhage occurs in about half of the cases. The bleeding may be profuse and the blood bright red, or it may be less severe and the color of the blood changed by contact with the gastric juices to a dark brown like coffee grounds.
Excess Acid.—Hyperacidity is present in the majority of the cases, the percentage of HCl rising at times fifty per [Pg 252] cent. or more. Other cases occur in which all of the just mentioned symptoms except dyspepsia are missing, the first intimation of the ulcer being hemorrhage or perforation.
The patient with gastric ulcer may recover entirely and never have a return of the trouble, but care and close attention are necessary, since the ulcers are apt to recur, at times a series of ulcers developing one after another. Death may occur from exhaustion or from perforation and peritonitis. Surgical intervention is as a rule necessary when the ulcers persist, as they generally develop at or near the pyloric opening; and the constant development of cicatricial tissue brings about an obstruction of the pylorus, which if not relieved would allow the patient to starve.
Diet Treatment.—There are a number of treatments used in overcoming this condition. After the test meal and the diagnosis, the patient is placed upon a diet directed to overcome the chief symptom; for example, if the ulcer developed as a result of hyperacidity, the diet would be directed toward the relieving of that symptom. Boas[93] divides the treatment into three stages: (1) hemorrhage; (2) the intermediate stage; (3) the convalescent stage.
Starvation Treatment.—The majority of physicians institute a total abstinence period for the first stage, allowing no food or water to be taken by mouth. If the patient is very weak and anemic from the extended course of the disease, nutrient enemas are given from four to six times a day, alternating with saline enemas. This total abstinence continues from three to six days. Some cases have been known to be fed in this way for a month or six weeks with obvious success. However, this is not the rule but the exception. The diet must be adjusted to the needs of each individual, but a few general rules may be found helpful.
Dietetic Treatment.—Milk is the food generally utilized in the beginning. This may require peptonizing to [Pg 253] be digested, or it may have to be modified with limewater. Protein foods require HCl for their digestion. If these foods are fed they will absorb some of the excess acid, and in this way save the already irritated wall of the organ from additional irritation. When protein foods are given they must be in the form of soft-cooked eggs, scraped raw beef or beef juice, milk soups, and like protein foods.
When there is a dilatation of the organ there is more or less danger of fermentation taking place, with the formation of organic acids. These acids are exceedingly irritating, and every care must be observed to prevent their production. The following dietetic régime may be used as a guide in many cases of gastric ulceration:
Milk Diet.—½ glass (4 ounces) of milk peptonized at 115° F. for 20 minutes, every hour for three or four days. After this the interval between feedings is lengthened to two hours and the amount of milk increased to ¾ of a glass (6 ounces). This is continued from a week to ten days. The patient may be given a cup of well-strained meat broth, reënforced with an egg, once or twice a day, to vary the monotony of the diet. During the third week the milk may be given in the form of milk soups. These may be slightly thickened with barley, rice, or farina flour. The soups may be flavored with beef extract, but only a small quantity must be used, owing to the stimulating properties of these substances.
Water as a Stimulus to Gastric Secretion.—Water is exceedingly stimulating to the acid secreting cells of the stomach, hence it is advisable to limit the amount of water taken by mouth, allowing the patient just enough to wash out the mouth without swallowing any. The thirst is relieved by saline enemas.
It has been found, in many cases of gastric ulceration, especially those accompanied by hemorrhage, that glucose gives better results when used in rectal alimentation, than [Pg 254] any other substance. The strength of the solution varies from a five to a twenty-five per cent. solution. The number of glucose enemas given each day must be regulated by the physician. The method used is the same as in other rectal feedings, the enema is given “high,” and the flow regulated (drip-method).
Convalescent Diet.—During the fourth week, if the pain and discomfort are decreasing, soft-cooked or creamed eggs may be added to the diet, together with thoroughly boiled rice, farina, cream of wheat, wheatena and other finely ground wheat foods, wine or fruit jelly, sweetened slightly, or by using a small amount of saccharin for the purpose, junket and plain vanilla ice cream. At the end of the fourth week a very small portion of meat may be given once a day. It may be scraped raw beef spread upon toast or zwieback, or very lightly broiled beefsteak, broiled lamb chop or chicken (breast only), or boiled or broiled sweetbreads or brains. Spinach or green peas pressed through a sieve are the first vegetables allowed. After these young tender carrots and string beans may be given. Tea, coffee, and chocolate are eliminated from the diet. Milk flavored with coffee or cocoa may serve as a hot drink in the morning when the desire or need for such a drink is manifested. Butter is the best form of fat to be used in cases of gastric ulceration, but this must be given with the greatest caution. In cases where this fat is used in the form of cream, the amount must be cut down or entirely abandoned when there are evidences of butyric fermentation. Buttermilk, koumiss, and other fermented milk drinks are often found very satisfactory adjuncts to the diet. These may be given between meals, or at meals they may be substituted entirely for the milk when other foods are being given. They are not sufficiently nourishing to take the place of the milk diet otherwise. Albumenized orange [Pg 255] juice and cream, egg and vichy may be given to add variety to the diet.
Anemia.—When anemia is severe, as is often the case in gastric ulceration, the diet must be reënforced to overcome it. Some of the concentrated milk foods such as plasmon, encasin, sanatogen, etc., as well as the predigested meat foods, such as panopepton, liquid beef peptonoids, and like preparations, may be used to reënforce the diet.
Bland Diet.—In certain cases of gastric ulceration it has been found more advisable to use what is known as a bland diet. This consists of farinaceous foods such as farina, arrowroot, cream of wheat, corn meal, wheatena, malted breakfast foods cooked thoroughly and given in the form of gruels, and some of the proprietary infant foods, such as Mellin’s Food, Eskay’s Food, Racahout. These foods may require the addition of Taka diastase to make them more readily digested. They leave the stomach more rapidly than any of the others, and for this reason will be found to give less discomfort than the foods containing a high percentage of protein and fat. This diet, however, cannot be prolonged on account of its lack of balance. If the gruels are made with milk instead of with all water they become more evenly balanced. Samples of the stomach contents may be taken for analyses from time to time.
Lavage.—When lavage is necessary the patient must be allowed to rest after the process before being given food, otherwise it is apt to be vomited.
Instructions to Nurse.—The treatment for gastric ulceration is thus seen to be strenuous. In the beginning the patient is placed on a liquid or semi-solid diet, or is not fed at all for a time. This is done that the diseased organ may have a chance to adjust itself as far as possible and to give the physician an opportunity of studying the changes taking place in that organ. During the course of the [Pg 256] disease the general symptoms which develop from time to time, causing more or less pain and discomfort to the patient, are nervousness, which in some individuals amounts to melancholia, extreme anemia and an utter distaste for food, all of which require patience on the part of the physician, the nurse, and the patient herself to overcome. The nurse must see that the patient is not disturbed or made unhappy by having business or home cares talked over in her presence; she must be kept as cheerful and as comfortable as her condition permits and urged to use care in her diet. After the ulcer is healed, to prevent a return of the trouble she must be warned against eating too fast or when over-tired, and she must be advised against very hot and highly seasoned foods, for, in the observance of these simple common-sense precautions only is she even in a measure saved further attacks.
Special Diets Used for Gastric and Duodenal Ulcer.—There are several well-known diets used in these conditions. Among those that have been found most satisfactory may be mentioned the Sippi diet, the Lenhartz diet.
All of these diets require the most careful adjustment as to regulation of intervals of feeding, type of food material used, and method of preparation and administration of food.
The treatment is directed toward the reduction of the free hydrochloric acid in the stomach in order that the ulcer may have an opportunity for healing.
Sippi Diet.—Equal quantities of heavy cream and whole milk, beginning with ½ ounce each every hour during the day. Alkaline powders are given with the meal and one-half hour after the meal. These consist of 15 grains each of sodium bicarbonate and bismuth subcarbonate with the feeding, and 10 grains of light oxide of magnesia and 15 grains of sodium bicarbonate between [Pg 257] feeding. The cream and milk are increased at the rate of one-half ounce each at each feeding for two days, the powders are continued as on the first day. On the fourth day an egg is added to the diet, the milk and cream are given in quantities of one and one-half ounce each, every hour. On the fifth day two eggs are added. On the sixth day one helping of oatmeal or other soft cereal is added to the above diet. The diet is in this way increased until the patient is taking three eggs and nine ounces of cooked cereal each day in addition to the cream and milk mixture. The amount given at one time must be small, never exceeding six ounces (according to Carter, Howe and Mason).
An accurate control of the acidity of the stomach should be maintained, this is accomplished by withdrawing a certain amount of the gastric contents by means of the stomach tube.
The Lenhartz Diet.—This diet is likewise given in hourly feedings, consisting of milk and raw eggs in the beginning, then a small portion of sugar is added, next scraped beef is added to the milk, eggs and sugar, already given, then boiled rice. Next a small quantity of zwieback (or soft toast), and continuing in this way, chicken, and butter are admitted. In the beginning the quantity of milk is 100 c.c. and the number of eggs 2, given raw. It is served iced, and with a teaspoon. When the sugar is added it is beaten up with the eggs (20 gm.). The milk and eggs are divided into separate feedings and given at hourly intervals from 7 A.M. to 7 P.M. It is rarely possible to give the amounts called for in the Lenhartz diet after the sixth day, but as much as possible should be given without risking an acute disturbance. Women, as a rule, find it more difficult to take the full amount ordered than men.
The following outlines represent the diet for the first, third, sixth, seventh and tenth day:
FIRST DAY
| 7 A.M. | Egg |
| 8 A.M. | Milk, 20 c.c. |
| 9 A.M. | Egg |
| 10 A.M. | Milk, 20 c.c. |
| 11 A.M. | Egg |
| 12 noon | Milk, 15 c.c. |
| 1 P.M. | Egg |
| 2 P.M. | Milk, 15 c.c. |
| 3 P.M. | Egg |
| 4 P.M. | Milk, 15 c.c. |
| 5 P.M. | Egg |
| 6 P.M. | Milk, 15 c.c. |
| Total: Milk, 100 c.c. Eggs (raw), 2. |
THIRD DAY
| 7 A.M. | Egg; sugar, 2 gm. |
| 8 A.M. | Milk, 50 c.c. |
| 9 A.M. | Egg; sugar, 3 gm. |
| 10 A.M. | Milk, 50 c.c. |
| 11 A.M. | Egg; sugar, 3 gm. |
| 12 noon | Milk, 50 c.c. |
| 1 P.M. | Egg; sugar, 3 gm. |
| 2 P.M. | Milk, 50 c.c. |
| 3 P.M. | Egg; sugar, 3 gm. |
| 4 P.M. | Milk, 50 c.c. |
| 5 P.M. | Egg; sugar, 3 gm. |
| 6 P.M. | Milk, 50 c.c. |
| 7 P.M. | Egg; sugar, 3 gm. |
| Total: Milk, 300 c.c. Eggs (raw), 4. Sugar, 20 gm. |
SIXTH DAY
| 7 A.M. | Egg; sugar, 4 gm. |
| 8 A.M. | Milk, 100 c.c. |
| 9 A.M. | Egg; sugar, 4½ gm.; scraped beef, 12 gm. |
| 10 A.M. | Milk, 100 c.c. |
| 11 A.M. | Egg; sugar, 4½ gm. |
| 12 noon | Milk, 100 c.c. |
| 1 P.M. | Egg; sugar, 4½ gm.; scraped beef, 12 gm. |
| 2 P.M. | Milk, 100 c.c. |
| 3 P.M. | Egg; sugar, 4½ gm. |
| 4 P.M. | Milk, 100 c.c. |
| 5 P.M. | Egg; sugar, 4 gm.; scraped beef, 12 gm. |
| 6 P.M. | Milk, 100 c.c. |
| 7 P.M. | Egg; sugar, 4½ gm. |
| Total: Eggs (raw), 7. Milk, 600 c.c. Sugar, 30 gm. Scraped beef, 36 gm. |
SEVENTH DAY
| 7 A.M. | 1 soft-cooked egg |
| 8 A.M. | Milk, 100 c.c. |
| 9 A.M. | Egg; sugar, 13 gm. |
| 10 A.M. | Milk, 100 c.c.; scraped beef, 23 gm.; boiled rice, 33 gm. |
| 11 A.M. | 1 soft-cooked egg |
| 12 noon | Milk, 125 c.c. |
| 1 P.M. | Egg; sugar, 13 gm. |
| 2 P.M. | Milk, 125 c.c.; scraped beef, 23 gm.; boiled rice, 33 gm. |
| 3 P.M. | 1 soft-cooked egg |
| 4 P.M. | Milk, 125 c.c. |
| 5 P.M. | Egg; sugar, 14 gm. |
| 6 P.M. | Milk, 125 c.c.; scraped beef, 24 gm.; boiled rice, 34 gm. |
| 7 P.M. | 1 soft-cooked egg |
| Total: Eggs (raw), 4; (soft-cooked), 4. Milk, 700 c.c. Sugar, 40 gm. Scraped beef, 70 gm. Boiled rice, 100 gm. |
TENTH DAY
| 7 A.M. | 1 soft-cooked egg |
| 8 A.M. | Milk, 166 c.c. |
| 9 A.M. | Egg; sugar, 13 gm. |
| 10 A.M. | Milk, 168 c.c.; scraped beef, 23 gm.; boiled rice, 66 gm.; butter, 4 gm. |
| 11 A.M. | 1 soft-cooked egg; zwieback (or soft toast), 20 gm.; butter, 4 gm. |
| 12 noon | Milk, 166 c.c.; minced chicken, 25 gm. |
| 1 P.M. | Egg; sugar, 13 gm. |
| 2 P.M. | Milk, 166 c.c.; scraped beef, 25 gm.; boiled rice, 66 gm.; butter, 4 gm. |
| 3 P.M. | 1 soft-cooked egg; butter, 4 gm.; toast or zwieback, 20 gm. |
| 4 P.M. | Milk, 168 c.c.; minced chicken, 25 gm. |
| 5 P.M. | Egg; sugar, 14 gm. |
| 6 P.M. | Milk, 166 c.c.; scraped beef, 24 gm.; boiled rice, 67 gm.; butter, 4 gm. |
| 7 P.M. | 1 soft-cooked egg |
| Total: Eggs (raw), 4; (soft-cooked), 4. Milk, 1000 c.c. Sugar, 40 gm. Scraped beef, 70 gm. Minced chicken, 50 gm. Butter, 20 gm. Boiled rice, 200 gm. Toast or zwieback, 40 gm. |
As a rule the seat of the gastric cancer is the pylorus. The patient gives evidence of chronic gastritis with continued pain, localized tenderness, vomiting of partially digested food and at times dilatation from extreme fermentation. The hemorrhages are as a rule not large, the blood having changed to a brownish color resembling coffee grounds. Vomiting, in cases where the pylorus is involved, generally occurs several hours after eating, the vomitus being in an advanced state of fermentation. Upon analysis of the stomach contents there is found to be a lack of free HCl.
Dietetic Treatment.—In the dietetic treatment of cancer of the stomach the most digestible forms of foods must be given, milk forming in this, as in other gastric disorders, the chief article of diet. As too much food cannot be tolerated, the meals must be small, even if given more frequently. The patient is often found to evince a distaste for meat, in which case fish may be substituted. When meat is given, it must be simple in form and preparation, such as boiled or broiled sweetbreads or brains, scraped beef or stewed chicken. Rice, farina, cornmeal mush, and other fine cereals, cooked with or without milk, are valuable additions to the diet. Well-cooked and strained spinach, green peas, cauliflower, carrots, and tender string beans and boiled or baked potatoes well mashed may be recommended. Tea, coffee, or cocoa may be used to flavor the milk. These must be given in small portions. The following diet list is recommended by Friedenwald and Ruhräh:
| Calories | ||
| 8 A.M. | 100 grams of milk with tea | 100.0 |
| 30 grams of milk toast | 130.0 | |
| 10 A.M. | 100 grams of baked trout | 106.0 |
| 100 grams of milk or 30 grams panopepton (57.5) | 67.0 | |
| [Pg 261] | 10 grams of butter | 81.0 |
| 50 grams of toast | 130.0 | |
| 50 grams of sherry | 60.0 | |
| 12 M. | Bouillon with 5 grams somatose | 16.0 |
| 100 grams of chicken | 106.0 | |
| or 100 grams squab (100) | ||
| or 100 grams of calves’ sweetbreads (90) | ||
| or 100 grams of calves’ brains (140) | ||
| 60 grams of macaroni | 212.0 | |
| or 100 grams of mashed potatoes (127) | ||
| or 100 grams of spinach (166) | ||
| or 100 grams of asparagus (18) | ||
| 25 grams of stale wheat bread | 65.0 | |
| 4 P.M. | 20 grams of toast | 130.0 |
| 20 grams of butter | 162.0 | |
| 40 grams of caviar | 52.0 | |
| 7 P.M. | 130 grams of milk (100) with 5 grams somatose (16) | 116.0 |
| 100 grams of rice cooked in milk | 177.0 | |
| 50 grams of wheat bread | 130.0 | |
| 9 P.M. | 30 grams of panopepton | 57.5 |
| 2024.5 |
1. Errors in Diet.—Over-feeding, under-feeding, improper food, unbalanced diet.
2. Disturbed Secretory Processes.—
(a) Over- or under-secretion of gastric juice.
(b) An excess or deficiency of hydrochloric acid in the
juices.
3. Impaired Motility and Tone of the Gastric Organ.—The peristaltic waves and muscular contraction of the [Pg 262] stomach walls becoming sluggish prevent the food mass from passing into the intestines at a normal rate of speed, thus giving rise to a fermentation of the food and a consequent dilatation of the organ from the gas thus produced.
Other Factors.—Lack of fresh air and exercise, indoor occupation, bad hygiene, unsanitary surroundings, heredity, certain diseases which are accompanied by gastric disorders.
Diseases of Gastric Organ.—Acute and Chronic Gastritis, Gastric-Ulceration, Gastric Cancer.
Treatment.—Tests—Test meals, X-Ray examinations (pictures and Fluoroscope). Patient is given no breakfast on day of test. In X-Ray laboratory a bismuth or barium meal is given, this meal consists of a pint of fluid, either buttermilk or malted milk, into which a certain amount of bismuth or barium chloride is mixed.
Starvation Period.—A period of abstinence from food is instituted in most of the gastric disorders, (a) to determine the extent and character of the disease, (b) to rest the digestive tract.
Dietetic Treatment.—Diet adjusted to meet the needs of the individual case as determined by the medical examination.
Instruction to Patient.—Individual warned against overeating, drinking and constipation.
(a) Formulate a diet order for a patient suffering from chronic gastritis. (Individual’s food requirements must be observed.)
(b) Formulate a diet for gastric ulceration. List the available foods; the avoidable foods.
(c) Outline a diet to be used in case of gastric cancer; show how it differs from the one used in gastric ulceration.
[92] It is also customary to give the patient a bismuth or barium meal in order that an X-ray and fluoroscopic examination may be made to determine the character and extent of the disturbance.
[93] “Diseases of the Stomach,” by Boas.
Diarrhea, like gastritis, may be a symptom of many diseases and a result of many digestional disturbances. Enteritis, enterocolitis, dysentery, typhoid fever, and certain cases of tuberculosis and syphilis are all accompanied by an inflamed condition of the mucous lining of the intestinal walls, and in each of these pathological conditions we may find diarrhea as a resulting symptom.
Causes.—Diarrhea may be acute or chronic in character. It may be brought on by errors in diet, warm weather, certain drugs, ptomaines, bad hygiene, polluted water or milk, and by overeating. Idiosyncrasies against certain kinds of food have been found in both adults and children; these idiosyncrasies are manifested by pain and diarrhea whenever the offending foods have been eaten. Acute diarrhea has also been brought on in children by the drinking of cold lemonade when over-heated.
Diarrhea in Children.—All diarrheas in children, and especially those developing during the hot months, must be looked on with suspicion and given immediate attention before they have an opportunity to develop serious features which may terminate in death before the seriousness of the condition is realized.
As a rule, almost any diarrhea in children will raise the temperature. This does not occur so often with adults unless the diarrhea results from infectious fevers, ptomaines, [Pg 264] etc., in which case it may rise suddenly and to a considerable height.
The Bowels.—The symptoms of this condition are too liquid or too frequent stools, the number varying from three to twelve or more a day. They may be greenish yellow in color and contain particles of undigested food and mucus. In prolonged diarrheal attacks the stools sometimes contain blood.
The attack may be accompanied by more or less pain of a colicky nature, due to the formation of gas in the intestinal tract. In ptomaine poisoning this pain is sometimes very intense. As a rule the intestinal tract is emptied by means of salt, oil, etc., but this is generally directed by the physician. A soapsuds or salts and glycerin enema to flush the colon will often give quick relief by dispelling the gas.
Starvation.—The entire digestive tract requires absolute rest for a certain period; no food and very little water, the latter in the form of bits of ice only, are given for a period lasting from twelve to thirty-six hours or more, depending upon the violence of the attack and the condition of the patient. This is to allow the toxic substances which are probably causing the disturbance to pass out of the body, either in the feces or in the urine. When the acute symptoms subside, that is, when the pain and distention of the intestines have disappeared, and the bowel movements become more normal in number and character, the dietetic treatment suitable to the condition is instituted.
Dietetic Treatment.—The first day the patient is given a small cup of weak tea, half a glass of buttermilk or peptonized milk, or a cup of well-skimmed meat broth, every three or four hours. If the patient is weak, the nourishment may be given oftener, and in those cases it is often [Pg 265] found advisable to give a small amount of alcohol in the form of brandy in albumen water, or panopepton or liquid peptonoids. These may be administered in tablespoonful doses every two hours. Whole milk, unless it is peptonized, and at times even then, is not advisable in diarrheal conditions on account of its liability to form curds which decompose with the production of toxic substances, known to be exceedingly irritating to the already inflamed mucous membranes lining the intestinal walls.
Increasing the Diet.—As the diarrhea and inflammation subside, the following foods are gradually introduced into the dietary, keeping in mind always that a return of the acute symptoms is apt to occur. Hence the patient must never be overfed. It is better to err on the side of too little than too much food during the early convalescent period.
Diet.—Soft-cooked eggs, toast (slightly buttered), cocoa made with water instead of milk, chicken, calf’s-foot or wine jelly; later, well-cooked rice, junket, and soft custard; still later, lightly broiled beefsteak, lamb chops, chicken, squab or quail, sweetbreads or brains. Not until the patient is entirely free from all symptoms of diarrhea or intestinal disturbance may the following foods be given: cream or cream dishes such as cream toast, cream chicken, or cream soup, raw or stewed fruit, green vegetables, salt foods, spiced foods of any description; pastries, confectionery and desserts in general, unless they are simple in character and are sweetened with saccharin instead of sugar, as the latter substance is particularly susceptible to fermentation.
Anemia as a Result.—Anemia is one of the most common results of prolonged diarrheal attacks, especially in those toxic diarrheas resulting from infectious diseases, dysentery, etc. The blood-making tissues suffer from a lack [Pg 266] of nourishment and are in consequence incapable of producing blood of the best quality. Hence the starvation treatment cannot be carried on over a very extended period or the resulting anemia may be more difficult to overcome than the original trouble.
Selecting and Regulating the Diet.—The following points must be kept in view when regulating the diets of individuals who are prone to develop diarrhea:
Preparing the Diet.—Only such foods as are known to agree with the individual, and these prepared in the simplest manner possible, must have a place in the dietary.
Fermentation.—All foods that are subject to fermentation either in the stomach or intestines must be withheld, at least until the attack is well over. Sugar is an example of such foods; saccharin may be substituted when necessary.
Avoidable Foods.—Pork, veal, and shellfish must be left out of the dietary, possibly for months, since they have been found frequently not only to bring about a return attack of diarrhea but also to have been the cause of the original one.
Fatty foods of all sorts had best be avoided as long as there are symptoms of diarrhea; these foods are handled with difficulty by the digestive apparatus and impose extra work upon the intestine, which is already taxed by the disease.
Restricting Fluids.—Fluid foods should be more or less limited in the diet, since they require more effort on the part of the intestines than the more concentrated foods.
Proprietary Foods.—Certain proprietary infant foods[94] are at times found to be exceedingly valuable, since they furnish food in a concentrated and digestible form. Among these Mellin’s Food, Racahout, and Imperial Granum may be mentioned.
The Stools.—When the diarrhea is chronic in character, the character of the stools indicates the seat of the inflammation. When there is a great deal of undigested food found in them the upper part of the bowel is more affected; when the stools contain more mucus than food the lower bowel is the chief seat of the trouble. The frequency and fluidity of the stools impose a great strain upon the entire body, causing a progressive emaciation and anemia.
The treatment is similar to that instituted in acute attacks. The starvation régime cannot be carried out for a long period. Efforts must be made to ascertain the cause of the trouble and to overcome it. This is, as a rule, more easily accomplished with adults than with infants and children.
Dietetic Treatment.—The diet is the chief point of observation and attention. The same care must be observed as is found necessary in the after-treatment of acute diarrhea. The patient must be cautioned not to eat indigestible foods or those which are known to cause trouble in this respect. She must be warned against eating when over-tired.
Enterocolitis is an inflammation of the lower intestines and colon. The stools contain more mucus than those occurring when the inflammation is higher up in the intestines and blood is also more frequent in these stools. The prostration is more marked and the fever apt to be higher than in ordinary diarrheal attacks. However, acute attacks of enterocolitis do not produce the marked anemia or the emaciation which are so common in the chronic cases of enteritis.
[Pg 268] Dietetic treatment the same as that used in acute diarrhea.
Dysentery is a disease in which the seat of inflammation is the colon. The bowels are distended and tender, the pain at times is acute and spasmodic, and the fever moderate. The constant desire to defecate and the straining which accompanies each effort, as well as the small stools, containing both blood and mucus, furnish the characteristic symptoms of this disease. Rest in bed is absolutely necessary; the patient must be induced to use a bedpan.
Dietetic Treatment.—The diet consists entirely of liquids as in acute diarrhea, the same careful régime being observed as in those conditions. The soreness in the abdomen is at times relieved by spice poultices or a hot turpentine stupe.
When the above conditions become chronic, the patient loses weight and strength rapidly, becomes anemic and emaciated. The treatment, like that used in the acute disease, consists of rest and liquid diet. The medicinal treatment is left entirely in the hands of the physician.
Appendicitis is an inflammation of the vermiform appendix. It may be acute or chronic in form.
Symptoms.—The disease is manifested by sudden pain in the right side, tenderness over the seat of the inflammation, and a localized rigidity of the right iliac fossa. The attack is as a rule accompanied by fever which may run as high as 103° or 104° F. The patient may suffer from nausea and vomiting. Constipation is generally an annoying symptom of the disease.
Rest in Bed.—The treatment of the acute attack consists of total abstinence from food for twelve or more hours [Pg 269] until the most acute stage has passed and the patient either passes into the hands of the surgeon or the symptoms begin to subside in violence. It is necessary that the patient be kept in bed, not being allowed to rise for anything. The nurse must make him understand that his recovery, possibly his very life, depends upon his absolute quiet during the early stages of the disease.
Dietetic Treatment.—When the first acute symptoms have passed, the diet must consist of fluids, well-skimmed meat broths, buttermilk, peptonized milk, albumen water or albumenized orange juice. No solid food must be given until the acute symptoms have disappeared. When the tenderness in the right side has entirely left him and he no longer suffers the pain or nausea, a gradual return to a normal diet may be made. The patient must be cautioned against eating indigestible foods, as an attack of intestinal indigestion may readily start up an irritation in the susceptible appendix and cause a second attack of appendicitis which is often of a more serious nature than the first.
Convalescent Diet.—The return to solid food is made gradually as in other intestinal disorders, by giving the most digestible foods first. Soft toast, soft eggs, fine cereal gruels, well-cooked rice, well-baked white potatoes, meat, wine or fruit jellies; then lightly broiled beefsteak, lamb chop, chicken, sweetbreads, or brains given in small quantities until the intestinal tract has regained its vigor.
Foods to Be Avoided.—Highly seasoned foods must be avoided on account of their astringent qualities, which may cause constipation. Long, tough-fibered meats, coarse vegetables, rich foods, in fact anything which may cause intestinal indigestion, must be eliminated from the dietary. A decomposition of the foods lying in the lower part of the small intestine is dangerous to such individuals, since such products are highly toxic in character and exceedingly irritating to the already tender appendix.
Chronic constipation is so universal a condition that it must be treated and overcome whenever it is possible. This condition is not only the cause but the result of disease. It may be induced by improper food, poor hygiene, sedentary habits, lack of exercise, the taking of drug preparations such as cough sirups which contain opium in some form, the constant taking of cathartics and enemas, or it may be an hereditary condition.
Diet, Exercise, and Fresh Air.—The chief means of overcoming this deplorable chronic condition is by regulating the diet and increasing the amount of exercise in the fresh air.
At times it is necessary to resort to artificial stimulation of the intestinal movements; at others, on account of the disease of which it is only one of the symptoms, it is dangerous to irritate the already inflamed mucous membranes lining the intestinal wall. In these cases the physician prescribes the method of procedure. In ordinary cases, however, the following suggestions may be used as a guide in overcoming the condition.
Available Foods.—It must be borne in mind that the food must not be too concentrated in character or it will be so completely absorbed as to leave little or no residue for the feces, and since the waste products of metabolism, both of food and body materials, must be eliminated, a certain amount of fecal matter is necessary to assist in this work. Vegetables, such as celery, turnips, lettuce, asparagus, string beans, spinach, and beans, lentils, lima beans, and onions; fruits, such as raisins, figs, and prunes; and cereals which have not had all the bran removed, such as cut oats, cracked wheat, etc., on account of the cellulose they contain, act admirably in overcoming chronic constipation. It is found, however, that when even these are not sufficient in certain [Pg 271] cases, bran added to the food, either alone, with the breakfast cereal, or in the form of biscuits, muffins, or cookies, will give just the necessary amount of ballast to the food mass to make it stimulate the peristaltic movements by its pressure upon the intestinal walls.
Stimuli to Peristalsis.—Foods yielding certain acids exert a stimulating action upon intestinal peristalsis.
Available Foods.—Those particularly valuable for this purpose are limes, oranges, apples, prunes, figs, raisins, and most fruit juices (with the exception of blackberries, which are constipating), tomatoes, and rhubarb. The fruit juices may be diluted with water or carbonated water (in the latter case the action is increased because of the gas contained in the water), and taken the first thing in the morning, or the fruit may be eaten at night before retiring, and in the morning on an empty stomach. Prune pulp or prune jelly may be given to children as well as to adults. The action of this fruit is augmented by the addition of senna leaves. A conserve made of prunes, figs, and raisins given in teaspoonful doses at night and before breakfast often gives splendid results in curing chronic constipation.
Gas-forming Foods.—The eating of foods which give rise to a slight formation of gas owing to their tendency to ferment likewise acts as a stimulus to intestinal movements. Among these may be mentioned honey, molasses, cauliflower, cabbage, spinach, and onions. If the honey and molasses are poured on bran muffins or biscuits, on breakfast food, or added as sweetening agents to cookies, they will be found particularly valuable. Care must be taken, however, not to give too much of either of these foods or they will disturb the digestion and do more harm than good.
Use of Salt Foods.—Foods such as herring, caviar, anchovies, ham, etc., on account of the salt they contain, exert a stimulating effect upon the movements in the small and large intestines. Graham bread, spread with brown [Pg 272] sugar, molasses, or honey, makes an acceptable addition to the meal of the majority of children and to that of many adults.
Fats and Mineral Oils.—The use of fats is often recommended; olive oil may be given in tablespoonful doses before breakfast and at night or it may be served on vegetables and salads. If one or two tablespoonfuls are taken at night and before breakfast, it may act as a laxative. In many cases, however, this oil is completely absorbed in the small intestine and hence there is none left to lubricate the passage for the food mass. When vegetable oils do not prove satisfactory, mineral oils may be substituted. These oils have absolutely no fuel value and are not digested in the intestinal canal but mix with the fecal mass, softening it and stimulating its passage through the large intestine. There are certain individuals with whom the mineral oils do not act as lubricants and instead of softening the feces and lubricating the passage will slip through the intestinal canal without carrying the feces along.
Sample Diet Sheets.—The following menus are suggested for the use of individuals suffering with chronic constipation:
Breakfast
| 7 A.M. | Orange juice and water. |
| 8 A.M. | 1 bran muffin with honey and cream. |
| 1 or 2 slices of bacon. | |
| Whole wheat biscuits. | |
| A cup of coffee, cereal coffee, or hot milk (not boiled). |
Luncheon
| 1 P.M. | Casserole of beef made with lean beef. |
| Turnips and potatoes. | |
| Graham bread or muffins and honey or preserves. | |
| Milk or “hot water” tea. |
Dinner
| Tomato bouillon. | |
| Roast lamb. | |
| String beans. | |
| Potatoes baked with jackets on. | |
| Celery salad, dressed with plenty of oil and lemon juice. | |
| Prune jelly with whipped cream. |
Breakfast
| Prunes and figs cooked together. | |
| Slice of ham with 1 soft-cooked, poached, or scrambled egg. | |
| Whole wheat or bran biscuits. | |
| Coffee with cream and sugar. |
Luncheon
| Vegetable soup. | |
| Pork and beans. | |
| Boston brown bread. | |
| Baked apple (skin eaten). | |
| Oatmeal wafers. |
Dinner
| Roast beef. | |
| Spinach or cauliflower served with butter sauce. | |
| Cold slaw. | |
| Pineapple jelly (pineapple left in), whipped cream, | |
| or | |
| Date and fig pudding. |
Auto-intoxication is a condition produced by the absorption of the decomposition products of food in the intestinal canal.
[Pg 274] Absorption of Toxins.—As a rule the condition occurs in individuals suffering more or less from constipation which may be due to errors in diet or a lack of tone in the intestines, giving rise to a sluggishness in the peristaltic movements in this region of the alimentary canal. In certain individuals the liver is more or less sluggish, or in some way fails to do its regular work of detoxifying the products of metabolism brought in by the blood stream, in which case these toxins are reabsorbed into the system and induce a condition known as auto-intoxication.
Care of Bowels.—As a rule the patient has more or less fever, nausea and at times vomiting. The head aches and the abdomen may be distended by the formation of gas in the intestines. The treatment is like that used in the majority of intestinal disorders. The bowels are emptied by means of soapsuds or salts and glycerin enemas. Certain physicians recommend an enema made with equal quantities of milk and molasses, with enough hot water added to make a thin, warm solution. Care must be used in preparing this flatus enema on account of the danger of curdling the milk with the acid in the molasses and the hot water. If the solution should curdle it must be discarded and a fresh solution prepared. A flatus enema containing salts, glycerin, and a few drops of turpentine is also valuable in removing the gas formed by the action of the putrefactive bacteria upon the unabsorbed food mass. This enema must be given “high” so as to reach the spot in the colon where it may efficiently do its work.
Dietetic Treatment.—The diet may consist of fluids for the first few days, or as long as the fever continues. Buttermilk is probably the best fluid food to use under such conditions, since it not only nourishes, but likewise furnishes lactic acid bacteria which aid in the destruction of the more harmful bacteria, especially numerous under the conditions just mentioned. When whole milk is given it is best [Pg 275] to peptonize it. Well-strained meat broths may be given occasionally to vary the diet and albumenized orange juice or orange juice in carbonated water may also be given once or twice daily during the febrile period. After this, the patient may have well-cooked cereal gruels. These may be dextrinized with vegetable diastase (Taka diastase) if necessary. A return to normal diet is made gradually to prevent a return of the trouble. The patient should be advised against overeating, and eating highly seasoned or indigestible foods.
Convalescent Diet.—The diets recommended for use during convalescence from other intestinal disorders may serve here, reducing, however, the allowance of meat, since meat proteins are particularly susceptible to attacks of putrefactive bacteria.
Dietary Precautions.—After the body has returned to its normal state, the patient must keep in mind the danger arising from constipation and intestinal putrefaction. The following menu is given as a guide to aid the individual in selecting a diet which will in a measure assist in preventing future attacks of intestinal putrefaction and auto-intoxication:
| 7 A.M. | 1 glass of water with orange or lime juice. |
| Breakfast | |
| 8 A.M. | Stewed prunes or figs. |
| Cereal and cream. | |
| Buttered toast. | |
| Crisp bacon. | |
| Coffee. | |
| Luncheon | |
| Vegetable or tomato soup. | |
| Green vegetables such as cauliflower, greens, or tomatoes; or | |
| [Pg 276] | Baked dishes such as macaroni and cheese, scalloped macaroni and tomatoes; or |
| Baked potatoes, or potatoes au gratin, or stuffed tomatoes with rice. | |
| Stewed fruit or fruit jelly. | |
| Sponge cake with simple sauce. | |
| Junket. | |
| Toasted crackers or bread. | |
| Dinner | |
| Milk soup. | |
| Cream of spinach, celery, peas, or tomatoes. | |
| Baked eggs, cheese soufflé or nut loaf. | |
| Tender green peas, cauliflower, spinach, boiled or creamed potatoes, well-boiled rice. | |
| Fruit, vegetable, tomato, or cheese salad. | |
| Simple dessert, such as cottage pudding with simple sauce, fruit pudding, prune whip, or frozen desserts; ice cream or water ices; or | |
| Cheese and crackers. | |
| Coffee. | |
Character.—Acute or chronic, accompanying many pathological conditions, especially in children in whom diarrhea in any form must be given immediate attention.
Causes.—Errors in diet, polluted water or milk, ptomaines, bad hygiene, and certain drugs.
Bowels.—The stools vary in number from three to twelve a day. They may be greenish yellow in color, containing mucus and particles of undigested food and, in prolonged cases, blood.
Treatment.—Rest in bed and total abstinence from food for from twenty-four to forty-eight hours. Salines are [Pg 277] usually given by mouth or by rectum, but this is left to the discretion of the physician. Very little water is given by mouth during the period of total abstinence. Thirst is relieved by bits of ice, and enemas are given if necessary.
Administration of Diet.—When acute symptoms have disappeared and the stools are becoming more normal in character and number, a fluid diet of from four to six ounces is administered every three or four hours or oftener if patient is very weak. Brandy may likewise be given in cases in which exhaustion is marked.
Dietetic Treatment.—Concentrated foods of the simplest character and only those known to agree. Proprietary infant or invalid foods, except malted foods, which exert a laxative effect; among those found to be good may be mentioned Mellin’s Food, Imperial Granum, and Racahout.
Foods to Be Avoided.—Fatty foods; pork, veal, and shellfish; all foods that are subject to fermentation in the stomach or intestinal tract (sugar).
Foods to Be Limited.—Fluids, soup, beverages, etc., because they impose more work on the intestines.
Seat of Inflammation.—Lower intestine and colon.
Differentiating Characteristics.—More mucus and blood in stools; greater prostration; greater rise of temperature; and less anemia than in chronic enteritis.
Dietetic Treatment.—Practically the same as in other diarrheas.
Characteristic Symptoms.—Acute and spasmodic pain, tenderness and distention in the bowels, moderate fever, straining and a constant desire to defecate, small stools containing blood and mucus, loss of weight and marked anemia when condition becomes chronic.
[Pg 278] Treatment.—Rest in bed absolutely necessary; the use of the bedpan made obligatory; soreness relieved by hot turpentine stupes or spice poultices.
Dietetic Treatment.—No food for a period of from thirty-six to forty-eight hours, after which fluids and the régime recommended in acute diarrhea are advisable. In chronic dysentery the diet is practically the same. The extreme exhaustion and anemia accompanying these conditions make it necessary to increase the diet carefully but soon to offset as far as possible the devastating effects of the disease.
Treatment.—Confinement to bed is absolutely necessary while acute symptoms prevail. The life of the patient may depend upon the care with which this “quiet” period is carried out. No food should be given for twelve or more hours to enable the physician to make a proper diagnosis and to allow the intestinal tract and appendix complete rest from the irritating effects of food passing down the canal.
Dietetic Treatment.—Acute Stage: Total abstinence for a period, after which fluids as given in other acute intestinal disorders. No solid food until acute symptoms have subsided; then a gradual return to normal.
Convalescence.—When tenderness in right side has disappeared, the return to a normal diet is made gradually. Gelatin, soft eggs, soft toast, fine cereal gruels, well-cooked rice, well-baked white potatoes, tender rare beefsteak or lamb chops, the breast of chicken, sweetbreads, and brains are recommended.
Relapse or Recurring Appendicitis.—The patient must be warned against eating indigestible foods or any kind of foods liable to cause constipation; also against overeating or eating when over-heated or over-tired. One attack predisposes to another, hence the above precautions are necessary to prevent the condition from becoming chronic.
Causes.—Improper foods, indoor occupations leading to a lack of fresh air and exercise, bad hygiene, certain drugs, such as cough sirups, etc., containing opium in some form, constant use of cathartics and enemas to move the bowels, heredity.
Dietetic Treatment: Foods to Be Avoided.—Highly spiced foods must be avoided on account of their astringent qualities, too concentrated foods because they fail to furnish the necessary bulk without which the waste matter cannot pass out of the body at a sufficient rate of speed to prevent putrefaction taking place in the intestinal tract.
Foods Stimulating Peristalsis on account of their bulk: Bulky foods, such as vegetables, cabbage, turnips, cucumbers, spinach, beans, celery, lettuce, etc.; cereal foods containing a high percentage of bran, bran bread and cookies, fruits such as raisins, prunes, figs.
Foods Acting as Stimuli to Intestinal Movements on account of their acid content: Limes, oranges, apples, prunes, figs, raisins, most fruit juices (blackberries excepted), rhubarb, tomatoes, cauliflower, spinach, onions, honey, and molasses; senna leaves likewise have a distinct action upon the peristaltic movement of the intestines, hence are included here.
Precautions.—Emphasis should be placed upon the dangers of (1) overeating any of the foods indicated in the above list and thus bringing about conditions more dangerous in result than the original disturbance; (2) the taking of drugs to move bowels on account of the ease with which the habit is acquired and the consequent inability of the bowels to move without such whips; (3) the taking of too little water, thereby allowing a too concentrated condition of the food mass and a consequent accumulation of substances which inhibit peristaltic action.
[Pg 280] Use of Fats and Mineral Oils.—Olive and other vegetable oils, if not completely absorbed, are advised on account of their lubricating effects. The same can be said of the mineral oils which have no food value but in many cases furnish the lubricant necessary in certain individuals suffering from sluggish intestinal peristalsis.
(a) List the food used in the treatment of enterocolitis; outline the method of administering the diet.
(b) Formulate a convalescent diet for diarrheal cases.
(c) List the foods used in chronic constipation; list the avoidable ones.
[94] Malted foods are contraindicated, as malt exerts a very laxative effect.
Fever is an abnormal condition characterized by an elevation of body temperature, quickened respiration and circulation, and a certain amount of tissue waste. This elevation of temperature may be due to various conditions, such as local inflammation, infectious diseases, disturbed metabolism and food poisoning (ptomaine).
Tissue Waste in Fevers.—Fevers of short duration, such as accompany colds, tonsillitis, chicken pox and intermittent fever, remittent fever, and at times malarial fever, do not cause sufficient tissue waste to make the nutrition the important feature of the treatment. In ptomaine poisoning the tissue waste may be great, but it is the result of the poisoning, as is the fever, so that the diet needs to be adjusted only after the disturbance has abated. In the beginning, starvation is instituted and the fever disappears when the poisoning is controlled.
Treatment of Fevers of Short Duration.—In all fevers of short duration then, the treatment is directed with the following points in mind: (1) relieving the cause, (2) preventing gastro-intestinal disturbances, (3) saving the heart, kidneys, etc., extra strain.
Dietetic Treatment.—In doing this the diet is so formulated as to meet the above-mentioned conditions, and fluids seem the best form in which food can be given to bring about the desired results. The quantity of fluids should be small and the intervals between feedings short. Two-hour intervals seem best in the beginning. These intervals are lengthened as the fever decreases and the [Pg 282] amount of food at each feeding increased. When convalescence is established, semi-solid, soft or convalescent diet may replace the fluids and the patient gradually brought back to a normal diet.
Fluid Diet.—The following foods constitute a fluid diet: milk, whole milk, plain, peptonized, or albumenized, buttermilk, koumiss, malted milk, milk shake, milk punch, cream, whey; fruit beverages, plain, albumenized, or mixed with whole raw egg; eggnog, milk and ginger ale, cocoa, strained gruels, broths reënforced with egg or plain. Carbonated water may be added to milk or fruit beverages.
Schedule of Feeding.—The following schedule may be used as a guide in fevers of short duration:[95]
I
| 7 A.M. | 6 oz. hot milk or cocoa. |
| 9 A.M. | 6 oz. broth reënforced with egg. |
| 11 A.M. | Milk shake. |
| 1 P.M. | Oatmeal gruel, 4 oz.; 2 oz. cream. |
| 3 P.M. | Albumenized orange juice, 4 oz.; 1 egg white. |
| 5 P.M. | 6 oz. broth reënforced with egg white. |
| 7 P.M. | 6 oz. cocoa. |
| 9 P.M. | 6 oz. malted milk. |
| 12 M. and 4 A.M. | 4 oz. hot milk and 2 oz. cream. |
The above furnishes approximately 750 calories.
II
| 7 A.M. | 6 oz. cocoa. |
| 9 A.M. | 4 oz. oatmeal gruel, 2 oz. cream. |
| 11 A.M. | Eggnog. |
| 1 P.M. | Milk broth reënforced with egg. (3 oz. milk, 3 oz. broth, 1 egg white.) |
| [Pg 283] 3 P.M. | Cream, egg and vichy. |
| 5 P.M. | Albumenized milk, 6 oz. |
| 7 P.M. | Hot malted milk chocolate, 6 oz. |
| 9 P.M. | Milk broth reënforced with egg. |
| 12 M. | 4 oz. oatmeal gruel, 2 oz. cream. |
| 4 A.M. | 6 oz. malted milk (half water, half milk). |
Furnishing approximately 1500 calories.
III
| 7 A.M. | Oatmeal gruel, 4 oz., 2 oz. cream. |
| 9 A.M. | Orange eggnog. |
| 11 A.M. | Malted milk chocolate (3 oz. milk, 3 oz. water). |
| 1 P.M. | Clam broth (milk), 6 oz. |
| 3 P.M. | Milk shake, 4 oz.; 2 oz. cream. |
| 5 P.M. | Cornmeal gruel, 4 oz.; 2 oz. cream. |
| 7 P.M. | Hot cocoa, 6 oz. |
| 9 P.M. | Hot malted milk. |
| 12 M. | Hot milk, 4 oz.; 2 oz. cream. |
| 4 A.M. | Hot milk, 4 oz.; 2 oz. cream. |
Furnishing approximately 1460 calories.
The two night feedings may be omitted if patient is asleep.
These diets will be seen to be below the maintenance requirements in health, but the need for care in preventing gastro-intestinal disturbances makes it safer to have it so for a few days, especially if the elevation of temperature is great. After the temperature becomes normal the following foods may be added to the diet:
Soft or Convalescent Diet.—Cream soups, soft-cooked, creamed, or poached egg, soft or baked custard, junkets, egg, cocoa, or plain vanilla ice cream, soft toast, milk or cream, buttered toast, cereals, gelatin jellies, fruit, wine, or meat jellies, vegetable purées, baked white potato, apple sauce, [Pg 284] baked apple, fruit whip, blanc-mange, broiled lamb chops, beefsteak, or chicken, sweetbreads, broiled or creamed brains.
Sample Menus.—The following menu is a sample convalescent dietary:
Breakfast
| 7:30 A.M. | Cream of wheat 3 oz., cream 1 oz. |
| 1 soft-cooked or poached egg. | |
| 1 slice of toast buttered. | |
| 6 oz. cocoa or milk flavored with coffee. | |
| 2 tablespoonfuls of strained prune pulp with 2 oz. cream. | |
| 10:30 A.M. | Albumenized orange juice. |
Dinner
| 12:30 P.M. | Cream of pea soup, 6 oz. |
| 1 baked potato with butter. | |
| 1 slice of buttered toast. | |
| 1 cup of cocoa or 1 glass of milk or buttermilk. | |
| 3:30 P.M. | Ginger ale and milk, 3 oz. each. |
Supper
| 6 P.M. | 2 slices of buttered toast moistened with 4 oz. milk and 2 oz. cream. |
| 1 soft-cooked egg or 3 tablespoonfuls of well-cooked cereal or 2 tablespoonfuls of boiled rice. | |
| 2 tablespoonfuls of apple sauce served with 1 tablespoonful of cream. | |
| 1 cup of cocoa, malted milk, whole milk, or buttermilk. | |
| 9 P.M. | 4 oz. hot milk, 2 oz. cream, or 1 cup of cocoa or malted milk. |
The return to normal diet is made with caution that the digestion of the patient may not be upset or the temperature raised again by over-feeding.
[Pg 285] Energy Requirements.—In fevers of short duration it is not difficult to regulate the amount of food necessary for the maintenance of the patient, since the body will, as a rule, adjust itself when the cause of the fever has been removed. At times, however, it is necessary to make an effort to tempt the appetite of the patient when convalescence is established, that recovery may be made more rapid and complete.
Care of the Mouth.—Probably there is nothing more essential in the treatment of fevers in general and typhoid fever in particular than the care of the mouth. Well-nourished patients rarely ever show the dry, cracked tongue and lips that was formerly one of the common occurrences in typhoid fever. However, in any febrile condition the mouth is apt to acquire a disagreeable taste; this “bad taste” is so prominent in certain cases as to render it difficult for the patient to eat. This can be, to a great extent, eliminated by the use of aseptic mouth washes. When the patient is not strong enough to rinse the mouth before and after eating, the nurse must use a swab for the purpose. The food must be carefully selected and attractively served and every effort made to make food as dainty and palatable as possible.
Thirst.—Thirst is relieved with crushed ice, fruit beverages, and carbonated waters. In certain conditions it is necessary to limit the fluids, but in typhoid fever the giving of the requisite amount of liquids is one of the most difficult tasks confronting the nurse. It is wise to find out the beverages particularly liked by the patient and, whenever it is possible, make use of them. As a rule alcohol is not necessary in the diet of typhoid fever patients. However, in certain cases of that disease, as well as in febrile conditions induced by other causes, the use of alcoholic stimulation may be necessary; it must be left to the discretion of the physician to prescribe it.
Intestinal Disturbances are accountable for the majority of the fevers of short duration during infancy and childhood, and in many of those cases in adults.
Malaria causes an elevation of temperature which is, as a rule, of short duration.
Contagious Diseases, such as scarlet fever, measles, whooping cough, and mumps, are likewise accompanied by more or less elevation of temperature.
Treatment consists of a period of rest in bed, with an abstinence from food, in order that the disease may manifest itself, and also that any offending food material which may cause the fever may have an opportunity to pass out of the body.
The Heart, in some of the diseases accompanied by an elevation of temperature, is more or less strained; this is particularly true in tonsillitis, diphtheria, etc.
The Kidneys are likewise taxed in certain diseases, even when the fever is not great or lasting; this is found to be the case in scarlet fever, tonsillitis, etc.
Dietetic Treatment consists in giving no food for a period lasting from twenty-four to forty-eight hours. This is followed by a liquid diet, milk and broth particularly, which is continued as long as the fever remains.
Convalescent Diet is instituted as soon as the fever has disappeared and acute symptoms subside.
Thirst is apt to be great with any elevation of temperature. It is relieved by water, crushed ice, and fruit beverages.
The Mouth requires much care, even in fevers of short duration. A simple antiseptic wash should be used several times each day.
Nitrogen Equilibrium is not sufficiently disturbed in such cases to require taking into account. Should the [Pg 287] disease, however, develop into one causing a material breaking down of the body tissues, measures must be instituted to prevent the upsetting of the nitrogen balance in the body.
(a) Outline the dietetic treatment for malarial fever.
(b) Outline a diet order, using liquids only. Show method of reinforcing this diet.
(c) Show how the solids are added as convalescence progresses.
[95] In scarlet fever and other conditions in which the kidneys may be involved the above diet is not given unless advised by physician in charge.
Definition.—Typhoid fever is an acute infectious disease excited by specific bacteria (Eberth). The intestines become the seat of ulcerations (Peyer’s patches), which at times perforate. The chief symptoms of the disease are fever, headache, abdominal distention and tenderness, more or less diarrhea and a rose-colored abdominal rash. The source of infection is found in the intestinal contents of a typhoid fever patient, which in some way come in contact with and infect drinking water, milk, etc.
Energy Expenditure in Febrile Conditions.—In febrile conditions the energy expenditures increase as much as twenty-five per cent. In some cases, and when bacterial activity is added to this, as is the case in typhoid fever, the tissue waste becomes correspondingly greater; hence the nutrition assumes the chief rôle in such cases, for in no other way can the tissue waste and energy expenditure be met and overcome.
Energy Expenditures in Typhoid.—In typhoid fever the problem of meeting these expenditures, and at the same time protecting the heart and kidneys from the abnormal strain placed upon them in handling the toxic substances produced as the result of bacterial action in the intestines, becomes very real. It requires eternal vigilance and patience not only from the physician but especially from the nurse, with whom so much responsibility rests. The dietetic treatment necessarily is the principal point to which all efforts must be directed. By this is understood not only the type and amount of food given the patient, but the behavior [Pg 289] of this food in the body as manifested by the symptoms, namely, the appearance of the patient, the condition of the mouth, the abdominal distention, tenderness, diarrhea, nausea, and vomiting, the hemorrhage which at times occurs in spite of all care, and perforation which sometimes results in death, and acidosis or acetonuria. All of which makes this disease one requiring the most efficient attention from a nutritional standpoint.
Energy Requirements in Typhoid Fever.—In a previous chapter the energy expenditures of the normal individual were dealt with; it was seen that a man at rest, that is, in bed, not rising for anything, had a normal expenditure of energy requiring from 1900 to 2200 calories per day. Now, if these expenditures were increased twenty-five per cent. by the fever and still more by the bacterial activities, it is clearly seen that the diet must be increased in proportion if the tissue waste is to be prevented and the normal body weight of the patient maintained.
High Calorie Diet.—Dr. Warren Coleman,[96] to whom we owe so much for his pioneer work in feeding in typhoid fever, devised the so-called “High Calorie Diet.” This consists of foods of the most digestible type prepared in the simplest way. The weight of the patient is considered and the diet directed with the following points in view: (1) to cover the energy requirements of the body; (2) to make good the tissue waste which at times amounts to a loss of from 15 to 20 grams of nitrogen a day (or from ¼ to ¾ pound of muscle);[97] (3) to check or prevent the development of serious complications, kidney, heart, etc.
In the Metabolism Ward at Bellevue Hospital, New York,[98] the best results are obtained by the giving of diets [Pg 290] furnishing from 60 to 80 calories per kilogram per day, or from 4000 to 5500 calories.
Fluid Diet.—It is clearly seen that it would be practically impossible to obtain a sufficient number of calories by using milk alone or even a mixed fluid diet to supply the above requirements. Since milk alone in such a diet would probably cause such discomfort as to make it unwise to continue it, the ideal diet would seem to be one in which the fats, proteins and carbohydrates are furnished in a semi-solid or solid form, together with a sufficient amount of liquids to prevent too great concentration in the food, to relieve thirst, and to act as a carrier of reënforcing substances, such as lactose, eggs, casein products, etc.
Absorption Food.—The question as to whether the food is absorbed when given to typhoid fever patients has often been asked. That it is has been proved in the series of calorimeter experiments conducted in the Metabolism Ward, Bellevue Hospital.[99] Here it was demonstrated that under the high calorie diet the patient consumed large amounts of food with relish and that which was not utilized by the organism immediately was stored for future needs.
Diarrhea and Tympanites.—Constant attention and study of various typhoid patients taking a maximum amount of food a day has proved that the diarrhea and tympanites which at times occur in these as well as other cases are due to too much of one or another of the food constituents rather than to the general amount of the diet. Diarrhea may then be traced to an excess of cream, and the tympanites to an excess of lactose, and a reconstruction of the dietary will often obviate the trouble.
Increasing the Diet.—It is always advisable to “go slow” in adding new foods to the diet; milk, cream, eggs and lactose are the principal articles constituting the diet. [Pg 291] To this are added fine cereal gruels, well-cooked rice, rice custard, tapioca custard, junket, ice cream, wine or fruit jellies, toast, eggs (soft-cooked, poached, creamed, or raw, in milk), or fruit beverages, cocoa, buttermilk, koumiss, certain proprietary infant foods such as Mellin’s Food, Eskay’s Food, Racahout and malted milk, with a well-baked potato, milk, cream or buttered toast added as the condition and appetite warrant.
Milk Diet.—The following milk diets[100] were devised by Dr. Coleman to be given in certain cases of typhoid fever during the acute stage. These formulas consist of milk, cream and lactose and furnish from 1000 to 3000 calories per day.
| Calories | |
| 1000 calories per day— | |
| Milk, 1000 c.c. (1 qt.) | 700 |
| Cream, 50 c.c. (1⅔ oz.) | 100 |
| Lactose, 50 gm. (1⅔ oz.) | 200 |
| This furnishes eight feedings, each containing | |
| Milk, 120 c.c. (4 oz.) | 80 |
| Cream, 8 gm. (2 dr.) | 15 |
| Lactose, 6 gm. (1½ dr.) | 24 |
| 2000 calories per day— | |
| Milk, 1500 c.c. (1½ qt.) | 1000 |
| Cream, 240 c.c. (8 oz.) | 500 |
| Lactose, 125 gm. (4 oz.) | 500 |
| This furnishes seven feedings, each containing | |
| Milk, 210 c.c. (7 oz.) | 140 |
| Cream, 30 c.c. (1 oz.) | 60 |
| Lactose, 18 gm. (4½ dr.) | 72 |
| 3000 calories per day— | |
| Milk, 1500 c.c. (1½ qt.) | 1000 |
| Cream, 480 c.c. (1 pt.) | 2000 |
| Lactose, 250 gm. (8 oz.) | 1000 |
| [Pg 292] This furnishes eight feedings, each containing | |
| Milk, 180 c.c. (6 oz.) | 120 |
| Cream, 60 c.c. (2 oz.) | 120 |
| Lactose, 30 gm. (1 oz.) | 120 |
Varying the Diet.—It has been found possible, even advisable, to vary the above diets in many cases. The disease extends over such a long period that if a fluid diet is adhered to the patient would grow exceedingly tired and even disgusted if milk alone was given, hence a mixed fluid diet such as is used in the Presbyterian Hospital, New York City is suggested.[101]
PRESBYTERIAN HOSPITAL DIET LIST
| 8 A.M. | Milk and coffee, each 120 c.c. (4 oz.). |
| 10 A.M. | Milk, hot or cold, 240 c.c. (8 oz.). |
| 12 M. | Oatmeal gruel, 120 c.c. (4 oz.), with milk 60 c.c. (2 oz.). |
| 2 P.M. | Junket with cane and milk sugar. |
| 4 P.M. | Oatmeal gruel, 120 c.c. (4 oz.), with milk 60 c.c. (2 oz.). |
| 6 P.M. | Junket with cane and milk sugar. |
| 8 P.M. | Hot milk, 240 c.c. (8 oz.). |
| 10 P.M. | Whey, 180 c.c. with 1 whole egg and sherry. |
| 12 M. | Oatmeal gruel, 120 c.c. (4 oz.) with milk. |
| 2 A.M. | Junket with 60 c.c. (2 oz.) can and milk sugar. |
| 4 A.M. | Milk, 240 c.c. (8 oz.). |
| 6 A.M. | Milk, 240 c.c. (8 oz.). |
15 gm. (½ oz.) of lactose added to each of the four milk feedings.
The following foods and diet lists are used with success in various hospitals:
From 1 to 1¼ quarts of milk and 1 pint of cream and lactose, beginning with 1 tablespoonful in each milk feeding [Pg 293] and raising the amount day by day until the patient is taking 2 oz. (4 tablespoonfuls) at each milk feeding, given in eight feedings. This may be given as milk, hot or cold, or it may be made into cocoa, soup, ice cream, junket, or on the cereal.
Milk.
Cream.
Buttermilk.
Whey.
Koumiss.
Zoolak.
Fermillac.
Albumenized fruit juices, egg, and orange juice.
Milk shake.
Broths (chicken, beef, mutton or clam), reënforced with lactose or egg or given plain.
Proprietary infant foods.
Cream soups, beef juice, liquid peptonoids, panopepton.
Orangeade.
Lemonade.
Eggnog.
Milk punch.
Malted milk.
Malted milk shake.
Albumenized milk.
Strained gruels (except oats).
Cream, egg and vichy.
Chocolate malted milk.
Milk gruels.
Eggs—creamed, soft-cooked, poached, custards, baked custards.
Toast—milk or cream toast.
Gelatin—meat, fruit, or wine jellies.
Junkets—plain, egg, or cocoa.
Cereals—fine, strained cereals, except oats.
Rice—boiled or in custard.
Tapioca—custard.
Baked or mashed potato.
Cornstarch or arrowroot pudding.
Ice cream.
Meat is not given until convalescence is established, and then in only the most digestible form, such as rare beefsteak or lamb chop or a small piece of broiled breast of chicken.
| Time | Material | Amount | Calories | ||
| 6 A.M. | Hot milk | 4 oz. | 78 | ||
| Cream | 2 oz. | 76 | |||
| Lactose | ½ oz. (15 gm.) | 60 | |||
| 8 A.M. | Cocoa | Milk | 3 oz. | 59 | |
| Water | 3 oz. | ||||
| Cocoa | 2 tsp. | 35 | |||
| Cream | 1 oz. | 38 | |||
| Sugar | 2 tsp. | 40 | |||
| Lactose | ½ oz. (1 tbs.) | 60 | |||
| Egg | 1 | 60 | |||
| Toast | 1 slice (well moistened) | 73 | |||
| Butter | ½ oz. | 73 | |||
| 10 A.M. | Buttermilk | 6 oz. | 56 | ||
| 12 M. | Cream of pea soup | 6 oz. | 300 | ||
| Mashed potato | 20 gm. | 28 | |||
| Toast | 1 slice | 73 | |||
| Butter | 20 gm. | 84 | |||
| Coffee and milk | 3 oz. each | 59 | |||
| Cream | 2 oz. | 76 | |||
| Sugar | 2 tsp. | 40 | |||
| Lactose | 20 gm. | 80 | |||
| Orange juice and egg | Orange juice | 3 oz. | 38 | ||
| 3 P.M. | Egg | 1 | 60 | ||
| Lactose | 30 gm. | 120 | |||
| 5 P.M. | Farina | 3 oz. | 102 | ||
| Milk | 2 oz. | 59 | |||
| Cream | 2 oz. | 76 | |||
| Lactose | 20 gm. | 80 | |||
| Egg | 1 | 60 | |||
| Apple sauce | 1 oz. | 30 | |||
| Cream | 1 oz. | 38 | |||
| Cocoa | 6 oz. | 108 | |||
| or | |||||
| Tea and | 3 oz. | 0 | |||
| Milk | 3 oz. | 78 | |||
| Sugar | 2 tsp. | 40 | |||
| Toast | 1 slice | 73 | |||
| 7 P.M. | Gruel | 4 oz. | 102 | ||
| Cream | 2 oz. | 76 | |||
| Lactose | 15 gm (½ oz.) | 60 | |||
| 9 P.M. | Broth | 6 oz. | 18 | ||
| Egg white | 1 | 13 | |||
| [Pg 295]12 M. | Milk | 4 oz. | 78 | ||
| Cream | 2 oz. | 76 | |||
| Lactose | 20 gm. | 80 | |||
| 3 A.M. | Milk or | 4 oz. | 78 | ||
| Malted milk | 1 tbs. | 58 | |||
| Cream | 2 oz. | 76 | |||
| Lactose | 20 gm. | 80 | |||
| Total calories 3145 | |||||
Advantages of Newer Treatment.—A marked difference is noticed in the patients treated by the old starvation diets and those given the high calorie diet. Dr. Coleman states[102] that while the range of temperature is apparently unaffected, the total duration of the disease is shortened in some instances by months through the shortening of convalescence. He further states that certain symptoms which have hitherto been attributed to the specific action of the typhoid bacillus have been discovered to be due to faulty methods of treatment, particularly to an inadequate or improperly balanced diet. The various investigators who have made the study and treatment of this disease a lifework claim that the mortality from this disease has been tremendously reduced by the use of the high calorie diets which maintain the nutrition of the patient throughout the disease, thus eliminating the horrors of the long, tedious convalescence which tried the nerves and patience of the patient, the nurse, and the physician. There is no doubt that so far as the administering of this diet is concerned it requires more effort on the part of the nurse than the old treatment of a glass of milk every two or three hours. It is necessary for the nurse to be able to carry out the [Pg 296] orders as expressed in the diet lists, to be able to compute the proteins (nitrogen), fats, and carbohydrates in a food or recipe. But this is readily done by studying the tables given in the first section of this text. She must likewise be able to recognize the symptoms as they arise. In hospitals, the urinalysis is made as a routine procedure. In private cases the physician will either have the analyses made or expect the nurse to be able to make the simple tests.[103]
One of the greatest difficulties attending the administering of the high calorie diet is persuading the patient to take sufficient food for his needs. The fluids are often more difficult to give in quantity than the more solid foods, and it requires much tact on the part of the nurse to prevent a refusal of the necessary fluids. However, if the patient is possessed of even ordinary intelligence, an explanation of the reasons for the large amount of food will as a rule be all that is necessary. Few individuals will willingly prolong an illness attended with the discomforts generally present in typhoid fever.
Hemorrhage occurs in a certain percentage of cases of typhoid regardless of the diet, whether it be a strictly milk diet or the high calorie diet just described. The measures to combat them are essentially the same. It is necessary to guard against excessive tympanites since the pressure therefrom against the ulcerated intestinal walls may cause perforation resulting in hemorrhage. Lactose at times causes an evolution of gas as do fats under certain circumstances. Hence it is necessary to follow symptoms and watch the stools in order to determine which food material is to blame for the tympanites and reduce the allowance of that food in the diet.
Idiosyncrasies against Milk.—Certain individuals manifest an inability to take milk. This may be real or imaginary. When it is a true idiosyncrasy, it may be found [Pg 297] necessary to substitute some other food for the milk in the diet, but great care should be taken to determine the real character of the disagreement before eliminating so invaluable a food from the diet. When the disagreement proves merely a distaste for milk, some of the different methods used in disguising it, such as flavoring or coloring, may be practiced. Otherwise, it is well under the circumstances to use some of the pre-digestive methods in order to increase its utilization. It is well to emphasize the value of accurate data on this subject as it is exceedingly difficult to administer a high calorie diet without milk in some form.
Essential Points.—Thus the dietary in typhoid fever is seen to be the most important part of the treatment. A careful study of the tables will enable the nurse to do her part in nourishing the patient. It is necessary that she be able to compute the nitrogen, carbohydrates, and fats in a diet and arrange these constituents in such a way as to give the desired amount of each in the dietary and in a form acceptable to the patient.
Rate of Metabolism is greatly increased in typhoid fever even over other febrile conditions, not only on account of the elevation and duration of the fever, but also on account of the activities of the specific bacteria in the intestinal tract which differentiate this disease from other febrile conditions.
Energy Expenditures and Requirements of the body in typhoid fever, on account of the character of the disease, are much greater than those of the normal individual and must be met by an increase in the diet if the body is to be saved from destruction.
The Bowels.—Diarrhea develops during any period of the disease due to excess amount of fat or to a disagreement of some of the other food constituents. It is advisable to [Pg 298] cut down the allowance of cream temporarily and to watch stools and other symptoms for evidences of dietetic errors.
Hemorrhage must be guarded against by eliminating, as far as possible, all substances liable to cause an excessive gas formation in the intestines.
Absorption of Food is as a rule good. The patient is usually able to handle a large quantity of food provided it is judiciously administered with a due regard to the symptoms manifested at the time.
Simplicity of Diet is absolutely essential. All the materials must be selected carefully according to the physician’s orders and prepared with the greatest care in order to prevent digestive disturbances.
High Calorie Diet is one in which the fuel value of the food ingested meets or exceeds the energy expenditures of the patient. Foods composing the diet are, milk and eggs for the proteins, with carbohydrates and fats in their simplest and most digestible form to balance the diet.
Administering a High Calorie Diet is accomplished successfully provided the nurse exercises care with regard to the symptoms arising from time to time. These must be carefully noted and reported to the physician, for in this way only is it possible to give a sufficient quantity of food to cover the excessive breaking down of the body due to the disease.
Fluid Diet is at times necessary since certain patients cannot tolerate a high calorie diet, but this is a point decided by the physician. A fluid diet consists of fluids alone, milk in particular, with broths and fruit beverages as ordered. The milk is given in definite amounts and at stated intervals.
Milk Diet is one consisting solely of milk or in which the bulk of the nourishment is furnished by milk. It may be reënforced or not as desired. Lactose is the substance commonly used as a reënforcing agent. It is impossible to [Pg 299] cover the energy expenditures of typhoid fever with a milk diet even if it is perfectly administered, but certain complications make it, at times, the only rational method of feeding.
The Advantages of High Calorie Diet over other diets are distinctly noticeable in typhoid fever patients. Those treated by this method are more comfortable during the course of the disease and are saved a long, tedious convalescence which has made the starvation treatment a thing of horror in the past. The return to health is attended by a much better physical condition when the patients are well nourished than is possible when they are kept on practically a starvation ration. The mortality from the disease has been materially lessened by the administration of the high calorie diet.
Acidosis may develop in typhoid fever patients and must be guarded against. The behavior of the fat in the body should be carefully watched and the amount reduced at the first evidence of acidosis. At the same time an increase in the carbohydrates may assist in overcoming the condition. This adjusting of the diet, however, is entirely in the hands of the physician.
The Kidneys in typhoid fever patients are under a great strain, chiefly on account of the increased rate of metabolism. Great care must be exercised in the dietetic treatment to prevent these organs from being overworked with a consequent development of nephritic conditions.
Care of the Mouth in any febrile condition is important, but especially so in typhoid fever, where the disease itself causes a most unpleasant taste in the mouth. This prevents the taking of nourishment with any degree of comfort, hence the mouth should be cleansed before and after each feeding. Any of the aseptic mouth washes may be used.
Thirst may be relieved by plain or carbonated waters, [Pg 300] fruit beverages, and crushed ice. When in certain complications the fluids in the diet are in a measure restricted, ice is used and water is given in spoonful doses. This, however, is the exceptional, rather than the ordinary state of affairs.
Increasing the Diet after a fluid diet must be made with great care in order to prevent a relapse. Following the high calorie diet the increase is simple. The patient passes from the prescribed foods to meat with apparently no effort. The increase should not be made, however, until convalescence is firmly established.
Reënforcing the Diet.—On account of the great increase in the rate of metabolism and because of the difficulty of furnishing the requisite number of calories in the diet, reënforcing agents such as lactose, eggs, some forms of casein, or beef preparations are used.
Idiosyncrasies against certain foods are, at times, manifested by patients. Efforts must be made to determine whether they are real or imaginary before eliminating any food which may be of importance to their future welfare.
(a) Give a sample diet order, using liquids only. Raise the fuel value of the diet from 2000 to 3000 calories.
(b) Formulate a diet order, using the high calorie diet, fuel value 3500 calories.
[96] Warren Coleman, University and Bellevue Hospital Medical College, Visiting Physician, Bellevue Hospital, New York City.
[97] “Diet in Typhoid Fever,” by Warren Coleman, “Journal of American Medical Association,” Oct. 9, 1909, Vol. LIII.
[98] “Diet in Typhoid Fever,” by Warren Coleman, reprint from “Journal of American Medical Association,” June 9, 1909.
[99] Determined by calorimeter observation from the Russell Sage Institute of Pathology in affiliation with the Medical Division of Bellevue Hospital, under Warren Coleman and Eugene DuBois.
[100] “American Journal of Medical Sciences,” January, 1912, by Warren Coleman.
[101] F. P. Kinnicut, “Diets Used in the Presbyterian Hospital,” New York City.
[102] “Journal of American Medical Association,” Aug. 4, 1917.
The dietetic treatment for tuberculosis must, as in any other pathological condition, depend largely upon the general condition of the patient, and the symptoms manifested at the time.
Character of Disease.—The disease may have reached an acute stage in which the rise of temperature is marked and the progress of the tuberculous symptoms rapid, or it may be found to be an old chronic condition in which the progress is slow.
Again, the patient may be found to be suffering from a tuberculosis which is neither acute nor very slow. Each of these stages requires slightly different treatment which, however, for the main part is much the same.
Individuals having an incipient form of tuberculosis have been known to develop an acute form of the disease upon being subjected to a strenuous treatment for some other and entirely different condition. This has been especially noticeable in certain individuals to whom the starvation treatment is given.
Dietetic Treatment in Acute Stage.—The dietetic treatment of the acute tuberculosis under such circumstances must necessarily be adapted to that of the original disease for which starvation was believed to be necessary. The forbidden foods must still be omitted from the dietary, but in these cases it is found advisable not to prolong the [Pg 302] starvation treatment but to substitute foods which will do the least harm under the circumstances. This is necessary to cover the energy requirements of the body and to make good the tissue wasted through the development of the specific disease.
Dietetic Treatment in Chronic Stage.—The diet for tuberculosis has been so widely discussed and so universally used that a few words only seem necessary here. One of the chief points to be emphasized is the danger arising from gastro-intestinal disturbances. The digestive apparatus of the tuberculous individual is more apt to be impaired, so that any undue exertion required to digest a meal is likely to bring about disturbances more or less serious in character.
Method of Administering Diet.—For this reason it is no longer the custom to stuff the patient in an effort to overcome the inevitable tissue waste, since such treatment in many cases defeats the end for which it was intended, bringing on acute indigestion, or at times diarrhea, which might readily cause a greater loss of body weight than could possibly be produced by the surplus food given.
Adjusting the Diet.—More and more is it coming to be understood that the diet must be adjusted to suit the individual. Three wholesome meals a day are insisted upon, with lunches given between the morning and midday meal and during the course of the afternoon. Many patients are found to sleep better after they have partaken of a light lunch, consisting of hot milk, malted milk, or like beverages and crackers, so that this third meal is added to the other five. In this way the individual suffering with tuberculosis is assured of an efficient diet to meet the needs of the body without overburdening the digestive apparatus or overtaxing the excretory organs. The increased metabolism taking place in such patients, due both to the specific bacteria and to the febrile condition, is, as far as possible, provided for.
[Pg 303] Schedule of Diets.—The following dietary régime may be useful in formulating menus for tubercular patients:
Breakfast
Fruits.
5 oz. cereals with cream.
1 or 2 eggs, simply prepared to prevent indigestion.
2 slices of bacon, ham; fish cake or chop.
2 slices of toast or crusty rolls with butter.
Coffee, tea, or cocoa, with or without cream.[104]
Lunch
Vegetable or cream soups.
Cold meat, lamb chops, oysters, or fish.
Baked white or sweet potato.
1 green vegetable,—greens, cabbage, spinach, or string beans.
Stewed fruit or baked apple.
Rice or tapioca pudding.
Tea.
Bread and butter.
At the end of the meal one glass containing two-thirds milk and one-third cream. If the latter disturbs the digestion reduce the amount temporarily, or add one-half the contents of a tube of peptonizing powder, or one-quarter of a glass of limewater.
Dinner
Meat, lamb, mutton, chicken, duck, game, or fish.
Mashed or creamed potatoes.
1 or 2 green vegetables.
Simple salads.
Simple desserts consisting of puddings, custards, wine or fruit
jellies, ices or ice cream, sponge cake or angel food cake.
[Pg 304] The milk and cream is taken at the end of the meal as directed above.
Lunches
11 A.M., 4 P.M., 9 P.M., consisting of milk, malted milk, junket, buttermilk, albumenized broth, albumenized fruit juices, cream, egg, and vichy, eggnogs, served with crackers or sponge cake; cereal gruels and raw eggs taken with water, milk, or sherry may likewise form a part of this diet, since the nourishment in them is both concentrated and palatable.
Use of Eggs.—The old method of forcing the patient to eat a dozen or more raw eggs a day is no longer used, but three or four a day will be of undoubted value to the patient, provided they agree. There are patients, however, with whom eggs act almost as a poison, and in these cases it is decidedly unwise to force them.
Use of Milk.—Milk is to be used abundantly. If it should disagree, it may be peptonized or modified with limewater. At any rate, every effort should be made to enable the patient to drink at least one quart a day, and more, if possible.
If it fails to agree even when so treated, it should be abandoned, since the discomfort caused under the circumstances is more detrimental to the welfare of the individual than any benefit which he may gain by the small amount which may be absorbed.
High Calorie Diet.—As long as the patient is in bed the diet cannot be as full as it is made when he is up and about, as the body is then using more material to provide for the extra exertion and needs more food to replace that which has been utilized. Consequently the high calorie diet[105] will be found as a rule sufficient. As soon as the patient is able to receive more food without incurring digestional disturbances, it should be supplied, keeping ever in mind the danger of its upsetting his digestion.
[Pg 305] Advice to Patients.—The patient must be impressed with the necessity for living a simple, wholesome life, free from excesses of all kinds. The need for a regular régime in the beginning must be strongly emphasized. Too strenuous exercise and the consequent over-fatigue at times completely overcome all the good which has been accomplished in weeks or even months of studied effort, so that rest is an essential part of the tuberculous régime. The patient should sleep from eight to ten hours out of every twenty-four, and if this sleep is taken in the open, that is, in a tent or on a sleeping porch, the benefits derived therefrom are inestimable.
The Bowels.—The bowels should move every day, even if some gentle laxative or an enema has to be used to bring about the desired result. In a majority of cases, mineral oil or bran muffins, prunes, raisins, and figs prepared with senna will be entirely sufficient, however, and these substances are much less harmful than drugs, for the habit of taking purgatives becomes a fixed one in a short time, and is especially liable to become so when the patient is forced, by reason of the sedentary life, to depend on some such measures.
Massage.—Massage has been found beneficial in many cases, giving the needed exercise to the body, which it is otherwise unable to obtain.
In chronic tuberculosis, the patient should be instructed in the care necessary for his protection. He should be advised to report to the physician any symptoms occurring during the course of the disease, especially any hemorrhage. He must be reassured of the chances of recovery, even after hemorrhage has occurred. It is not well to encourage the habit of taking the temperature or weighing daily, since the knowledge of the fluctuations which inevitably occur in [Pg 306] these conditions may worry the patient to such an extent as to interfere with his final recovery.
Rest, Sleep, and Fresh Air.—Moderation in physical exertion, wholesome food at regular intervals, plenty of rest and sleep, preferably in the open, and an effort made to look forward to a complete recovery will go far toward bringing about the desired result. The tuberculous patient who sets his mind on recovery, refusing to be discouraged by the numerous setbacks which may from time to time occur, has a much greater chance of living a long and useful life than the patient who makes no effort in this direction.
Reënforcing the Diet.—The following reënforced foods have been found valuable in the diet for tuberculosis, especially in those cases which are confined to bed and in which the effort to eat causes more or less gastric distress:
Milk, whole milk, milk and cream, milk diluted with Apollinaris water, peptonized, modified milk, reënforced with egg or egg white or reënforced with one to four tablespoonfuls of lactose, malted milk, buttermilk, cream, egg, and vichy, milk shake, milk punch, malted milk shake, chocolate or cocoa malted milk, albumenized fruit juices, egg and orange, egg and wine, reënforced, if desired, with lactose, albumenized broths, proprietary infant foods, such as Eskay’s Food, Nestlé’s Food, Mellin’s Food, Racahout, cream soups reënforced with lactose or egg, junkets, and ice cream.
The diet in pneumonia is of considerable importance, since in this condition the strength of the patient is taxed by reason of the character of the disease, and the only means of attaining endurance to carry him through this trying period is by providing proper nourishment.
Dietetic Treatment.—The same general outline of diet is used as in acute infectious fevers, milk forming the basis of the diet. The patient is given an abundance of water and [Pg 307] other beverages in addition to the other fluid foods to relieve the thirst which is so often a common symptom in this disease.
It is sometimes found advisable, however, on account of the vomiting which may occur, to give a more concentrated form of nourishment, in which case liquid peptonoids, trophonine, and panopepton furnish a form of nourishment which is both strengthening and stimulating in character, and for these reasons particularly desirable. Freidenwald and Ruhräh advise against the use of starches and sugars in most cases of pneumonia.
Daily Diet Schedule.—The same fluid diets used in acute fevers and administered at two-hour intervals are advisable here. The following régime is used in pneumonia:
| 6 A.M. | 6 oz. malted milk. |
| 8 A.M. | 6 oz. cocoa. |
| 10 A.M. | 4 oz. oatmeal or cornmeal gruel with 2 oz. cream. |
| 12 M. | 6 oz. chicken broth reënforced with 1 egg white. |
| 2 P.M. | 6 oz. malted milk chocolate. |
| 4 P.M. | 6 oz. albumenized orange juice. |
| 6 P.M. | 6 oz. chicken or beef broth, reënforced with egg white. |
| 8 P.M. | 6 oz. hot milk. |
Night feeding consisting of milk, malted milk, or reënforced broth may be given at 12 M. and 4 A.M. if patient is awake.
The above diet may be varied by adding some of the beverages mentioned in the diet for tuberculosis or fevers.
Convalescent Diet Schedule.—As the acute symptoms subside and convalescence advances, the following diet may be instituted:
I
| Breakfast | 3 to 4 oz. cereal gruel with 2 oz. cream. |
| 1 soft-cooked egg. | |
| [Pg 308]10:30 A.M. | 6 oz. chicken broth, reënforced with egg, or 6 oz. albumenized orange or grape juice. |
| 1 P.M. | 6 oz. oyster soup with rolled crackers. |
| ¼ cup wine jelly with 1 tbs. cream. | |
| 1 glass (6 oz.) milk—2 parts milk, 1 part cream. | |
| 3 P.M. | Milk shake (4 oz. milk, 1 egg white). |
| Supper | 4 oz. farina with 1 oz. cream. |
| 6 oz. cocoa. | |
| 9 P.M. | 6 oz. malted milk. |
| Hot milk, broth, or malted milk may be given during the night at 12 or 4 A.M. if patient is awake. | |
II
| Breakfast | 4 oz. orange juice on cracked ice. |
| 3 or 4 oz. strained oatmeal with cream or butter. | |
| 1 slice soft toast. | |
| 6 oz. cocoa. | |
| 10 A.M. | 1 soft-cooked egg on toast. |
| 6 oz. milk. | |
| Dinner | 6 oz. cream of celery soup. |
| 2 oz. rice. | |
| 4 oz. custard (soft or baked). | |
| 6 oz. milk or cocoa. | |
| 3 P.M. | 5 oz. cream, egg, and vichy. |
| Supper | 1 soft-cooked egg. |
| 1 small baked potato. | |
| 6 oz. cocoa or malted milk. |
III
| Breakfast | Stewed prunes. |
| 3 or 4 oz. cream of wheat with 1 oz. cream. | |
| 1 soft-cooked egg. | |
| 1 slice of toast with butter. | |
| 6 oz. cocoa or milk. | |
| [Pg 309]10:30 A.M. | Eggnog (1 egg, 4 oz. milk, 2 oz. cream, 1 tbs. whisky or sherry wine). |
| Dinner | Cream of spinach soup. |
| 2 oz. mashed potatoes. | |
| 2 oz. green peas. | |
| 1 slice toast with butter. | |
| 2 oz. rice or tapioca custard. | |
| 3 P.M. | 6 oz. albumenized fruit juice. |
| Supper | 1 slice toast. |
| 1 poached egg. | |
| 6 oz. cocoa or hot milk. | |
| 2 or 3 oz. stewed fruit or prune whip. |
The diet may be reënforced with lactose and meat added only when convalescence is well established.
Tuberculosis Nursing.—The nurse must keep in mind that the lungs are in a condition more or less out of commission, and their work of excretion is forced upon the kidneys. For this reason, as well as on account of the increased strain upon the heart, it is necessary to keep the diet light and avoid all foods which may in any way exert an unfavorable influence upon either the kidneys or the heart.
Milk Diet.—A strict milk diet has been found necessary in certain cases of pneumonia, but this is used only while the febrile condition lasts, after which the diet is gradually increased, as in the case of acute nephritis and in diseases of the heart, to meet the needs of the individual.
Dietetic Treatment.—The diet in this condition is much the same as that used in other acute febrile conditions, that is, a fluid diet, the basis of which is, as a rule, milk.
The development of nephritis and certain cardiac symptoms at times follow attacks of tonsillitis, and for this reason the urine must be examined frequently and the diet [Pg 310] carefully adjusted to avert, if possible, this danger. When acute nephritis does follow the attack of tonsillitis, the diet must necessarily be adjusted to meet that condition rather than that of the original disease.
Special Diets.—The Mosenthal diet, and at times the Karell Cure, is used with more or less success. This, however, is adjusted by the physician. It remains for the nurse to report any unfavorable symptoms as soon as they occur, and to carry out the line of dietetic treatment deemed advisable by the physician.
Form.—Acute and chronic in character. The chief aim of the treatment in the former is to prevent its development into a chronic form.
Rest.—Sleep, preferably in the open air, in a tent or on a sleeping porch.
Proper Surroundings should be striven for. The patient should be kept tranquil in mind and body, free from disturbing worries and assured of the possibility of recovery with proper care.
Diet should be adequate without being too abundant; stuffing the patient is no longer considered necessary, in fact it is believed that forcing the eating of large quantities of eggs, etc., defeats its own ends, upsetting the digestion and causing a disgust for food almost impossible to overcome.
Gastro-intestinal Disturbances are apt to develop as the disease progresses. These are treated as in other conditions so complicated, except that the period of starvation must necessarily be limited on account of the metabolic waste already taking place from the disease itself.
The Lungs, as in pulmonary tuberculosis, are the seat of infection and are temporarily hampered in their work of excretion.
The Kidneys bear the brunt of the extra work caused by the impairment of the lungs, consequently all unnecessary work must be spared these organs if they are to be prevented from being overtaxed.
Nephritis is one of the complications apt to develop when the kidneys are not sufficiently strong to carry on their own work and that generally done by the lungs.
The Heart.—Cardiac symptoms are also likely to develop during attacks of pneumonia and make the disease one to be dreaded and guarded against.
The Diet.—The dietetic treatment in pneumonia is like that used in acute infectious diseases, fevers in general, fluids constituting the form of diet and milk the chief food, as long as there is an elevation of temperature.
The Heart.—As in pneumonia, the development of cardiac symptoms must be guarded against. These symptoms may not develop at once but show later during or after convalescence.
The Kidneys.—Nephritis also develops in some patients and the treatment is directed as far as possible to prevent its developing into a chronic form.
Dietetic Treatment is the same as used in acute infectious conditions, fevers of short duration, taking care to institute the diet for acute nephritis should the patient show evidences of this disease.
Write a diet order for a tuberculous patient weighing 135 pounds, allowing 3000 calories and fifty per cent. of the protein to be derived from animal sources.
[104] The addition of cream to coffee produces acute indigestion in certain individuals, hence the nurse must be governed by this point in formulating the diet.
The dietetic treatment which is essential before and after operations is deserving of attention here, since it constitutes one of the points so frequently overlooked or slighted. As a rule the treatment depends (1) upon the character of the disease for which surgical intervention is necessary, and (2) upon the general health and physical condition of the patient in question.
Preparatory Treatment.—In many cases it is found to be advisable to build up the patient before subjecting her to the shock of an operation, and the more serious the operation the more necessary this “building-up” process.
The character of the disease also has much to do with the preliminary diet. In certain pathological conditions involving the gastro-intestinal tract, for example, the patient comes to the surgeon after medical treatment has failed to give relief and surgical intervention is necessary to save life. The body is found to be in a condition bordering on starvation, anemic and exhausted from insufficient nourishment. The functions of the blood-making organs have become out of gear, as it were, and the blood consequently is deficient in one or more of its essential elements. For such patients it is wise to attempt to reënforce and strengthen their bodies before operation, that they may have more endurance to withstand the shock which is more or less unavoidable.
[Pg 313] Adjusting the Diet.—In any case where preliminary diet is prescribed the condition for which the operation is necessary determines the nature of the diet; for example, if the operation is to be upon the kidney, the diet beforehand would naturally be in the nature of a nephritic one to save the diseased organ unnecessary work. If the stomach or intestinal tract required surgical care, the diet would necessarily be formulated to meet the particular needs of the organ in question, an analysis of the stomach content furnishing the keynote of the diet. In any case the food must be simple in character and well prepared. All food in any way liable to bring about indigestion should be studiously avoided.
Habits.—The habits of the patient must be regulated so that she may not “overdo”; at the same time, gentle exercise may be the very thing needed to give an impetus to the appetite and thus assist in the adding of strength for the approaching ordeal. Many patients respond readily to a change of air and scene and frequent small meals instead of a few large ones,—a lunch in the mid-morning and mid-afternoon hours, consisting of a glass of milk and a cracker or malted milk chocolate or reënforced fruit juices. A cup of warm milk before retiring induces the much-needed sleep, hence is advisable under the circumstances.
The Bowels.—The bowels must be kept open. Coarse bread such as that made from bran or graham flour is advisable. Prunes and figs cooked with senna leaves are likewise simple laxatives which are both palatable and effective. For stubborn cases of constipation it is often found that a teaspoonful of a conserve made with a third of a pound each of raisins, prunes, and figs ground fine, with an ounce of senna leaves added, taken at bedtime and before breakfast, will overcome the condition and make the patient more comfortable and the general health better.
Preliminary Light Diet.—The day before the operation [Pg 314] the diet must be light; the intestinal tract must not be filled with a food mass which is difficult to get rid of. On the morning of the operation the patient is given no food if the operation is to be performed at an early hour, otherwise a cup of tea, coffee, weak cocoa, or broth with a cracker is given. Some physicians give a glass of milk at this time, while others do not. It is the physician who must decide the question if there is any doubt about it. The stomach must be empty before administering the anesthetic.
In certain emergency operations when it has been impossible to prepare the patient ahead, the difficulties attending the administering of the ether are sometimes greatly increased. The cleansing of the stomach and intestinal tract oftentimes eliminates or materially decreases the nausea and vomiting which so often forms one of the most dreaded sequences of the operation. For this reason many surgeons require the patient to be given lavage before leaving the operating room.
Total Abstinence.—No food is given for twenty-four hours following the operation (1) on account of the nausea and vomiting which so often follows the giving of an anesthetic—ether particularly—and (2) because the entire organism is better for a complete rest.
Routine Treatment.—The routine treatment in uncomplicated cases is rest, then water, very hot or iced, or carbonated, or vichy in spoonful doses, then albumen water, broth, etc., then milk, buttermilk, koumiss, etc., after which the semi-solids, etc., until a normal diet is reached. After a week or more the character of the operation certainly determines the dietetic treatment. To quote Dr. Thomas S. Brown,[106] “To give the same diet after pyloroplasty, gastro-enterostomy, gall bladder operation, or gastric resection [Pg 315] as we would after operations for fracture of the thigh or cancer of the breast shows a basic ignorance of the pathologic physiology of the former group of cases.” “We should remember that hyperacidity remains long after the underlying cause has been removed and it is tempting providence, to say the least, to ply these patients with tomato soup, salad dressing, and coarse food in the early stages of their convalescence.”
Character of Diet.—It must be kept in mind that the character of the diet is of vital importance, especially in the after-treatment of operations upon the stomach. In gastro-enterostomy, for example, the food mass passes from the stomach directly into the upper part of the small intestine through the new opening. Thus the semi-liquid food highly acid in character comes in direct contact with the delicate intestinal walls which are accustomed, not to the acid, but to a neutral or alkaline medium.
Adjusting Diet to Disease.—Thus it is demonstrated that unless care is used in selecting the diet this portion of the intestinal tract will be injured; hence the nurse must understand which foods are liable to stimulate an excess flow of acid in the stomach and avoid them. She must also keep in mind that the foods given must be in a semi-liquid or very finely divided condition, since the mechanical efforts made by the musculature of the gastric organ act as a direct stimulant to the secretory cells of that organ.
Much of the responsibility thus rests upon the nurse whose business it is to administer the diet. The efforts of the best surgeon in the world may be entirely overcome by a careless, thoughtless, or ignorant nurse.
Rectal Feeding.—In some cases it is found necessary to nourish the patient more than is possible by mouth. This is especially so with emaciated and very weak patients and for those who have undergone operations upon the [Pg 316] mouth or throat and in some of the above-mentioned stomach cases when the passage of any food over the newly-operated-upon surfaces is inadvisable. In these cases rectal feeding is resorted to and from two to three nutrient enemas[107] alternated with saline enemas are given daily.
Under ordinary conditions when the patient has not been operated upon for gastro-intestinal disorders, gall bladder or kidney diseases, the dietetic régime is as follows:
Postoperative Feeding.—First day: starvation, a little hot or cold water or carbonated water may be given if there is no nausea or vomiting. If nausea or vomiting persists, a few spoonfuls of champagne or clam broth or juice will often check or relieve it entirely. Fluids alone must be given during the first forty-eight hours after the operation. When stimulation is necessary, albumen water or coffee containing a spoonful of brandy[108] will be found useful. When nausea entirely disappears, well-skimmed broth milk, clam or oyster broth, buttermilk, koumiss, malted milk, may be given. A gradual return to the normal diet is made, adding soft toast, soft-cooked eggs, junket, ice cream, meat, wine, or fruit jellies before solid food is introduced into the dietary.
After-care in Feeding.—Care must be observed to prevent indigestion after almost any operation, but especially after abdominal operations there is a great tendency to form gas, hence anything which in any way increases the tendency may bring about a condition of extreme discomfort and even acute pain to the patient. For this reason it is unwise to follow too closely the desires of the patient as to the food to be eaten; for example, corned beef and cabbage may be the thing of all others desired by the patient, but it would be the height of folly to risk such a meal until all danger of digestional disturbances is at an end. It [Pg 317] is wiser to avoid such disturbances than to trust to relieving them after they occur. The digestion of even a perfectly normal individual is at a disadvantage when that individual is deprived of outdoor exercise. How much more so will it be when the entire organism is taxed by the ordeal through which it has just passed. Convalescence is never hastened by imprudent eating, and a condition as bad as the original may be brought on by lack of care on the part of the one whose business it is to feed the patient.
Diet After Appendicitis.—After a simple operation for appendicitis the same régime is carried out as in stomach and intestinal operations: fluids on the second day, soft diet on the third, and solid food of the simplest character and prepared in the simplest way may be given on the fifth and sixth days. When, however, the operation has been of a more serious character, for example, when there was pus formation or a gangrenous appendix, the feeding by mouth must not be instituted for five days or more, nutrient enemas being used instead. Patients have been known to die from exhaustion after operations upon the stomach and intestines, not on account of the operation but on account of the lack of reserve power and endurance to carry them through the ordeal without a sustaining diet to overcome it. Under the circumstances Dr. F. Ehrlich[109] advises the following routine method: “So soon as the nausea from the anesthetic has worn off the patient gets tea, red wine, and gruel; on the day after the operation he is given sweetbreads in bouillon even if it nauseates him; if the nausea is persistent, his stomach is washed. On the second day finely chopped cooked squab, chicken, or veal, is added; on the third day, beef, potato purée and cakes; on the fourth, chopped (raw) ham, soft zwieback, and soft-boiled eggs. [Pg 318] On the fifth, white bread and spinach. After the seventh day the meat is not chopped, and the patient returns gradually to normal diet. The bowels are regulated by oil enemas.”
Diet After Operation upon Gall Bladder or Liver.—The dietetic treatment in these cases is like that of any other abdominal operation except for the character of the food. Fats are not well handled by the body of such individuals and should be eliminated as far as possible from the diet. Broths must be skimmed carefully to remove fat, and milk when given should be skimmed or given in the form of buttermilk or koumiss.
Diet After Operations upon the Kidneys.—The diet administered after operations upon these organs is logically one in which those foods which are entirely dependent upon the kidneys for their elimination are restricted. In a former chapter the fate of the foods in metabolism was explained; the protein foods were seen to be the ones leaving the body chiefly by way of the kidneys and for this reason in the diet after operations upon these organs, as well as in that administered in disturbances affecting their functioning powers, this food constituent, the protein of meat in particular, must necessarily be restricted. The upsetting of the nitrogen equilibrium is for so short a period after kidney operations that this feature need not be considered here. The diet under the circumstances is essentially the same as that given during acute attacks of nephritis.
Factors Affecting Diet before and after operations must be considered under two heads, namely, the character of the disease for which the operation is considered necessary and the general physical condition of the patient at the time.
Emaciation and Anemia are often encountered in [Pg 319] patients having certain gastro-intestinal disturbances for which surgical intervention was found to be necessary. At times a preliminary up-building treatment is required before it is considered wise to submit the patient to the shock of so serious an operation.
Adjusting the Diet according to the character of the disease for which the operation is to be performed is most important. It is not always possible to build up the body beforehand, but in many cases it is necessary to make the effort. At times the reënforcing of the diet and a certain amount of gentle massage will enable the patient to pass through the trying ordeal more comfortably than would otherwise be possible.
Selecting the Diet to conform to the character of the disease is as important a factor in the recovery of the patient as food itself. This selection is left largely to the nurse, consequently it is necessary that she should understand just which foods are indicated or contraindicated under the circumstances, and adjust the diet after the abstinence period accordingly. For example, the diet fulfilling all the needs of a patient who has just undergone an operation for a broken leg might be highly injurious for a patient just operated upon for some disturbance of the liver or kidneys. The diet given after must be essentially like that given just before the operation, in order that the affected organ may have an opportunity to heal and return to its normal functioning power.
Gastro-intestinal Disturbances must be avoided, both before and after the operation. In the preliminary treatment, when every effort is being made to increase the strength and endurance of the patient, such disturbances do away with any gain brought about by judicious dieting. After the operation, attacks of indigestion not only cause pain and discomfort as a result of the gas formation, but [Pg 320] may cause symptoms far-reaching and even dangerous in their effects. The diet, then, must be composed of the simplest food and prepared in the most careful manner, the amount of food given at a time must be small—it is wiser to feed the patient oftener than to run the risk of indigestion by giving more than can be readily handled by the already taxed digestive apparatus.
The Bowels must be kept open in the majority of cases. Peristalsis is stimulated by the giving of water and fruit beverages as soon as it is advisable to give anything by mouth.
Reënforcing the Diet is at times necessary in order that the patient’s strength may be kept up. In such cases lactose, eggs and some of the predigested casein or beef preparations are found to be valuable.
Before the Operation the patient must be made ready to take the anesthetic. This is done by preventing an accumulation of food in the intestinal tract. The day before the operation, then, it is necessary to limit the diet materially by giving food in small amounts. The light diets prescribed in acute conditions are as a rule suitable, unless otherwise indicated.
The Day of the Operation a cup of tea, coffee, or broth may usually be given, with a cracker, unless the operation is to be performed early in the morning, in which case the patient is given no food at all. Some physicians allow a glass of milk on the day of the operation, but this is left entirely to the physician in charge.
After Operation a period of total abstinence from both food and water is necessary in order not to increase or induce nausea and vomiting. As soon as these symptoms subside, unless otherwise indicated, a certain amount of hot, cold, or carbonated water may be given. After this, albumen water may form the first nutrient administered. Milk, broth and fruit beverages follow the giving of albumen [Pg 321] water, after which the semi-solids, such as soft eggs, gelatin and milk soups, constitute the convalescent diet.
The Character of the Diet after the operation depends wholly upon the nature of the disease for which the operation was deemed necessary.
Diet After Gastro-enterostomy must be adjusted in order not to increase the acid content of the gastric organ, otherwise the delicate mucous linings of the intestines would be subjected to direct contact with materials which are irritating in character, owing to the fact that the mass passes through the new opening and has thus been deprived of the neutralizing agents found in the upper part of the intestinal tract. Under the circumstances milk, albumen water and fine cereal gruels are the best foods from which to formulate the diet after the necessary period of abstinence and fluid diet.
After Appendicitis, as a rule, no food is given for five days in cases where there has been a pus formation and the appendix gangrenous. Otherwise the routine treatment diet is given—water, then albumen water, followed by broth, milk and fruit beverages, fine cereal gruels, etc.
After Liver and Gall bladder Operations the character of the food must be considered. The fats are not well handled in such conditions and must be avoided as far as possible. Broths must be well skimmed and the milk fat free. Buttermilk and koumiss are probably the most suitable forms in which to give milk in these cases.
After Kidney Operations the work of elimination through kidney must be limited as far as possible in such cases. While it is impossible to rest the organ entirely, the giving of a proper diet under the circumstances will do much toward relieving the strain placed upon it. The protein foods, with the exception of milk, must be excluded from the diet. The régime practiced in acute nephritis gives the most satisfactory results.
(a) Write a diet order for patient operated upon for gastric ulcer.
(b) Formulate diet to be used after a gall bladder operation.
(c) Outline diet used after operation upon the kidney.
[106] “Some Gastro-intestinal Notes,” “The Medical Clinics of North America,” Vol. I, No. 1, pp. 192-193, by Thomas R. Brown, Johns Hopkins Hospital.
[109] “Diet in Health and Disease,” p. 555, by Friedenwald and Ruhräh.
The importance of the kidney functions has been clearly demonstrated. Urine, which is the fluid secreted by these organs, is one of the most important sources of information, not only as to the manner in which the body utilizes food in health, but as an index to certain pathological conditions, the processes of which are more or less indicated by the products excreted in the urine.
Function of the Kidneys.—The kidneys, as has already been stated, furnish a means by which the greater part of the waste products of the body are eliminated and in addition to this function they adjust the salts in the body. In an early chapter the function of the salts in food was explained. A certain amount of these substances, we know, is absolutely necessary to carry on the work in the body, but harm comes when a surplus is retained in excess of that which can be used in performing the various processes. Consequently the function of the kidneys to adjust the salts balance is by no means their least important one.
Elimination of the Toxins.—The toxic substances manufactured in the body and those resulting from bacterial action upon unabsorbed proteins are likewise eliminated in the urine. Thus it can be readily understood how necessary it is to keep these organs in good repair, that they may continue their work in an efficient manner.
It is necessary from a pathological standpoint for the nurse to understand the making of some of the simpler tests, that she may simplify her own work and that of the physician.
[Pg 324] Excretion of Carbon Dioxide and Water.—We have already spoken of the combinations of carbon and hydrogen compounds. These substances being oxidized, the carbon dioxide produced is eliminated by way of the lungs and the water is excreted partly by way of the lungs and skin, but chiefly by way of the kidneys.
Oxidation and Excretion of Nitrogenous Substances.—When the nitrogenous substances are oxidized, the used-up oxygen products are eliminated by the kidneys in the form of urea and more or less highly oxidized substances, such as ammonia and other salts, purin bases, and creatinin.
Uric Acid, the chief of the oxidation products of nucleoproteins, is produced in the body and from food, and is always in the urine, being one of its normal constituents. It is only when this substance is in excess in the urine that a pathological condition is indicated.
Examination of the Urine, then, is made for several different purposes: (1) to ascertain whether the kidneys are doing their work properly; (2) to find if the kidneys, or any part of the urinary tract, are either temporarily or permanently diseased; (3) to be able to judge from the various substances in the urine whether there is any abnormal process taking place in the body.
Tests.—In the examination of the urine for the above purposes, certain definite tests are made. These tests differentiate between the abnormal and the normal.
(1) Color.
(2) Amount in twenty-four hours.
(3) Odor.
(4) Specific gravity.
(5) Reaction, acid or alkaline.
(6) Albumen, indican, acetone bodies.
(7) Sugar.
[Pg 325]
(8) Microscopic examination for casts, cells, bacteria, etc.
The Color of normal urine varies, especially with the amount voided.
The variations in color range from the pale straw color of individuals who are voiding large quantities to the deep lemon or amber of those who void much less.
Pathological conditions are indicated to a certain extent by the color of the urine. Fevers heighten the color, small quantities of blood cause a smoky appearance, while bile changes the color of the urine to a greenish yellow.
Precipitates in the Urine.—When the urine has been allowed to stand for a time there is sometimes a brick-red deposit due to the precipitate of urates. This disappears upon heating and is not an evidence of any diseased condition.
Turbidity of Urine.—The turbidity of fresh urine then is the only kind which need be considered, since standing in the cold often brings about this condition, due to the growth of bacteria and deposits of both phosphates and urates.
Requirements in Testing Urine.—Urine to be tested should be fresh, and when it is not possible to make the examination at once it should be preserved with chloroform, or some other harmless preservative, until ready to use.
Bacteria in Urine.—The changes due to bacterial growth in the urine are manifested not only by the turbid character of the urine but also by the odor of ammonia.
The Amount of Urine.—The amount of urine voided in twenty-four hours varies with the individual in health as well as in disease. Many individuals void a great quantity during the twenty-four hours, chiefly because they drink a great quantity of water and other beverages. The average amount of urine passed in twenty-four hours by an [Pg 326] adult, or a child over eight years, is from 1000 to 2000 c.c. It represents from 60% to 70% of the amount of water ingested.
Collecting the Urine for Testing.—In measuring the urine it is necessary to begin collecting it after the bladder has been emptied the first thing in the morning. The patient should void just before the end of the twenty-four-hour period to be sure that the amount formed by the kidneys during this time is accounted for.
Diseases in Which Urine Is Diminished.—In certain diseases the amount of urine passed is diminished. This is found to be true in diarrhea and dysentery, when water is lost in the feces, in hemorrhage from any part of the body and from vomiting. It is likewise at times the case after abdominal operations and in nervous conditions, such as hysteria. The urine is diminished when there is an organic obstruction in the urinary tract and certain obstructive diseases of the heart, the lungs and the liver. In these latter cases, there is seen to be a retention or suppression of urine. In both acute and chronic nephritis and in certain fevers, the bladder at times must be emptied by means of a catheter. At other times, the condition is relieved as far as possible by limiting certain articles of food in the diet. At any rate, these points must be kept in mind when examining the urine.
Effect of Food upon the Urine.—The odor of normal urine is changed after eating certain foods, such as onions and asparagus. In disease, the odor of urine has a distinct value as a means of diagnosis; cystitis gives a foul odor, certain bacteria bringing about a decomposition in the urine and giving rise to an odor of putrefaction. In cases where there is a fistula connecting the bladder and rectum, the urine has a fecal odor.
Specific Gravity of Normal Urine.—The density or specific gravity of urine means the weight of any volume of [Pg 327] urine as compared with that of equal volume of distilled water. The specific gravity of normal urine varies from 1012 to 1024, that is, in a thousand cubic centimeters of urine there are found from 11 to 18 grams of solid material. In health it is necessary to know the amount of urine passed in twenty-four hours, to be able to judge whether the amount of solids is too high or too low.
Specific Gravity of Diabetic Urine.—In conditions like diabetes mellitus, where there is a wastage of sugar taking place in the body—that is, instead of being oxidized to carbon dioxide and water and glucose, the sugar is passing into the urine without completing its oxidation—the specific gravity rises in these cases to 1030 and over, showing distinctly that a greater amount of solid material is in the urine than is present normally. In chronic Bright’s disease and diabetes insipidus, the specific gravity is low.
Method of Determining Specific Gravity.—The specific gravity is determined by the use of an instrument known as a urinometer. The urine is poured into a tube and the urinometer is dropped into it. The different figures are marked upon the stem of the instrument and it is a simple matter to read off the figures of the level to which the stem sinks.
Reaction to Litmus.—In a former chapter it was stated that normal urine was, as a rule, acid, that is, it turns blue litmus red. Certain diseases render the urine alkaline. A like result is brought about upon the ingestion of sodium citrate or bicarbonate of soda. Urine which stands and becomes decomposed is alkaline in reaction, due to the bacterial action, with the production of ammonia.
Albumen in the Urine.—The presence of albumen in the urine is important, since normal urine does not contain this material in quantities sufficient to be recognized by ordinary tests. Hence in disease its presence is an indication of pathological processes taking place either in the [Pg 328] kidney or the urinary passages. The chief abnormal condition indicated by the presence of albumen in the urine is nephritis. Traces of albumen may occur in patients with fever or a heart weakness. Blood and pus in the urine likewise indicate albumen. When the nephritic condition is chronic, the kidneys themselves are diseased and the presence of albumen may be in traces only, while during the acute attack large quantities may be passed, but the urine will clear up after a time.
Benedict’s Qualitative Sugar Test.—Boil 5 c.c. of Benedict’s solution; add 8 drops of urine to be examined; hold the tube over the flame and allow to boil vigorously for 3 minutes and set aside to cool of itself. In the presence of sugar the entire solution will be filled with a precipitate which may be greenish, yellow, or red, according to the amount of sugar present. When the percentage of sugar is low (under 0.3%) the precipitate will form only upon the cooling of the solution. If there is no sugar present, the solution will either remain clear or show a slight turbidity, due to the precipitation of urates. The nurse must remember that to be useful the test must be made accurately. There must never be more than 10 drops of urine and 8 drops is the usual quantity. The boiling must be vigorous and the solution allowed to cool spontaneously.
Fehling’s Test for Sugar.—Fehling’s alkaline solution and Fehling’s copper solution must be kept in separate bottles until ready for use. Then about 2 c.c. of Fehling’s alkaline solution is poured into a test tube and 2 c.c. of Fehling’s copper solution is added. This is diluted with hydrant water to 8 c.c. Half of this quantity is sufficient for the test. The upper half of the solution is boiled over flame (gently agitated while heating), and while still boiling a few drops of urine are added. If no change appears, it is boiled again and a few drops more of urine are added. If a [Pg 329] reddish precipitate appears, sugar is present. The chemical reaction taking place is the reduction of copper sulphate to cuprous oxide. Sometimes a partial reduction occurs when urates are in excess, but once having seen the real reduction, a partial one cannot mislead the examiner.
Haines’s Test.—Pour 1 teaspoonful of Haines’s solution into a test tube and boil gently over a Bunsen burner; add 6 or 8 drops of urine and again heat to boiling. A yellow or red precipitate will indicate the presence of glucose.
Benedict’s Test.[110]—The simple quantitative test for sugar is the one devised by Benedict. This is simpler than the polariscopic examination and better suited for ordinary use.
Place 5 c.c. of Benedict’s quantitative solution in a small dish, add a little less than one-fourth of a teaspoonful of sodium carbonate and one-eighth of a teaspoonful of talcum and add 10 c.c. of water. Dilute urine (1 part urine to 9 parts water) except where the qualitative test showed a low percentage of sugar, that is, when the precipitate turns green instead of yellow, in which case it will be unnecessary to dilute the urine. Place dish over burner and bring the contents to a boil. Pour the urine into a graduated pipette. Now add the urine drop by drop to the contents in the dish until the blue color entirely disappears. This test should be done over several times to assure an accurate calculation. The calculation is made as follows: 5 c.c. of Benedict’s quantitative copper solution are reduced by 0.01 gram of glucose, consequently the quantity of undiluted urine required to reduce 5 c.c. Benedict’s solution contains 0.01 gram of glucose.
| 0.01 | × 100 = per cent. |
| x | |
| x = c.c. of undiluted urine. | |
Example; 1500 c.c. urine in 24 hours. 5 c.c. used to reduce (decolorized) Benedict’s solution.
| 0.01 | × 100 = 0.2 per cent. |
| 5 |
1500 × 0.002 (0.2 per cent.) = 3 grams of sugar in 24 hours.
Example: If the urine had been diluted with 9 parts water, in other words, 10 times, the calculation would be 5 c.c. diluted urine = 0.5 c.c. actual urine.
| 0.01 | × 100 = 2 per cent. |
| 0.5 |
1500 × 0.02 (2 per cent.) = 30 grams of sugar in 24 hours.
Hill and Eckman perform the Benedict’s quantitative test as follows:[111]
Measure with a pipette 25 c.c. Benedict’s solution into a porcelain dish, add 5 or 10 grams approximately of solid sodic carbonate, heat to boiling, and while boiling, run in urine until a white precipitate forms, then add urine more slowly until the last trace of blue disappears. The urine should be diluted so that not less than 10 c.c. will be required to amount of sugar which 25 c.c. of reagent is capable of oxidizing.
Calculation: 5 divided by number of cubic centimeters of urine run in equals per cent. of sugar.
Fermentation Test for Quantity of Sugar in Urine.—If the urine is 70° F. (room) temperature when the specific gravity is taken at both the beginning and end of the test, it will assure accuracy.
[Pg 331] To 100 c.c. of urine of known specific gravity, add one-fourth of fresh yeast cake thoroughly broken up. Mix thoroughly and set aside at a temperature between 85° and 95° F. for twenty-four hours, after which time test with Benedict’s or Fehling’s solutions. If reduction is obtained, it will be necessary to allow the fermentation to continue until it is complete. When no further reduction is obtained, the specific gravity is taken after the urine has reached a temperature of 76°. The difference in the specific gravity at the beginning and end of the test multiplied by 0.23 gives the percentage of sugar in the urine.
The following formulas represent the various solutions used in the above test:
| Gm. or c.c. | |
| Copper sulphate (pure crystals) | 17.3 |
| Sodium or potassium citrate | 173.0 |
| Sodium carbonate (anhydrous) | 100.0 |
| Distilled water to make | 1000.0 |
| (1) Copper Sulphate Solution: |
| 34.65 grams copper sulphate dissolved in water and sufficient water added to make 500 c.c. |
| (2) Alkaline Solution: |
| 125 grams potassium hydroxide. |
| 173 grams Rochelle salts dissolved in water q.s. to make 500 c.c. |
| Keep solution in separate bottles and mix in equal quantities when ready to use. |
| Copper sulphate (pure) | 30 grams |
| (dissolved in ½ oz. (15 c.c.) distilled water) | |
| [Pg 332] Add ½ oz. pure glycerin, mix thoroughly, and add 5 oz. liquor potassæ. | |
| Copper sulphate (pure crystals) | 18 grams |
| Sodium carbonate (crystallized) (or 100 grams of anhydrous salt) | 200 grams |
| Sodium or potassium citrate | 200 grams |
| Potassium sulphocyanide | 125 grams |
| 5% solution of potassium ferrocyanide | 5 c.c. |
| Distilled water to make total volume of 1000 c.c. | |
Dissolve the carbonate, citrate, and sulphocyanide with the aid of heat and enough water to make 800 c.c. of mixture. (Filter, if necessary.) Weigh exactly the copper sulphate crystals and dissolve in 100 c.c. of water, now add it to the first solution; stirring constantly. Add the ferrocyanide solution; cool and dilute to exactly 1 liter.
50 mg. (0.050 gm.) of sugar will reduce 25 c.c. of the above solution.
Gerhardt’s Ferric Chloride Reaction for Diacetic Acid.—To 10 c.c. of fresh urine, add carefully a few drops at a time of undiluted aqueous solution of ferric chloride U.S.P. A precipitate of ferric phosphates first forms, but upon the addition of a few more drops of the same solution it is dissolved. A Burgundy red (red wine) color is obtained in the presence of diacetic acid. The depth of this color is indicative of the quantity of acid present. Joslin[112] records the intensity of the reaction as follows, +, ++, +++, or ++++.
According to Joslin, it must be remembered that similar reaction is obtained in the urine of individuals taking salicylates, antipyrin, cyanates, or acetates, but it is a simple process to differentiate between the color produced as a [Pg 333] result of diacetic acid and that produced by the above-mentioned drugs. If the solution is boiled for two minutes, the color from diacetic acid will disappear, owing to the unstableness of that substance, while that from the drugs will remain unchanged.
Test for Acetone.—Pour 5 c.c. of urine to be tested into a test tube, add a crystal of sodium nitroprusside, acidify with glacial acetic acid, shake well, and then make alkaline with ammonium hydrate. The presence of acetone is indicated by a purple color.
The heat test[113] is the simplest. This consists of first filtering the urine through filter paper, then pouring some of the clear urine into a test tube, holding the test tube in a flame so that only the upper layer boils, then adding a few drops of 2% solution of acetic acid and boiling again. If there is albumen present, a very faint, or a heavy cloudiness (precipitate of coagulated albumen) forms on boiling and persists or becomes heavier on the addition of a few drops of dilute acetic acid (2%) and boiling again. If a precipitate occurs at the first boiling, but clears up again entirely on adding acetic acid, it is not albumen but harmless phosphates or carbonates.
Into a test tube pour a few drops of nitric acid, filter the urine and allow a small quantity of it to trickle from a pipette down the side of a test tube until it comes in contact with the acid. If albumen is present a distinctly formed white ring is seen at the zone of contact.
This material is found in cases of obstinate constipation and in other intestinal disturbances where the passage of [Pg 334] the food mass in the small intestines is delayed and the putrefactive bacteria exert their activities upon the unabsorbed protein.
Test.—Mix equal quantities of urine and fresh hydrochloric acid and add drop by drop fresh concentrated solution of chloride of lime (5 to 1,000). Indican is indicated by the appearance of a blue color.
Urinalysis represents one of the most important means for determining the health of an individual, since it is the urine that shows those substances produced in the body as a result of the breaking down of the body tissues and protein foods.
Composition of Normal Urine must be familiar to the nurse in order that she may recognize any change taking place in the urine of her patient which may indicate pathological conditions in the body.
The Specific Gravity of urine is one of the points by means of which the presence of certain substances more or less abnormal in character is determined.
Other Points, such as color, odor, quantity, reaction, and chemical composition, likewise show any deviation from the normal in the individual.
Urine Tests are necessary to determine the composition of the secretion. The character of these tests and the methods used in making them form an essential part in the training of the nurse.
Tests for the presence of albumen, sugar, and possibly indican in the urine, should be made by the nurse. The latter substance represents the extent of putrefaction taking place in the body and for this reason should be included in the urine tests.
Collecting the Urine for testing is important. The amount includes all that has been voided throughout the [Pg 335] entire twenty-four hours beginning after the bladder has been emptied on the first morning and ending after the first specimen has been voided on the morning of the second day.
Preserving the Urine for testing is usually necessary, especially during the warm weather. The specimens should be collected in a wide-mouthed sterile glass jar. This should be kept in a cold place. Some harmless preservative such as chloroform should be added to assure its keeping.
(a) Outline tests used in urinalysis; state when they are used.
(b) List the equipment needed for making the simple tests.
(c) Make tests in laboratory and list results in note-book.
[110] “Treatment of Diabetes Mellitus,” pp. 182-183, by Joslin.
[111] “Starvation (Allen) Treatment for Diabetes Mellitus,” by Hill and Eckman.
[112] “Treatment of Diabetes Mellitus,” p. 186, by Joslin.
[113] “Chemistry for Nurses,” by Reuben Ottenburg.
Nephritis is a disease of the kidneys, in which changes occur in the tissues of the organs themselves; these changes may be caused by inflammation of the kidneys and renal passages brought on as results of the retention of certain poisonous substances in the blood, or from the action of specific bacteria. The disease may be acute or chronic in form and develop as a result of prolonged exposure to cold and wet, of tonsillitis, scarlet fever, typhoid fever, and to a less extent of malaria, syphilis, pregnancy, and tuberculosis, as well as from the effects of certain irritating drugs, such as cantharides and turpentine.
Directing the Treatment.—In any case the treatment must be directed toward the relief of the acute symptoms in the beginning and followed up by a general treatment which will tend to strengthen and relieve the overtaxed organs and to increase their power to functionate normally.
Causes and Effects.—In acute nephritis, the chief symptoms are uremia, and edema; the urine is materially diminished in quantity and at times suppressed; it is often found to be rich in albumen and containing hyaline and blood casts, red and white blood cells, and various pigments.
In chronic nephritis, which may be the result of an acute attack, or as a sequel of other diseases already mentioned, there is seen to be a progressive loss of flesh and strength, marked anemia, gastro-intestinal disturbances, increased blood tension and edema, the latter especially in the face on arising in the morning. Uremia may develop at any time.
[Pg 337] Limiting the Work of the Kidneys.—In both acute and chronic nephritis, great effort must be put forth to relieve the tax upon the kidneys and to stimulate their functioning power.
In other diseases, in which definite organs are involved, the treatment consists chiefly of resting the affected parts (1) by starvation, (2) by deflecting the work to other organs when it is possible, chiefly by changing the diet until the disturbance is overcome. This is generally effectual in most cases, as has been specially demonstrated in the treatment of gastro-intestinal diseases.
Problems to Be Considered.—But in nephritis, there are other problems to consider, which make it impossible to institute such a treatment as will effect a perfect rest of the renal organs. The kidneys represent the chief source whereby the waste products of the body are eliminated. This waste consists not only of the end-products of the nitrogenous foods ingested, but also the end-products of tissue metabolism, which is the inevitable result of the wear and tear of life. Hence, when the functions of the kidneys are disturbed, these products, often toxic in character, are retained instead of excreted. Thus instead of forming normal constituents of the urine they find their way into the general circulation, exerting a damaging effect upon the tissues, especially of the kidneys with which they are brought into such direct contact.
Substances Difficult of Excretion.—It has been proved that the kidneys in nephritis find it difficult to excrete certain substances, namely, urea, water, salts, and the purin bodies. Many authorities claim that the uremia manifested in acute nephritis is the result of the retention of end-products of the protein metabolism already mentioned and that the edema is due to a like retention of water and salts. The greatly diminished quantity of urine voided during the acute attack would seem to prove this theory. Martin [Pg 338] Fisher,[114] however, claims the condition to be due to an acidulation of the tissues with a consequent osmosis of water, and directs his treatment to overcome this condition, not by restricting the quantity of water and salt, as is generally practised, but by injecting a saline solution into the body in large quantities with the effect of increasing the flow of urine by concentrating the salt content of the blood and therefore its osmotic power. The fluids are withdrawn from the tissues, thus adding fluidity to the blood stream, which in turn flushes the kidneys, ridding them of the poisons which interfere with their normal functioning.
Adjusting the Diet.—The uremia and edema must be relieved. Since it is an undisputed fact, in the majority of cases, that good results from the regulating of the diet so as to minimize as far as possible the work of the kidneys, the various diet cures will be included here.
Milk Cure.—Milk, as a rule, forms a basis of most of the nephritic diets chiefly because of its low salt and protein content and on account of its non-toxic end-products.
The percentage of water in milk is likewise known and for this reason the fluid content of a milk diet can be easily calculated. However, it is also true that the greatest drawback to a diet consisting solely of milk is the large amount of water therein compared with its nutrient value.
Resting the Kidneys.—During the acute stage of nephritis the kidneys are given as much rest as possible by eliminating all food and restricting the amount of water entering the body. The thirst is relieved by small sips of plain or carbonated water or by ice pellets held in the mouth, or, as is sometimes necessary, by injections of water into the rectum.
Adjusting the Fluids.—The amount of fluid, however, [Pg 339] must be adjusted to meet the condition of the patient, taking into consideration the amount of urine voided and the uremic symptoms manifested. If the urine is not suppressed the amount of water taken may be slightly in excess of the urine voided, thus promoting diuresis. In many cases an excellent diuretic drink consisting of one pint of water and one teaspoonful of cream of tartar with a half a lemon and perhaps a little sugar, serves the purpose of relieving the thirst, which is at times acute during this period.
The extent of the starvation treatment must depend upon the patient himself. As a rule, however, it is not carried out longer than two days, after which milk may be substituted, allowing from twenty to thirty ounces per day, which is as much fluid as an ordinary nephritic patient can handle.
The regulation nephritic diet, which is bland in character, contains nothing that will tend to increase the irritation and inflammation of the kidneys, and furnishes a certain amount of nourishment when the symptoms of the disease warrant the giving of any food other than milk.
The following diets used in cases of high urea or severe hypertension:
| Protein | Carbohydrates | Fats | ||
| Grams | Grams | Grams | ||
| Breakfast: | 6.7 | 160 | 51 | |
| Cooked Farina | (100 grams) | Total calories for day, 1192 | ||
| Butter | (20 grams) | |||
| Fruit | (100 grams) | |||
| Lactose | (30 grams) | |||
| 200 grams of fruit juice served between meals | ||||
| Dinner: | ||||
| Asparagus | (100 grams) | |||
| Butter | (20 grams) | |||
| Fruit | (100 grams) | |||
| Lactose | (30 grams) | |||
| [Pg 340]Supper: | ||||
| Carrots | (100 grams) | |||
| Fruit | (100 grams) | |||
| Butter | (20 grams) | |||
| Lactose | (30 grams) | |||
| Protein | Carbohydrates | Fats | ||
| Grams | Grams | Grams | ||
| Breakfast: | ||||
| Protein-free cookies[116] | (5) | |||
| Fruit juice | (100 grams) | 0 | 166.5 | 39 |
| Lactose | (15 grams) | |||
| Dinner: | ||||
| Protein-free cookies | (5) | Total calories, 1045 | ||
| Fruit juice | (100 grams) | |||
| Lactose | (15 grams) | |||
| Supper: | Each cookie weighs 10 grams | |||
| Protein-free cookies | (5) | |||
| Fruit juice | (100 grams) | |||
| Lactose | (15 grams) | |||
Doctors Chase and Rose advise farina used more frequently than oatmeal, and the plain cream soup, rice or potato, more often than soups made of celery or asparagus (the latter used to break the monotony). They also advise the more frequent use of green string beans and asparagus in preference to other vegetables.
Elimination of Salt.—In many cases of nephritis, especially those belonging to the parenchymatous type, the kidneys manifest a difficulty in eliminating salt, and instead of excreting the normal quantity, find it impossible to eliminate more than two or three grams or less a day. The retained salts pass into the fluids of the tissues, giving rise to or increasing the already existing edema. Tests[117] have been devised to find the extent of the kidney function to excrete salt. The following diets are among those commonly used:[118]
[Pg 341] 3 liters of milk (this contains 5 gm. sodium chloride and 100 gm. protein)
or
Strauss Diet, consisting of ¾ liter milk, 4 eggs, 150 gm. bread, and enough fruit and fruit juice, tea and sugar to make it palatable. (This diet contains about 3 gm. of salt.)
If the kidneys are able to excrete the amount of salt contained in these diets, salt may be added in quantities of from 5 to 10 grams.
Salt-poor Diets.—When the kidneys are unable to eliminate the normal amount of salt, some of the salt-poor diets should be advised. Coleman claims,[119] however, that these diets have not fulfilled the promises held out by them. Coleman groups the salt-poor diets under three headings:
(1) The strict salt-poor diet, of which Widal’s diet is an example.
(2) The medium strict salt-poor diet, allowing from 2.5 to 5 grams of salt a day. Under this heading the milk diet was placed, in which 2 to 3 grams of salt is served a day at table.
(3) The moderate salt-poor diet, in which from 5 to 10 grams of salt are allowed each day. In using this diet it is not necessary to prepare a special menu for the patient, but take precautions to leave the salt shaker off the tray and exclude bacon, ham, and other salty foods from the dietary.
Limiting the Amount of Food.—It must be kept in mind that the nephritic condition makes it imperative to fall below rather than exceed the food requirements of the individual.
| Salt-free bread | 200 gm. |
| Meat (beef, chicken, or mutton) | 200 gm. |
| Vegetables (beans or rice), salt-free | 250 gm. |
| Butter, salt-free | 50 gm. |
| Sugar | 40 gm. |
[Pg 342] Contains 60 grams of protein, 1 to 2 grams of NaCl, and furnishes approximately 1500 calories.
Strouse and Perry arranged a dietary from the above diet as follows:
8 A.M. Bread, 60 grams; lamb chop, 50 grams; butter, 10 grams; rice, 100 grams; sugar, 40 grams.
12 M. Bread, 60 grams; roast beef, 100 grams; butter, 20 grams; beans, 150 grams.
5 P.M. Bread, 80 grams; butter, 20 grams; chicken, 50 grams.
Milk, 1500 to 2000 c.c., white salt-free bread, 400 to 500 grams; salt-free butter, 40 grams; eggs, 4 to 6. This diet contains from 5 to 6 grams of salt.
Karell has devised the milk cure, which is used possibly more than any other diet. It not only furnishes a dietary régime, which is used in nephritis, but it is likewise advocated in organic diseases of the heart and blood vessels.
Methods of Administering the Karell Cure.—The cure is begun by giving from 3 to 6 ounces of milk three or four times a day. Karell makes a point of using small quantities to begin with and having the milk skimmed. The milk is given at regular intervals, is warmed in winter and given at room temperature in the summer. It may be given plain or diluted with limewater. After a week if the stools remain solid, the daily allowance of milk is increased to two quarts. Constipation is an indication of the agreement of this diet and the patient’s utilization of the milk. If, however, he manifests gastro-intestinal disturbances, resulting in diarrhea, the amount must be temporarily reduced. Karell advocates boiling the milk and relieving the constipation with enemas or mild laxatives. The addition of small quantities of coffee to the morning portion of milk, or of stewed [Pg 343] prunes or a baked apple to the afternoon feeding, also tends to overcome the condition.
Thirst.—The extreme thirst may be relieved by adding plain water, limewater, or seltzer to the feedings.
If during the second or third week of the cure the hunger becomes too great for the patient to endure, a small piece of herring or stale bread may be given.
Once a day a milk soup thickened with a cereal may be given. The above diet is carried out from five to six weeks, after which the patient is gradually returned to a normal diet. Milk, however, should still constitute an important part of the diet. The Karell cure is modified more or less to meet the condition of the patient, the amount of milk administered in some cases being more and in others considerably less than mentioned in the above régime.
Limiting the Proteins.—The extent of the damage caused by the end-products of protein metabolism cannot be easily estimated, but it is wise not to err on the side of an over-supply, since the retaining of these materials in the body gives rise to a certain type of intoxication (uremic poisoning).
Relative Toxicity of the Animal Proteins.—The difference between the various animal proteins as to their relative toxicity has been the subject of much discussion. As far as their nutrient value is concerned, they are practically the same, that is, the protein of beef and the protein of chicken show very similar analyses. The beef contains, however, more extractives, which we know are high in purins. These substances have proven detrimental to the welfare of a nephritic patient.
Selection and Preparation of Foods.—For this reason the so-called red meat is sometimes boiled instead of roasted, as the latter mode of preparation increases the formation of purins on the brown outer surfaces of the meat. Chicken and fish contain less purin bases and for this reason are often [Pg 344] included in the diet when beefsteak and lamb chops are excluded. Meat soups and broths contain little nutrient value, consisting as they do chiefly of water, salt, and extractives, all of which are looked upon with disfavor, and classed with the offending articles of food in the nephritic diet. Cream soups, except bean or pea soup,[121] may be given in moderation. They are non-toxic in character and of high nutrient value, furnishing a valuable addition to the diet when the gastro-intestinal symptoms permit of such addition.
Advisable Foods.—The following foods are used in the formation of diet for an advanced convalescent nephritic patient when not otherwise contraindicated:
Cereals, potatoes, rice, green vegetables and salads, fruits, fresh and stewed, ham, bacon, or beef once or twice a week, chicken, lamb, or mutton[123] several times a week, simple desserts, such as junket, prune or fig whip, orange, lemon, grape, pineapple or apricot gelatin, bread, rice or tapioca pudding, plain vanilla ice cream.[124]
Foods to Be Avoided.—The following foods are avoided except the meats, which must be given not more than once to three times a week, as directed by physician:
Meat broths, especially those made from commercial meat extracts, bouillon cubes, etc.
Strong tea or coffee.
Alcoholic beverages, unless especially prescribed by the physician.
Liver, kidney, sweetbreads.[125]
[Pg 345] Meat croquettes and other made dishes.
Rich sauces or gravies.
Condiments and spices of all sorts.
Rich pastries.
The salt must be limited and water and other fluids restricted.
Sample Diet Sheets.—The following menus[126] formulated from the above diet list are suggested:
No. 1.—8 A.M. Sliced oranges, cream of wheat with cream, buttered toast, cocoa.
10:30 A.M. 6 ounces of milk with crackers.
12:30 P.M. Cream of spinach soup, rice, string beans, orange gelatin, bread and butter.
3 P.M. 6 ounces of buttermilk with crackers.
6 P.M. Cereal and cream, baked potato, apple sauce, cocoa, bread and butter.
No. 2.—8 A.M. Stewed prunes, wheatena and cream, milk or dry toast with butter, cocoa.
10:30 A.M. 6 ounces of malted milk with crackers or 1 slice of zwieback.
12:30 P.M. Cream of corn soup, mashed potatoes, beet tops or mustard greens, lettuce salad, dressing made with lemon juice and olive oil, rice pudding.
3 P.M. 6 ounces of orange or grape juice with crackers.
6 P.M. Cream toast, sliced peaches, cocoa.
No. 3.—8 A.M. Half a grapefruit, farina and cream, toast and butter, cocoa.
10:30 A.M. 6 ounces of buttermilk with crackers.
12:30 P.M. Cream of tomato soup, creamed potatoes, buttered beets, celery salad, apple tapioca pudding, bread and butter.
3 P.M. 6 ounces of milk with crackers.
6 P.M. Ralston’s Health Food with cream, baked potato, tomato salad, toast and butter, cocoa.
[Pg 346] No. 4.—8 A.M. Stewed prunes, grits and cream, toast and butter, cocoa.
10:30 A.M. 6 ounces of malted milk with crackers.
12:30 P.M. Cream of asparagus soup, creamed cauliflower, boiled rice, lettuce salad, bread and butter, pineapple gelatin.
3 P.M. 6 ounces of orange juice with crackers or zwieback.
6 P.M. Creamed toast, escalloped potatoes, fruit salad, toast, cocoa, and cocoa junket.
Chronic nephritis may develop as a sequel to an acute attack, and an individual suffering from chronic nephritis may at any time develop acute symptoms. In any case the dietetic treatment would necessarily have to be made to cover the existing symptoms.
Dietetic Treatment.—In cases where the patient has entirely recovered from uremia but still manifests symptoms of water and salt retention, the diet would be naturally directed to cover the latter, at the same time taking care not to strain the weakened functions by giving more food than could be readily handled. The water and salts still have to be restricted, but a certain amount of fat and carbohydrate with small additions of nitrogenous food materials may be added from time to time as the kidneys show improvement. It must be borne in mind, however, that at this time it is very easy to overtax the renal organs and it is safer to err on the side of under rather than over feeding.
The logical treatment, therefore, consists of utilizing the improved functions while those still failing to react are getting further rest.
Adjusting the Proteins in Diet.—If the individual shows a definite anemia, as is often the case after acute attacks, either as a result of the disease itself or the [Pg 347] necessarily low diet, which the acute symptoms of uremia and edema made necessary, other measures are necessary to bring the body back to a normal condition. It has been found that in these cases where there has been no permanent damage to the renal organs, but merely a temporary impairment of the functioning power, the treatment must be, first, a rest to the affected parts; second, the temporary restriction of all articles of food which impose a tax on the kidneys to eliminate; the third, the gradual return to normal diet as the acute symptoms decrease and the function of the kidneys no longer shows impairment. Such a case is cited by Strouse and Perry[127] as occurring in the Michael Reese Hospital. Mr. X. recovered from the acute stage of nephritis and all signs of edema and uremia disappeared; the man was kept on a low salt and low protein diet for a long time. His urine was clearing up, but he did not feel up to standard and remained anemic. Thinking in all probability that his symptoms were due to a low protein diet, meat was slowly added to his dietary until he was receiving 60 grams of protein a day. There was an immediate general improvement in his condition with no increased renal disturbance. It is an obvious fact that chronic nephritis, like any other chronic condition, requires a different method of treatment from that practised to relieve the acute stage. The very fact that it is chronic proves that the strenuous methods are neither necessary nor wise.
Testing the Kidney Functions.—The authorities of to-day endeavor to ascertain the extent of the damage to the renal organ by testing its functioning power. These renal function tests have been the subject of much interest and investigation. Probably the ones most commonly employed are those devised by Hedinger and Schlayer[128] and adapted for use in the Johns Hopkins Hospital by Mosenthal.
[Pg 348] Diets Used in Tests.—The diet employed in making these tests consists of different amounts of certain substances known to be diuretic in character. This diet is rigidly adhered to and a careful analysis of the urine passed, the total quantity and specific gravity of each specimen made and in this way the various functions of the kidneys and the impairment thereof are tested. Thus an intelligent adjustment of the diet may be made.
Renal Functional Tests.—The following schedule is used by Mosenthal, of the Johns Hopkins Hospital, in making what is known as the “Two-Hour Test for Renal Function”:
| For | Date |
All foods to be salt-free from the diet kitchen, salt for each meal will be furnished in weighed amounts.[130]
All foods or fluids not taken must be weighed or measured after each meal and charted in spaces below. Allow no food or fluid at any time except at meal times.
Note any mishaps or irregularities that occur in giving the diet or collecting the specimens.
| Breakfast 8 A.M. | Boiled oatmeal | 100 grams | |
| Sugar 1 to 2 teaspoonfuls | |||
| Milk | 30 c.c. | ||
| 2 slices of bread | 30 grams each | ||
| Butter | 20 grams | ||
| Coffee 160 c.c. | |||
| Sugar 1 teaspoonful | 200 c.c. | ||
| Milk 40 c.c. | |||
| [Pg 349]Dinner—Noon | Meat soup | 180 c.c. | |
| Beefsteak | 100 grams | ||
| Potatoes, boiled, mashed or baked | 130 grams | ||
| Green vegetables as desired | |||
| 2 slices bread—each | 30 grams | ||
| Butter | 20 grams | ||
| Tea, 180 c.c. | |||
| Sugar, 1 tsp. | 200 c.c. | ||
| Milk, 20 c.c. | |||
| Water | 250 c.c. | ||
| Pudding, tapioca or rice | 110 grams | ||
| Supper 5 P.M. | 2 eggs cooked any style | ||
| 2 slices of toast | 30 grams each | ||
| Butter | 20 grams | ||
| Tea, 180 c.c. | |||
| Sugar, 1 tsp. | 200 c.c. | ||
| Milk, 20 c.c. | |||
| Fruit, stewed or fresh | 1 portion | ||
| Water | 300 c.c. | ||
8 A.M. No food or fluid is to be given during the night or until 8 o’clock next morning (after voiding) when the regular diet is resumed.
Patient is to empty bladder at 8 A.M. and at the end of each period as indicated below. The specimens are to be collected for the following periods in properly labeled bottles:
8 A.M. to 10 A.M.; 10 A.M. to 12 Noon; 12 Noon to 2 P.M.; 2 P.M. to 4 P.M.; 4 P.M. to 6 P.M.; 6 P.M. to 8 P.M.; 8 P.M. to 8 A.M.
Chart Used in Johns Hopkins Hospital.—The following chart is inserted here to show the method used in the Johns Hopkins Hospital for carrying out the Two-hour Renal Test:
| Time of Day | Urine | NaCl | Nitrogen | |||
| C.C. | Specific Gravity | Per cent | Grams | Per cent | Grams | |
| 8 A.M.-10 A.M. | ||||||
| 10 A.M.-12 Noon | ||||||
| 12 Noon-2 P.M. | ||||||
| 2 P.M.-4 P.M. | ||||||
| 4 P.M.-6 P.M. | ||||||
| 6 P.M.-8 P.M. | ||||||
| 8 P.M.-8 A.M. | ||||||
| Total day | ||||||
| Night, 8 P.M. to 8 A.M. | ||||||
| Total 24 hours | ||||||
| Intake of fluid | ||||||
| NaCl | ||||||
Urine to be collected punctually every two hours and kept in the ice-box, every specimen having twenty drops of tutuol added to insure preservation.
Another modification of the Hedinger-Schlayer diet is used in the Peter Bent Brigham Hospital,[131] Boston, Massachusetts, as follows:
| 7 A.M. | Coffee, milk, sugar, toast, and butter. |
| 10 A.M. | Milk, toast, and butter. |
| 12:30 P.M. | Bouillon, broiled steak, butter, mashed potatoes, toast, coffee, milk, sugar. |
| 4 P.M. | Tea, milk, sugar, crackers. |
| 7 P.M. | Soft egg, blanc-mange (1 egg, sugar, cornstarch, and milk) and cream. Amounts sufficient to give 2500 calories, 1500 c.c. fluid, 76 grams of protein, 127 grams of fat, 245 grams of carbohydrate, and from 5 to 8 grams of sodium chloride. |
[Pg 351] On two days previous to the test the patient usually had a diet containing 2000 calories, 75 grams of protein, 4 grams of sodium chloride.
The test diet is a mixed diet containing known amounts of water, nitrogen, and chloride, together with the food diuretics (purins, salt, and water), as can be seen. The diet is divided into unequal portions containing known but varying amounts of fluid, nitrogen, and salt. Two-hour specimens are collected from 7 A.M. to 9 P.M., and one night specimen is obtained containing all the urine passed between 9 P.M. and 7 A.M. Each specimen is analyzed for volume, specific gravity, total nitrogen, nitrogen concentration, total chloride, and chloride concentration.
Purpose of Tests.—The purpose of the test is to find out to what extent and in what manner the diseased kidney under stimulation by the various diuretics taken in the food reacts in putting out the varying amounts of salt.
Dr. O’Hara likewise describes another test known as The Added Urea and Salt Test, which was first described by von Monakow and also carried out in the Peter Bent Brigham Hospital. The method used was as follows:
Patient is given 75 grams of protein, 4 grams of sodium chloride, and 1500 c.c. of water, with a caloric value of from 2000 to 2200 calories. After the output of fluid, salt and nitrogen reaches an equilibrium on this diet on one day 10 grams of additional salt is given and several days later the patient receives 20 grams of urea. This order may be reversed. The daily output of urine, salt, and nitrogen is determined and charted. After the salt and nitrogen is added to the diet in normal individuals, their excretion after forty-eight hours returns to its previous level. In diseased kidneys this may not be the case.
Value of Tests.—Thus it is seen that in these tests for [Pg 352] kidney functions, an effort is made to determine the extent of damage wrought by the disease upon the renal organs and the manner in which they react under definite circumstances. However, it is not so simple as it would seem to formulate a dietary based on the findings resulting from the renal tests. Notwithstanding this, these tests are coming more and more into use, both in hospitals and private practice, and a nurse must understand just how they are carried out, and must realize that unless her part is performed with absolute accuracy the entire value of the test will be obliterated. Too much stress cannot be laid upon this phase of the test, if it is to be of any value whatsoever in determining the condition of a diseased kidney.
This form of nephritis is more insidious in character, developing more slowly and manifesting different characteristics, than those seen in some of the other types already mentioned. The condition is, as a rule, associated with heart symptoms and high blood pressure. The blood shows an increase in urea and other end-products of protein metabolism, whereas there is no manifest change in the metabolism of salt or water. The great increase in volume of urine voided would show an inability on the part of the kidneys to eliminate a highly concentrated urine. This hypothesis is further demonstrated in the urine tests.
Urinalysis.—Upon analysis the urine in these cases shows less albumen and fewer casts than found in other types of nephritis. The disease is manifested by slight headache, gastric disturbances, and a frequent desire to urinate.
Dietetic Treatment.—The treatment here depends upon the extent of the impairment of the functions of the kidney. If the damage is not extensive and the diagnosis [Pg 353] has been sufficiently early to insure prompt improvement upon treatment, the diet is so directed as to prevent the occurrence of any of the acute symptoms. The patient is warned against overeating and drinking, over-exercise and nervous excitement. When it is possible, a change to a warm, dry climate is advisable with more rest and sleep and less work and worry. He is advised to eat less at meals and if hungry to eat a light lunch of milk or buttermilk with crackers in the mid-morning. The same dietary precautions must be taken in these disturbances as in other nephritic conditions, keeping always in mind the fact that the kidneys are the chief organs of excretion in the body, and through them must pass the majority of all end-products of nitrogen metabolism.
Limiting the Nitrogen.—The nitrogenous foods cannot be eliminated entirely, especially if, as is often the case, the individual suffers from chronic nephritis and is up and about attending to business; but they can be judiciously regulated in the diet. All such foods as fried foods, rich pastries, rich sauces and gravy, spices of all kinds, tea and coffee, celery and asparagus, must be avoided.
Limiting the Fluids.—von Noorden limits the amount of fluid to 1¼ liters per day. This does not include the water content of the various foodstuffs. He advises a period of observation to determine the amount best suited to the condition of the patient and reducing this amount from 250 to 150 c.c. a day until the desired quantity is reached. He advises a drinking day once a week, allowing the patient to drink as much water as he likes.
Development of Uremia.—Whenever evidences of uremia appear the treatment must be changed to meet the condition. It is necessarily more strenuous than that used ordinarily in the chronic nephritis. If the uremia becomes positive, then the treatment laid down for acute nephritis [Pg 354] already described must be at once instituted. The patient must be put to bed at once and every effort made to assist the body in getting rid of the causes.
In certain cases of nephritis, in which uremic poisoning is due to the retention of the end-products of nitrogen metabolism, or to the toxins formed as a result of the tissue changes due to the disease, the water then instead of being restricted in the dietary is greatly increased to encourage a free diuresis with a consequent washing out of the accumulated poison. Certain authorities recommend a strict milk and water diet, as has already been described in the beginning of the chapter. A light or soft diet is advised until the condition improves, resting the renal organs as far as possible. This diet may consist of fruit juices, strained cereals with cream, cocoa, milk, buttermilk, toast, butter, strained apple sauce, cream soups, except those made with beans or peas. The above diet is gradually increased by adding a mashed or baked potato, well-cooked green vegetables, stewed or raw fruit, rice and tapioca pudding, and chocolate blanc-mange.
Selection and Preparation of Food.—The preparation of foods for the nephritic differs in certain particulars from that used in other pathological conditions, namely, the restriction of certain food constituents; dishes made with meat and eggs are cut out of the diet, and salt is used as sparingly as possible, when it is used at all. The nurse must weigh or measure out the maximum quantity allowed and divide this in portions for each feeding, measuring carefully any that is not used and charting it. In this way it is possible to increase or decrease the amount according to the symptoms of the individual. The water content of the various foods comprising the diet is, as a rule, not considered, but it is necessary to adhere strictly to the orders of the physician and to curtail the beverages, water, tea, coffee, [Pg 355] etc., until the amount conforms to that laid down in the dietary.
The nitrogenous foods, with the exception of milk, are as a rule eliminated from the nephritic diet. The nurse must study the tables and learn which food materials come under this head. It may seem difficult to prepare diet for the sick without eggs, but it is possible and at times obligatory.
Combating Anemia.—In chronic (ambulatory) nephritis the anemia must be reckoned with. It is not safe to upset the nitrogen equilibrium of the body, but it has been proved that this may be maintained on as little as 30 or 40 grams of protein a day. This will be seen not to be difficult to obtain when milk forms an important part of the diet. The wheat and oat cereals, as well as the bread, contain protein, and a judicious use of these foods will enable the nurse to give her patient the necessary quantity to offset, in a measure, the anemia which is at times most troublesome.
Advice to Patient.—One important point must be observed by the nurse and impressed upon the patient when he leaves her care. This is moderation in the amount of food eaten. The kidneys must never be overtaxed, even with foods which in themselves seem harmless. As danger lies in overindulgence, this point cannot be too strongly emphasized.
Advice to the Nurse.—The use of the formulas included in this text is left to the discretion of the nurse. In those calling for seasoning, such as pepper, mustard, etc., the condiments must be omitted. A small amount of celery salt may be substituted in certain instances if the dish is unpalatable without something of the kind. In cases where the salt is restricted the dishes are prepared as directed, with the exception of the salt. The recipes calling for eggs and meat are not to be used unless directed by the physician. Cornstarch, sago, and tapioca may be used instead of gelatin. [Pg 356] The following menus may be used as guides in selecting foods to prepare for the nephritic patient after the rigid régime is to a certain extent relaxed:
Breakfast
Grapefruit, orange, prunes, pears, peaches, or strawberries.
Cereals: cream of wheat, farina, Pettijohn’s, Ralston’s, hominy, grits, and oatmeal with cream.
Toast, buttered or creamed.
Cocoa, tea, or coffee, as directed by the physician.
Dinner
Milk or cream soup, well-cooked green vegetables with butter or cream sauce.
Potatoes, white or sweet, baked, mashed, or boiled, with butter, bread or rolls.
Stewed tomatoes, rice.
Salads: lettuce, tomato, romaine, chicory, or fruit salad, with a dressing of oil and lemon, or cream and lemon.
Simple desserts: junkets, cornstarch, sago or tapioca pudding, baked bananas, rice pudding, apple tapioca, orange tapioca, and ice cream.
Beverages: cocoa or tea, as directed by the physician.
Supper
Cereals and cream.
Baked or escalloped potatoes.
Baked or stewed apples.
Salads, excepting those made with meat or eggs.
Junket, raw or stewed fruit.
[Pg 357]
Toast or rolls with butter.
Cocoa.
Meat, fish or poultry once a day.[132]
Breakfast
Stewed or fresh fruit.
Cereals with cream.
Toast with butter.
Cocoa, milk, or tea.
Dinner
Cream soups.
Boiled chicken or fish.
Potatoes, white or sweet.
Green vegetables.
Salads, except with meat or eggs.
Simple desserts.
Rolls or bread and butter.
Milk or buttermilk.
Supper
Cereals or rice with cream or butter.
Baked or escalloped potatoes.
Stewed or escalloped carrots.
Salads, except those made with meat or eggs.
Fresh or canned pears, cherries, or pineapple.
Bread pudding, junkets, or cornstarch blanc-mange.
Bread, rolls, or toast, with butter.
Cocoa, milk, tea, or buttermilk.
According to Leva
Analysis marked thus: * from Atwater & Bryant.
| Per Cent. of Sodium Chloride in Raw Material |
|
| Meats | |
| Mutton | 0.1700 |
| Veal | 0.1300 |
| Calf’s brains | 0.2000 |
| Calf’s kidney | 0.3200 |
| Calf’s liver | 0.1400 |
| Beef (lean) | 0.1100 |
| Pork (lean) | 0.1000 |
| Fish | |
| Trout | 0.1200 |
| Halibut | 0.3000 |
| Herring | 0.2700 |
| Cod | 0.1600 |
| Carp | 0.0860 |
| Salmon | 0.0610 |
| Mackerel | 0.2800 |
| Haddock | 0.3900 |
| Poultry | |
| Duck | 0.1400 |
| Goose | 0.2000 |
| Chicken | 0.1400 |
| Pigeon | 0.1500 |
| Turkey | 0.1700 |
| Venison | 0.1100 |
| Oysters (washed) | 0.5200 |
| Oysters (with sea water) | 1.1400 |
| Prepared Foods | |
| Plasmon | 0.2100 |
| Roborat | 0.0051 |
| Sanatogen | 0.4200 |
| Somatose | 0.6600 |
| Bovril’s preparations | 0.26-14.1000 |
| Valentine’s meat juice | 0.08-1.2000 |
| Egg (white and yolk) | 0.2100 |
| Egg (white alone) | 0.2100 |
| Egg (yolk alone) | 0.0390 |
| Caviar | 3.0000 |
| Milk (whole) | 0.1600 |
| Cream | 0.1300 |
| Buttermilk | 0.1600 |
| Whey | 0.11-0.1500 |
| Condensed milk | 0.4000 |
| Butter (unsalted) | 0.02-0.2100 |
| Butter (salted) | 1.00-3.0000 |
| Peanut butter | 4.1000 |
| Oleomargarine | 2.1500 |
| Palmin | 0.0016 |
| Fructin | 0.1000 |
| Smoked and Salted Foods | |
| Ham (raw) | 4.15-5.8600 |
| Ham (boiled) | 1.85-5.3500 |
| Salmon (smoked) | 7.5000 |
| Bacon (smoked) (German) | 1.0100 |
| Bacon (smoked) (American) | 11.6100 |
| Corned beef (German) | 2.0400 |
| Corned beef (American) | 11.5200 |
| Cod (salt)* | 23.5000 |
| Cod (salt, boneless)* | 10.0000 |
| Herring (smoked) | 11.7000 |
| Mackerel (salt dressed) | 10.4000 |
| Salmon (salted, smoked) | 10.3700 |
| Sardines (French in oil) | 1.3400 |
| Cod liver oil | 0.1700 |
| Gelatine (dry) | 0.7500 |
| Beef marrow | 0.1100 |
| Sausages (Frankfurters) | 2.2000 |
| Sausages (various kinds) | 2.90-8.1000 |
| Anchovy paste (Cross & Blackwell’s) | 40.1000 |
| Meat Extracts | |
| Liebig’s | 2.6000 |
| Kemmerich’s | 1.4000 |
| Various bouillon capsules, extracts, etc. | 9.40-22.0000 |
| Foods Prepared for Table | |
| Bouillon | 0.5-1.0000 |
| Thick soups | 0.5400 |
| Roast beef | 0.9800 |
| Roast pork | 1.5400 |
| Chops | 0.9700 |
| Roast chicken | 0.3900 |
| Sauces | 0.7-1.5000 |
| Spinach | 0.9100 |
| Cauliflower | 0.4900 |
| Stewed pears | 0.0190 |
| Macaroni (à la Napolitaine) | 1.0400 |
| Scrambled eggs (salted) | 1.1000 |
| Carrots | 0.4600 |
| Apple sauce | 0.4100 |
| Tapioca pudding (unsalted) | 0.0260 |
| Rice, with apples | 0.1800 |
| [Pg 359]Vegetables | |
| Potatoes | 0.016-0.0780 |
| Beets | 0.0530 |
| Beans | 0.0900 |
| Peas | 0.0580 |
| Lentils | 0.13-0.1900 |
| Lentils (dried) | 0.1550 |
| Artichokes | 0.0360 |
| Cauliflower | 0.05-0.1500 |
| Cucumber (fresh) | 0.06-0.0800 |
| Horseradish | 0.02-0.0600 |
| Radish | 0.0750 |
| Celery, stalks | 0.25-0.4900 |
| Celery, roots | 0.0890 |
| Asparagus | 0.04-0.0600 |
| Spinach | 0.084-0.2100 |
| Tomatoes | 0.0940 |
| Cabbage | 0.11-0.4400 |
| Onions | 0.016-0.0900 |
| Canned Vegetables | |
| Green corn* | 0.4000 |
| Green peas* | 0.7000 |
| Tomatoes | 0.1000 |
| Mushrooms | 0.04-0.0600 |
| Cheese | |
| Parmesan | 1.9300 |
| Swiss | 2.0000 |
| American (pale) | 0.8200 |
| Pineapple cheese | 2.1300 |
| Edam | 3.3000 |
| English cream cheese | 0.70-1.1500 |
| Infant Foods | |
| Nestlé’s Food | 0.2900 |
| Rademan’s | 0.0300 |
| Robinson’s patent groats | Trace |
| Bread, etc. | |
| Graham bread | 0.6100 |
| Pumpernickel | 0.4600 |
| White bread | 0.18-0.2000 |
| Zwieback | 0.3800 |
| Macaroni | 0.0670 |
| Cereals, etc. | |
| Barley | 0.0370 |
| Oats | 0.0460 |
| Rye | 0.0140 |
| Wheat | 0.0130 |
| Rice | 0.0390 |
| Corn (maize) | 0.0190 |
| Wheat flour | 0.002-0.0080 |
| Oatmeal (American) | 0.2900 |
| Oatmeal (German) | 0.2800 |
| Quaker oats | 0.0820 |
| Sago | 0.1900 |
| [Pg 360]Fruits | |
| Pineapple | 0.0710 |
| Orange | 0.057-0.0550 |
| Apricot | 0.0047 |
| Lemon | 0.0045 |
| Strawberry | 0.010-0.0200 |
| Chestnuts | 0.045-0.0100 |
| Cherry | 0.0130 |
| Cocoanut juice | 0.0350 |
| Olives | 0.008-0.2100 |
| Plums | 0.0046 |
| Gooseberry | 0.0210 |
| Watermelon juice | 0.0110 |
| Grape | 0.0240 |
| Almonds, dry | 0.0100 |
| Walnuts, dry | 0.0190 |
| Cane sugar | 0.1100 |
| Lump sugar | 0.0490 |
| Chocolate (Lindt) | 0.0730 |
| Spices | |
| Capers (preserved in salt) | 2.1000 |
| Capers (preserved in vinegar) | 0.2000 |
| Pepper, black | 0.5100 |
| Pepper, white | 0.0190 |
| Mustard | 2.6600 |
| Vanilla | 0.0550 |
| Cinnamon | 0.0610 |
| Cocoa beans | 0.05-0.0950 |
| Coffee, roasted | 0.0450 |
| Tea | 0.1500 |
| Drinks | |
| Ground water | 0.0012-0.0060 |
| Spring water | 0.00055-0.0046 |
| Ale | 0.0017 |
| Beer, German | 0.0160 |
| Beer, English | 0.1000 |
| Champagne (Moet & Chandon) | 0.0045 |
| Apollinaris | 0.0430 |
| Fachinger | 0.0390 |
| Giesshuble (Mattoni) | 0.0021 |
| Vichy | 0.0530 |
The kidneys find difficulty in eliminating certain substances, namely, the end-products of protein metabolism—urea, water, salts, and purin bodies.
The Urine constitutes the chief point of investigation. Analysis shows the presence of albumen, casts, blood cells, and pigments, with a corresponding deficiency in the normal constituents, water, urea, and salts.
Volume of Urine.—The volume of urine is reduced, and at times suppressed, owing to the difficulty with which the kidneys eliminate water in nephritic conditions.
The Blood shows the presence of the toxic substances on account of the inability of the kidneys to eliminate them properly.
[Pg 361] Edema is a common symptom and is probably due to the retention of salts and water by the tissues of the body. It is treated and at times relieved by limiting the intake of fluids and reducing the amount of sodium chloride in the diet.
Uremia is the most dreaded symptom and develops as a result of the retained toxins in the blood. Its development is prevented, if possible, by reducing the amount of fluid and food, even of milk, in the diet.
Uremic Poisoning is an acute intoxication due to the abnormal retention of these poisons and the inability of the kidneys to eliminate them. It is combated by instituting a starvation treatment which is followed by the above-mentioned restricted diet.
Gastro-intestinal Disturbances, especially diarrhea, are apt to develop in chronic nephritis. Care must be taken to keep the meals small in size, simple in proportion, and constituted only from the allowed foods.
Anemia follows the acute attack and is especially noticeable in those cases in which a rigid starvation régime has been found necessary. It may likewise be the result of a long-continued diet in which the proteins have been reduced to the lowest possible amount. The simple proteins in the diet must, at times, be increased and the patient advised to take plenty of fresh air and sunshine, in order to overcome this progressive anemia.
Restrictions in the diet are essential. These consist of limiting the amount of food and fluids as well as the type of food ingested.
Restricting the Proteins.—Proteins are restricted on account of the difficulty with which the end-products are eliminated by the kidneys, also on account of the toxic character of these substances.
Restricting the Fluids.—It is necessary, on account of [Pg 362] their difficulty of elimination and because they impose an excessive tax upon the circulatory organs.
Treatment is largely dietetic in character by reason of the advantages just mentioned.
Starvation Treatment is instituted in order that the work of the kidneys may be lessened. This treatment consists of abstinence from food with a definite reduction in the fluid intake. It is found to be necessary during the acute stage of the disease.
Extreme Thirst, which is apt to be an annoying symptom at this time, is relieved, as far as possible, with small sips of water or ice pellets held in the mouth.
Nephritic Cures are devised, as far as possible, to relieve the acute symptoms and to prevent the disease from developing into a chronic condition. Milk is the basis of most of these cures. It is given in definite amounts at stated intervals; the quantity and frequency with which it is given being adjusted to the state of the disease and the condition of the patient.
The Karell Cure is one of the best known diet cures used in the relief of acute nephritis. It consists of the giving of skimmed milk three or four times a day in doses ranging from three to six ounces for one week, at the end of which time, provided the stools remain solid, an increase to two quarts a day is made.
Constipation under the circumstances is a favorable symptom, indicating as it does the agreement of the milk.
Diarrhea as a result of gastro-intestinal disturbances has directly the opposite indication. In these cases the milk must be reduced. Karell advises the boiling of milk and relieving the constipation by means of mild laxatives or enemas.
Duration of the Karell Cure is from four to six weeks, after which a gradual return to a normal diet is made.
[Pg 363] Hunger is apt to be prominent at this stage of the treatment and is relieved during the second or third week by giving a small piece of dry bread and milk, soup thickened with a cereal, once a day.
Functional Kidney Tests are made to determine the character and extent of the impairment of the functions of the kidneys. The diets used in these tests contain definite amounts of certain diuretic substances, and the analysis of the urine voided during the twenty-four-hour period required by the test shows the nature of the impairment and furnishes, in a measure, a means of determining the amount of food and fluid which is safe for the patient to take. It likewise shows the extent to which the restrictions in the salt and proteins are necessary.
Salt-free, or Salt-poor Diets are necessary in some cases. While restriction in the amount of salt used in the preparation of food for the nephritic patient is always advisable, if there is a tendency to edema, the salt shaker should be left off the tray, and when there is a definite amount of salt prescribed, it should be weighed or measured for the day rather than for the meal, and the amount consumed recorded after each feeding.
Special Points for the nurse to remember are the necessity for an early recognition of unfavorable symptoms—of instructing the patient upon leaving her care in the need for keeping the size of the meals small;—of the danger of indulging in alcoholic or other stimulating beverages;—of eating highly spiced foods, or of eating anything which may cause gastro-intestinal disorders.
She should emphasize the need for regular examination of the urine and the value of rest and freedom from nervous excitement, and the need of living in the sunshine as much as possible.
The nurse should study the diet list and become familiar [Pg 364] with the foods allowed and those to be avoided. The tables show the foods which are rich in salts and proteins. She should likewise understand and be able to make the simple test for albumen in the urine and the method of collecting the urine for the test made in the laboratory.
(a) Outline a salt-poor diet for patient in which the fluids are limited to 1500 c.c. per day.
(b) Formulate a diet for child of ten years with nephritis following scarlet fever.
(c) Write a diet order, using a salt-free diet.
[114] Fisher’s Solution.
| Sodium carbonate (pure crystals) | 14 |
| Sodium chloride | 10 |
| Water | 1000 |
[115] The above diets used in the Olmstead Hospital, Rochester, Minn. Courtesy of M. Foley and D. Ellithorpe, Mayo Clinic.
[117] For more extensive lists see Table of “Ash Constituents of Common Food,” pp. 472 to 477.
[118] “Journal of Internal Medicine,” Vol. XIV, 1914.
[119] Ibid.
[120] “Food for the Sick,” p. 108, by Strouse and Perry.
[121] Beans and peas belong to the class of foods known as legumes, which are high in protein and must be treated as any other protein food.
[122] Author’s list and diet sheets.
[123] Meats of all sorts should be boiled, or only the inside portions allowed.
[124] Some physicians exclude ice cream from the diet, while others permit a small portion, provided it is not so rich as to cause digestional disturbances.
[125] Boiled sweetbreads are sometimes allowed, but should never be given without the advice of a physician.
[126] The preparation of the menus requires care and attention; meal must be small and all fried foods avoided.
[127] “Food for the Sick,” p. 112, by Strouse and Perry.
[128] “Medical Clinics of Chicago,” Vol. II, No. 5, 1917.
[129] Copied from “Medical Clinic of Chicago,” Vol. II, No. 5, 1917.
[130] NaCl, 2 to 3 grams in a capsule accompanying each meal. Any salt unused is returned to the diet kitchen, where it is weighed and the amount used is indicated on the chart.
[131] Carried out by Dr. Henry Christian and described by James O’Hara in the “Archives of Internal Medicine,” Vol. XVII.
[132] The outside parts of roast meat must be avoided, even when meat is allowed once a day. Meat is only added after the condition materially improves.
[133] Coleman, in Forchheimer’s “Therapeusis of Internal Diseases,” Vol. I, p. 642.
The dietetic treatment in diseases of the heart has been the subject of much study, especially during the past few years.
The Diet.—In this pathological condition, as in many other diseases in which one or more of the functions of the body have become impaired, there can be no hard and fast rule covering the treatment or diet for all cases, but, as in nephritis, the condition of the individual, his symptoms, and the progress and extent of the disease must be taken into consideration in order to formulate a diet calculated to adequately nourish the body, while at the same time imposing the smallest amount of work with the least expenditure of labor upon the part of the diseased organ.
Division of Treatment.—The treatment of the disease then may be said to be divided into three stages: first, the stage of compensation; second, that of moderate compensation; third, that of decompensation. The diet is directed, first, toward relieving as far as possible the strain which is imposed more or less by all the food eaten; and second, keeping up the general nutrition of the body.
Dietetic Treatment.—No matter what has caused the impairment of the heart functions, the treatment must necessarily remain the same as far as diet is concerned. The patient is no longer able to handle a full and unrestricted diet. As long as compensation is good, the restrictions are scarcely noticeable; alcoholic beverages and possibly tobacco may have to be, to a certain extent, curtailed, and in some cases avoided altogether. However, if the [Pg 366] individual desires to live and be comfortable while so doing, he must lead a wholesome, simple life, since he cannot with safety indulge in any excesses, either in diet or in any other particular.
Diet in Second Stage.—When the second stage sets in, that is, when the heart muscle is unable to perform its normal function, attention must be directed toward two main points; first, the work of the heart; second, the pressure upon that organ from other sources, namely, the stomach and intestines. As long as the food does not disagree, that is, so long as there is no fermentation or putrefaction of the food material in the stomach and intestines the flatulence arising from the evolution of gas in those organs is slight and the pressure upward upon the heart inconsiderable.
Restricting the Fluids.—The heart must be spared all unnecessary work. This can only be accomplished by limiting the amount of food and fluids ingested. The latter imposes an extra burden upon the impaired organ to eliminate. Consequently, the amount of fluid should be limited to 1500 c.c. a day at most, and in many cases considerably less than that quantity.
Regulating the Meals.—The meals should be small and the intervals of feeding regular. It has been found best to give the fluids between meals rather than with the food. In many cases of heart disease, as in certain nephritic conditions, edema is a prominent symptom, so that it is necessary to direct our efforts toward overcoming that particular condition. The Karell Cure[134] and the salt-poor diet are used with excellent results. The latter is not so low as the former, and in many cases will accomplish all that is required. A modified Karell diet is used in the Michael Reese Hospital[135] in Chicago as follows:
“MODIFIED KARELL TREATMENT”
(Salt-free)
“Milk 200 c.c. at 8 A.M., 12 M., 4 P.M., and 8 P.M., for five to seven days.
Eighth day—Milk same as above.
10 A.M. one soft egg; 6 P.M. 2 slices of dry toast.
Ninth day—Milk as above.
10 A.M. one soft egg and 2 slices of toast.
Tenth to twelfth day—Milk as above.
12 M. chopped meat, rice boiled in milk, easily digested vegetables.
6 P.M. one soft-boiled egg.
The diet is gradually increased until a full tray is reached. All meats and vegetables should be chopped or scraped at first, and the heavier foods should be given only when the heart is practically compensated.”
Rules and Regulations.—There are a few general rules which it has been found advisable to impress upon individuals suffering from a disease in which the muscles of the heart have become weakened. The compensation of the organ may improve, but there is still a danger of a reoccurrence or a further development more or less serious, and at times fatal. So for this reason, certain rules must be observed throughout life:
First: the necessity for keeping the meals small, simple, and digestible. Death at times occurs with symptoms of gastric disturbance, which is, after all, due to the heart. Consequently it is not wise to invite such disaster by overeating, or by the partaking of any food which is liable to bring about indigestion, either in the stomach or in the intestines. Most authorities advise four or five meals a day rather than the regulation three, and limit the fluids at meal time to a few ounces only, when any are allowed, and [Pg 368] to a maximum amount of 1500 c.c. during the day, chiefly between meals.
Second: the need for limiting the amount and type of exercise taken, especially after eating, since the work of digestion requires all the power and strain of which the heart is capable, and since an additional tax placed upon it by muscular exertion might readily be just the final straw, the added fraction which weighs down the balance on the scale of life.
Third: the advisability of abstaining from alcoholic beverages, unless specially prescribed by the physician in charge.
Certain elderly people suffer from a condition known as senile heart, which is more or less associated with arteriosclerosis and high blood pressure. These individuals should be prevailed upon to take the precaution of regulating their habits of life, avoiding excesses of all kinds, not only on account of the weakened condition of the heart, but also on account of the condition of the arteries. They should avoid excitement and worry, since the very fact that they are worrying increases the blood pressure. Simple foods in limited quantities, five meals a day instead of three, and an avoidance of too much fluid, should be the keynote of their daily régime.
Tact on the part of the nurse is necessary in all cases, both young and old. It is often more difficult to instill good dietary habits in heart patients, after acute symptoms have subsided, than to carry them out during the acute attack, when the life itself depends upon a rigid adherence to the diet prescribed. But as these rules and regulations are essential to the future welfare of the patient, he must be taught with care, and in such a way that he will not be alarmed to an extent when more harm than good will come of the teaching.
The diet should consist chiefly of milk, eggs, rare meat in [Pg 369] moderation (mutton, chicken, fish, and oysters), well-baked bread, well-cooked cereals, potatoes and green vegetables, and simple desserts. All foods which in any way cause gastric or intestinal disturbances must be avoided. If these disturbances arise during the course of the disease, the patient should be promptly returned to the strict milk diet. When edema is prominent, it is treated as already described in the treatment for the like condition in nephritis by the Karell or salt-free diet.
The dietetic treatment given here is merely a guide to be used under certain conditions. The physician formulates the diet, and the nurse must understand what to expect and how to apply the treatment as the symptoms arise.
Dietetic Treatment, adjusted to relieve the weakened heart muscles and to save the organ from all possible strain.
Three Stages, during which the treatment changes according to the extent and progress made by the disease.
First Stage: The diet is practically normal. Compensation is good, consequently no dietary measures save the limiting of alcoholic beverages are necessary.
Second Stage: The compensation is only moderate and the heart cannot perform its normal functions, hence the diet must be directed toward relieving any pressure upon the organs from other organs and toward lessening the work of the heart itself.
Third Stage: In which the compensation is decidedly impaired and for this reason the dietetic treatment undergoes a decided change.
Digestional Disturbances in which there is an evolution of gas in the stomach or intestines may cause a pressure against the heart which is distinctly bad for it.
Limiting the Fluids in the diet in heart disease is necessary when the compensation is only moderate, as they impose an extra burden upon the organ to eliminate them.
[Pg 370] Amount of Food must also be limited. The meals must be small and taken without fluid. The latter should be taken between meals.
Edema occurs in a number of cases and must be treated as in nephritic conditions by limiting the fluids and by confining the diet to “salt-poor” foods.[136]
Karell Cure or modification thereof has been used with good results in many cases of heart disease.
Exercise must be limited in amount and confined to types which will not impose a tax upon the weakened heart muscles. Exercise after eating is especially to be discouraged, as this, together with the efforts required for the digestion of food, might readily prove too much for the heart to accomplish.
Elderly Patients must be warned against exercises of all kinds, not only on account of the condition of the heart, but also on account of the condition of the arterial walls. These harden with age and break down under undue pressure.
The Nurse should instruct the patient on the points necessary for the saving of the heart. She should teach the necessity for keeping the meals small and having them more frequently if necessary; of limiting the fluids at meals to a few ounces or leaving them out altogether at this time. She should know how necessary is the reduction of the fluid. She should also warn against the taking of alcoholic beverages except with the permission and advice of a physician.
Excitement and Worry increase the blood pressure, hence must be avoided by individuals suffering with any form of heart disease.
(a) Write a diet order for an elderly patient with severe cardiac disturbance.
(b) Outline the method of administering the Karell diet.
[135] “Food for the Sick,” p. 150, by Strouse and Perry.
Definition.—Diabetes is a disease which is characterized by an inability on the part of the body to utilize the carbohydrates, in consequence of which there is abnormal excretion of glucose in the urine.
Sugar in the Urine.—The appearance of sugar in the urine may not necessarily signify diabetes, it may be merely a temporary glycosuria due to certain pathological conditions, such as infectious diseases, diseases or trauma which affect the pancreas, and which disappear upon the recovery from the disease. But any appearance of sugar in the urine should be looked upon with suspicion, since the future welfare of the patient depends largely upon an early diagnosis in any form of diabetes.
True Diabetes.—Allen claims that true diabetes may always be distinguished from nervous glycosuria by the application of the laws governing these conditions (Allen’s Paradoxical Law[137]), which is “whereas in normal individuals the more sugar given the more is utilized, the reverse is true in diabetes.”
Manufacture of Sugar from Other Foods.—If the carbohydrate foods alone caused all the trouble in diabetes, the disease might be more easily controlled. This, we found, however, not to be true, since in certain conditions the body utilizes the protein foods for the manufacture of glucose also. Consequently in diabetes if the absolute sugar output of the body is to be controlled, the intake of nitrogenous foods must be likewise adjusted.
[Pg 372] Functions of Carbohydrates.—In the chapter describing the functions of the carbohydrates in the human body it was demonstrated that their energy-producing properties did not cover the extent of their usefulness. It has been proved that this food constituent normally acts as neutralizing agent for the toxic acids produced within the organism as a result of the breaking down of the fats. Hence, when this function of the carbohydrates becomes impaired, these acids, Oxybutyric acid, Diacetic acid and Acetone, fail to be neutralized and are consequently absorbed into the blood stream, giving rise to a form of intoxication known as acidosis. When acidosis becomes extreme, the diabetic patient is apt at any time to succumb to the dreaded diabetic coma.
Keeping Urine Sugar Free.—Thus it is seen that the treatment of diabetes mellitus consists not alone of freeing the urine from sugar and keeping it free, but of controlling the acidosis which may at any time develop.
Diabetic Cures.—Numberless so-called diabetic cures have been brought forward and more or less tested for years, but whether they have really accomplished cures has not been satisfactorily proved. Not until Dr. Allen instituted what is known as the Allen’s Starvation Treatment has the disease been so universally treated, at least by one method or modification of one method. Dr. Joslin, who has used this treatment most successfully, does not claim to have accomplished a cure, but states that he is watching the results of the treatment in his patients with interest.
Starvation Treatment.—The Allen Starvation Treatment consists of first a period of about forty-eight hours in which the patient is given an ordinary diet, during which time the daily weight is taken and the urine examined and recorded.
Acidosis.—It has been found in some cases, such as with elderly patients or those in whom there is an evident [Pg 373] acidosis, advisable to precede the period of starvation by a preliminary treatment.
Method of Treatment.—Joslin[138] suggests the following method of procedure:
“Without otherwise changing the diet omit fat. After two days, omit protein, then halve the carbohydrates daily until the patient is taking only ten grams, then fast.”
In the Michael Reese Hospital, the following series of test diets are given to determine the severity of the diabetes:
| BREAKFAST | |
| Grapefruit | ½ |
| Eggs | 2 |
| Bacon | 20 grams |
| Bread | 25 grams |
| Butter | 10 grams |
| Cream | 15 c.c. |
| Coffee | 1 cup |
| DINNER | |
| Cream soup | 3 oz. |
| Roast beef | 75 grams |
| Spinach | 100 grams |
| Kohl-rabi | 100 grams |
| Lettuce salad | 50 grams |
| Ripe olives | 15 grams |
| Bread | 25 grams |
| Butter | 20 grams |
| Wine gelatin | 4 oz. |
| Coffee | |
| Cream | 15 c.c. |
| SUPPER | |
| Lamb chop | 1 |
| Asparagus tips | 50 grams |
| Eggplant | 50 grams |
| Tomato salad | 50 grams |
| Custard (diabetic) | |
| Coffee | |
| Cream | 15 c.c. |
| Butter | 20 grams |
| Bread | 25 grams |
Diet in Mild Cases.—This diet contains approximately 70 grams of protein, 100 grams of fat, and 70 grams of carbohydrates, and the patient is kept on it for at least two days; then the carbohydrates are cut down by taking away 25 grams of bread every day.
| Key: | |
| A | Carbohydrate |
| B | Protein |
| C | Fat |
| D | Calories |
| E | 5% Vegetable |
| F | Orange |
| G | Oatmeal |
| H | Shredded Wheat |
| I | Uneeda |
| J | Potato |
| K | Bread |
| L | Egg |
| M | Cream 20% fat |
| N | Bacon |
| O | Butter |
| P | Meat |
| Q | Fish |
| R | Skimmed Milk |
| Diets with which to become Sugar free | Diet in Grams | Test Diets | Name of Diet | ||||||||||||||||
| A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | ||
| T. D.1 | 189 | 89 | 15 | 1247 | 300 | 300 | ... | 1 | ... | 240 | 90 | ... | ... | ... | ... | 90 | 120 | 480 | 1 |
| T. D.2 | 102 | 58 | 0 | 640 | 300 | 300 | ... | 1 | ... | 120 | ... | ... | ... | ... | ... | ... | 180 | 300 | 2 |
| T. D.3 | 64 | 33 | 0 | 388 | 300 | 300 | ... | ... | ... | 60 | ... | ... | ... | ... | ... | ... | 90 | 240 | 3 |
| T. D.4 | 36 | 27 | 0 | 252 | 300 | 200 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | 90 | 120 | 4 |
| T. D.5 | 15 | 5 | 0 | 80 | 300 | 50 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | 5 |
| Maintenance Diets | Carbohydrate (C) | Protein and Fat (PF) | |||||||||||||||||
| C1+PF1 | 10 | 11 | 6 | 138 | 300 | ... | ... | ... | ... | ... | ... | 1 | ... | ... | ... | ... | ... | ... | 1 |
| C2+PF2 | 22 | 13 | 18 | 302 | 300 | 100 | ... | ... | ... | ... | ... | 1 | 60 | ... | ... | ... | ... | ... | 2 |
| C3+PF3 | 32 | 24 | 24 | 440 | 600 | 100 | ... | ... | ... | ... | ... | 2 | 60 | ... | ... | ... | ... | ... | 3 |
| C4+PF4 | 42 | 29 | 39 | 635 | 600 | 200 | ... | ... | ... | ... | ... | 2 | 60 | 30 | ... | ... | ... | ... | 4 |
| C5+PF5 | 52 | 32 | 53 | 813 | 600 | 200 | 15 | ... | ... | ... | ... | 2 | 60 | 30 | 15 | ... | ... | ... | 5 |
| C6+PF6 | 63 | 43 | 65 | 1009 | 600 | 200 | 30 | ... | ... | ... | ... | 2 | 90 | 30 | 15 | 30 | ... | ... | 6 |
| C7+PF7 | 73 | 51 | 70 | 1126 | 600 | 300 | 30 | ... | ... | ... | ... | 2 | 90 | 30 | 15 | 60 | ... | ... | 7 |
| C8+PF8 | 83 | 59 | 87 | 1351 | 600 | 300 | 30 | ... | 2 | ... | ... | 2 | 90 | 30 | 30 | 90 | ... | ... | 8 |
| C9+PF9 | 96 | 62 | 93 | 1469 | 600 | 300 | 30 | ½ | 2 | ... | ... | 2 | 120 | 30 | 30 | 90 | ... | ... | 9 |
| C10+PF10 | 107 | 63 | 93 | 1517 | 600 | 300 | 30 | 1 | 2 | ... | ... | 2 | 120 | 30 | 30 | 90 | ... | ... | 10 |
| C11+PF11 | 131 | 75 | 98 | 1706 | 600 | 300 | 30 | 1 | 2 | 120 | ... | 2 | 120 | 30 | 30 | 120 | ... | ... | 11 |
| C12+PF12 | 155 | 79 | 98 | 1818 | 600 | 300 | 30 | 1 | 2 | 240 | ... | 2 | 120 | 30 | 30 | 120 | ... | ... | 12 |
| Food | Weight in grams | Approximate equivalent |
| Orange | 300 | One and one-half (large size) |
| 5 per cent vegetables | 300 | Three moderate portions |
| Skimmed milk | 480 | One pint (16 ounces) |
| Fish | 120 | Two small portions |
| Potato | 240 | Two medium sized potatoes |
| Meat | 90 | One moderate portion |
| Bread | 90 | Three small slices |
| Oatmeal (dry wgt.) | 30 | One large saucerful |
| Cream | 60 | Four tablespoonfuls |
| Bacon | 30 | Four crisp strips |
| Butter | 30 | Three medium portions |
The Test Diets are designed for the period during which the patient becomes gradually sugar free. On successive days advances can be made from Test Diet 1 to Test Diet 5, and if on the fifth day the patient is not sugar free, fasting can be employed for one or more days.
The Maintenance Diets are for use so soon as the urine of the patient is free from sugar. If this occurs as a result of Test Diet 5 the patient begins with Maintenance Diet C1PF1. The actual articles of food representing the carbohydrate in the diet for the first day are given under the heading of carbohydrate, for convenience described C1, 2, 3, etc. The articles referred to under protein and fat are under that heading, which for the same reason is described as PF1, 2, 3, etc. Certain cases of diabetes can proceed steadily day by day from C1PF1 to C12PF12, without showing sugar. If sugar does appear in the urine, drop back two days in the carbohydrate group, wait till sugar free, then advance in the protein and fat group until sufficient calories are obtained. Thus, if sugar shows on C7PF7 the diet prescribed would be that included in C5PF7 and thereafter progression could be made in the PF group until twenty-five to thirty calories per kilogram body weight were furnished the patient.
Occasionally the patient becomes sugar free on Test Diet 2, 3, or 4. It is then unnecessary to begin with Maintenance Diet C1PF1, but instead with a maintenance diet which contains a value for carbohydrate similar to that of the test diet upon which the patient became sugar free.
If the protein and fat are too high for the individual on a given day it is easy to advance the carbohydrate and decrease to an earlier day on protein and fat.
The plan is arbitrary and the majority of cases will demand some modification. It is arranged to enable patient or nurse to see in advance the general plan of treatment.
(Courtesy of Dr. Joslin and Thomas Groom & Co., Boston.)
[Pg 376] If the case is a mild one, this may be sufficient to free the urine from sugar, but the diet is given primarily to enable the physician to find out by means of urinalysis just how great is the functional impairment.
In some cases, which are mild in character, the urine is made free of both sugar and acetone without further dietetic measures. However, when a severe diabetes is manifested and a high percentage of glucose and in some cases acetone bodies are found in the urine a more rigid treatment will be found necessary.
Preliminary Diet.—Many physicians find it advisable, as has already been stated, to cut down the food allowance before stopping it entirely. In the Michael Reese Hospital this is done by first giving a practically fat-free diet, followed by one or two days in which three or four eggs, 250 to 300 grams (8 or 10 ounces) of 5% vegetables are given, after which it is found safe to institute the starvation treatment.
Sample Menus.—The following menus are given to illustrate the dietetic treatment which it is deemed advisable to institute in cases where the starvation treatment cannot be given at once:
After the test diet of forty-eight hours, the following régime is instituted:
Third Day
| Key: | |
| A | Protein Gm. |
| B | Fat Gm. |
| C | Carbohydrate Gm. |
| D | Calories |
| A | B | C | D | ||
| Breakfast: | |||||
| ½ grapefruit | 5.00 | 20 | |||
| 1 egg | 5.3 | 4.10 | 59 | ||
| 1 slice bread | 30 gm. | 2.6 | .30 | 15.00 | 73 |
| Tea or coffee | |||||
| Total for meal | 7.9 | 4.40 | 20.00 | 152 | |
| Dinner: | |||||
| Broth | 180 c.c. | 3.7 | .17 | .34 | 18 |
| Chicken (breast) | 90 gm. | 18.2 | 2.10 | 92 | |
| Spinach | 100 gm. | 2.0 | 3.00 | 20 | |
| Potato (1 medium) | 90 gm. | 1.8 | .09 | 15.60 | 70 |
| Lemon jelly | 90 gm. | 4.2 | 2.70 | 27 | |
| Total for meal | 29.9 | 2.30 | 21.60 | 227 | |
| Supper: | |||||
| Lamb chop | 50 gm. | 9.3 | 14.10 | 126 | |
| Asparagus | 100 gm. | 1.5 | 3.00 | 18 | |
| Bread | 20 gm. | 1.6 | .20 | 10.00 | 48 |
| Tea or coffee | |||||
| Total for meal | 12.4 | 14.30 | 13.00 | 192 | |
| Total for day | 40.2 | 21.00 | 54.60 | 571 | |
Fourth Day
| Key: | |
| A | Protein Gm. |
| B | Fat Gm. |
| C | Carbohydrate Gm. |
| D | Calories |
| A | B | C | D | ||
| Breakfast: | |||||
| ½ grapefruit | 5.0 | 20 | |||
| 1 egg | 5.3 | 4.10 | 59 | ||
| 1 slice bread | 20 gm. | 1.6 | .20 | 10.0 | 48 |
| Coffee or tea | |||||
| Total for meal | 6.9 | 4.30 | 15.0 | 107 | |
| Dinner: | |||||
| Tomato bouillon | 180 gm. | 2.2 | .23 | 2.5 | 15 |
| Whitefish | 90 gm. | 2.0 | 5.0 | 28 | |
| Boiled onions | 100 gm. | 1.5 | .30 | 7.5 | 40 |
| Bran muffin (1) | 5.0 | 7.00 | 4.5 | 101 | |
| Tea or coffee | |||||
| Total for meal | 25.7 | 16.20 | 20.5 | 322 | |
| Supper: | |||||
| 1 egg | 5.2 | 4.10 | 59 | ||
| Tomato (baked) | 100 gm. | .6 | 2.0 | 10 | |
| Bran muffin (1) | 1.0 | 5.00 | 7.0 | 101 | |
| Tea or coffee | |||||
| Total for meal | 6.8 | 9.10 | 9.0 | 170 | |
| Total for day | 38.4 | 29.60 | 44.0 | 513 | |
Fifth Day
| Key: | |
| A | Protein Gm. |
| B | Fat Gm. |
| C | Carbohydrate Gm. |
| D | Calories |
| A | B | C | D | ||
| Breakfast: | |||||
| ½ grapefruit | 5.0 | 20 | |||
| Broiled tomato | 100 gm. | 1.50 | 3.0 | 18 | |
| Tea or coffee | |||||
| Total for meal | 1.50 | 8.0 | 38 | ||
| Dinner: | |||||
| Broth | 120 c.c. | 3.00 | 12 | ||
| Lettuce | 50 gm. | .50 | 1.5 | 8 | |
| Cauliflower | 90 gm. | 1.50 | .40 | 3.9 | 25 |
| Tea or coffee | |||||
| Total for meal | 5.00 | .40 | 5.4 | 45 | |
| Supper: | |||||
| 1 egg | 5.35 | 4.16 | 59 | ||
| String beans | 100 gm. | 2.00 | 5.0 | 28 | |
| Celery | 50 gm. | .50 | 1.5 | 8 | |
| Tea or coffee | |||||
| Total for meal | 7.85 | 4.16 | 6.5 | 85 | |
| Total for day | 14.30 | 12.50 | 19.9 | 168 | |
Sixth Day
| Key: | |
| A | Protein Gm. |
| B | Fat Gm. |
| C | Carbohydrate Gm. |
| D | Calories |
| A | B | C | D | ||
| Breakfast: | |||||
| Asparagus tips | 60 gm. | 1.50 | 3.0 | 18 | |
| Spinach | 60 gm. | 1.10 | 1.80 | 1.8 | 32 |
| Tea or coffee | |||||
| Total for meal | 2.68 | 1.80 | 5.8 | 50 | |
| Dinner: | |||||
| Stewed celery | 100 gm. | 1.00 | .10 | 2.1 | 15 |
| String beans | 50 gm. | 1.50 | 2.5 | 16 | |
| Tea or coffee | |||||
| Total for meal | 2.50 | .10 | 5.6 | 31 | |
| Supper: | |||||
| Beet tops | 75 gm. | 1.50 | 2.5 | 16 | |
| Onions (boiled) | 75 gm. | 1.50 | .30 | 7.5 | 44 |
| Tea or coffee | |||||
| Total for meal | 3.00 | .30 | 10.0 | 60 | |
| Total for day | 11.20 | 2.20 | 21.4 | 141 | |
Method of Administering Treatment.—In many cases the patient is first put to bed during the starvation treatment, but recently Dr. Allen has emphasized the value of exercise, claiming that it assists in utilizing the sugar. In any case, the starvation régime remains the same. The patient is given only coffee or clear broth with or without whisky (one ounce every two hours) and the treatment continued from one to four days, or until the urine becomes sugar free.[141]
It has rarely been found necessary to continue the fast longer than four days, since in most cases the sugar decreases rapidly upon the discontinuance of food.
Loss of Weight.—The slight loss of weight, which may be noticeable as the result of starvation, is not undesirable, especially in those cases where obesity is a prominent feature. In fact care must be exercised in the follow-up treatment to prevent the taking on of weight by the diabetic individual, since, according to Allen, it is often found that even moderately obese patients (180 lb.) continue to excrete a small amount of sugar so long as they hold this weight, even upon a low carbohydrate diet, whereas those same patients show no difficulty in becoming sugar free if the weight is reduced by ten or fifteen pounds.
A number of schedules have been devised to enable the nurse successfully to carry out the Allen Treatment. In following out this treatment and reëducating the organs afterward to tolerate foods which they have been unable to handle on account of the impairment of the sugar-making [Pg 380] organs, it is necessary to make a series of tests whereby the diet is gradually increased in its various constituents until the diabetic patient is able to handle a reasonable amount of carbohydrates as well as other foods which have given more or less trouble in the past.
The following schedule, after Joslin,[142] is included, and a careful study of it is advised in order that the nurse may intelligently carry out the Allen Treatment.
Schedule.—Fasting in many cases begins at once and the patient experiences no ill effects from it. However, in severe, long-standing cases many patients do better if the fats are omitted at once and the rest of the diet left unchanged for two days. Then the proteins in the diet are omitted and the carbohydrates cut in half. This halving of the carbohydrates is continued daily until only 10 grams remain, after which they too are omitted. The fast is thus made complete and remains so until the urine is entirely free from sugar.
Carbohydrate Tolerance is determined by giving, as soon as the urine has been sugar-free for twenty-four hours, 150 grams of 5% vegetables. This is equivalent to from 8 to 10 grams of carbohydrates. After this 5 grams of carbohydrates, or 75 grams of 5% vegetables, are added daily to the diet until the patient is taking 20 grams. Then the addition of 5 grams of carbohydrates is made every other day, using the fruits and vegetables belonging to the 10% and 15% carbohydrate group, until potatoes and oatmeal and finally bread can be tolerated unless sugar appears in the urine before this or the tolerance reaches 3 grams to each kilogram of body weight or, in other words, until a man weighing 150 pounds is consuming 225 grams of carbohydrates per day.
[Pg 381] Protein Tolerance.—In making the test for the protein tolerance it is necessary to wait until the urine has been sugar free for forty-eight hours; 20 grams of protein is then given. This is equivalent to 3 eggs, and daily additions of 5 grams protein are made, usually in the form of meat, until the patient is receiving 1 gram of protein to every kilogram of his body weight per day unless his carbohydrate tolerance is zero, in which case it is wise to add only three-fourths of a gram of protein per day.
Fat Tolerance.—A determination of the fat tolerance is made coincidently with that of the protein. No additional fat is allowed until the protein tolerance reaches 1 gram per kilogram of body weight, unless the patient’s tolerance for protein is less than that. After which 25 grams of fat per day are added until there is no further loss of weight, taking care never to allow more than 40 calories per kilogram of body weight.
Reappearance of Sugar.—Should the urine again show the presence of sugar, another period of fasting lasting for twenty-four hours, or until the urine is again sugar free, must be instituted. After the second fast the increase in the diet may be twice as rapid as used after the first fast. However, it is not advisable to increase the amount of carbohydrates to more than half of that determined by the former tolerance for a period of two weeks, during which time the urine has been entirely sugar free, then the increase is made more slowly and the amount given should not exceed 5 grams a week.
Weekly Fast Days.—One day in seven should be set aside by the diabetic patient for fasting, when the carbohydrate tolerance is less than 20 grams. When, however, the tolerance is between 20 and 50 grams of carbohydrates, the patient may take one-half of his daily allowance of protein and fat and a certain amount of 5% vegetables as well upon [Pg 382] the weekly fast day. When the tolerance reaches between 50 and 100 grams per day, vegetables of a higher carbohydrate content may also be included. If the carbohydrate tolerance should exceed 100 grams per day, the carbohydrates upon the fast day may be simply half of the amount allowed upon other days.
The Giving of Alkalies.—If acidosis is evident, as may be indicated by an excretion of diacetic acid, oxybutyric acid, or acetone in the urine, alkalies may be given. Bicarbonate of soda may be given in doses of 2 grams every 3 hours, as suggested by Hill and Eckman,[143] but this is not as a rule necessary, for, as Jacobi aptly remarks: “Prevention is the treatment of acidosis in children, and those susceptible to acidosis should not have fat.” What he has said for children holds good for adults. However, it is likewise true that fat must constitute a large part of a diabetic diet and the only way to prevent it poisoning, is to raise the fat in the diet gradually until the tolerance is determined.
Determining the Extent of Acidosis.—It will be remembered that in an earlier chapter it was found that the excretion of ammonia in the urine to a certain extent indicated the extent of the acidosis in the body, that is, if the ammonia output exceeds three or four grams a day (twenty-four hours), the extent of the acidosis is considerable, while if it falls below that amount it is not alarming. More exact methods, however, for the determining of the severity of the acidosis will be found in another part of this text, where the test for sugar and the acetone bodies will be explained in detail.
Dietetic Treatment.—The patient is placed upon a vegetable diet consisting of vegetables containing not more than five per cent. carbohydrate.[144] These vegetables have their carbohydrate content still further reduced by changing [Pg 383] the water in which they are cooked three times. In many cases this will reduce their content as much as one-half.
A small amount of fat usually in the form of butter is allowed with these vegetables. The amount of 5% vegetables given must be carefully adjusted since the patient might readily take too much if allowed to follow the dictates of his appetite.
The carbohydrate intake during the first one or two days must be limited to 15 grams. This allows about 10 grams of protein, 7 grams of fat, and 15 grams of carbohydrates. Tea or coffee, without sugar or cream, may be given at each of the three meals.
The following table is included, showing the various foods arranged according to their carbohydrate content:
Meats, fish, broths, gelatin, eggs, butter, olive oil, coffee, tea, and cracked cocoa.
Foods arranged approximately according to per cent of carbohydrates
| 5% | 10% | 15% | 20% | |
| Vegetables, Fresh or Canned | Lettuce | Pumpkin | Greens | Potatoes |
| Cucumbers | Turnip | Peas | Shell beans | |
| Spinach | Kohl-rabi | Artichokes | Baked beans | |
| Asparagus | Squash | Parsnips | Green corn | |
| Rhubarb | Beets | Lima beans (canned) | Boiled rice | |
| Endive | Carrots | Boiled macaroni | ||
| Marrow | Onions | Prunes | ||
| Sorrel | Mushrooms | |||
| Sauerkraut | ||||
| Beet greens | ||||
| Dandelion | ||||
| Swiss chard | ||||
| Celery | ||||
| Brussels sprouts | ||||
| Water cress | ||||
| Sea kale | ||||
| Okra | ||||
| Cauliflower | ||||
| Eggplant | ||||
| Cabbage | ||||
| Radishes | ||||
| Leeks | ||||
| String beans | ||||
| Broccoli | ||||
| Tomatoes | ||||
| Fruits | [Pg 384]Ripe olives (20% fat) | Lemons | Apples | Plums |
| Grapefruit | Oranges | Pears | Bananas | |
| Cranberries | Apricots | |||
| Blackberries | Blueberries | |||
| Gooseberries | Cherries | |||
| Peaches | Currants | |||
| Pineapple | Raspberries | |||
| Watermelon | Huckleberries | |||
| Nuts | Butternuts | Brazil nuts | Almonds | Peanuts 40% |
| Pignolias | Black walnuts | English walnuts | Chestnuts | |
| Hickory | Beechnuts | |||
| Pecans | Pistachios | |||
| Filberts | Pine nuts | |||
| Misc. | Unsweetened and unspiced pickle, clams, oysters, scallops, liver, fish roe. | Reckon available carbohydrates in vegetables of 5% group as 3%, of 10% group as 6%. | ||
30 grams (1 oz.) contains approximately:
| Key: | |
| A | Protein Gm. |
| B | Fat Gm. |
| C | Carbohydrate Gm. |
| D | Calories |
| A | B | C | D | |
| Oatmeal, dry weight | 5.0 | 2 | 20.0 | 110 |
| Meat (uncooked ham) | 6.0 | 3 | 0.0 | 50 |
| Meat (cooked ham) | 8.0 | 5 | 0.0 | 75 |
| Broth | 0.7 | 0 | 0.0 | 3 |
| Potato | 1.0 | 0 | 6.0 | 25 |
| Bacon | 5.0 | 15 | 0.0 | 155 |
| Cream, 40% | 1.0 | 12 | 1.0 | 120 |
| Cream, 20% | 1.0 | 6 | 1.0 | 60 |
| Milk | 1.0 | 1 | 1.5 | 20 |
| Bread | 3.0 | 0 | 18.0 | 90 |
| Butter | 0.0 | 25 | 0.0 | 240 |
| Egg (one) | 6.0 | 6 | 0.0 | 75 |
| Brazil nuts | 5.0 | 20 | 2.0 | 210 |
| Orange or grapefruit (one) | 0.0 | 0 | 10.0 | 40 |
| Vegetables, 5% and 10% groups | 0.5 | 0 | 1 or 2 | 6 or 10 |
| Oysters | 6.0 | 1 | 4.0 | 50 |
Carbohydrate equivalent of 1 slice of white bread (1 oz. or 30 gm.) containing approximately 15 gm. of starch
| Uncooked Flours, etc. | Household Measure[147] | Gm. | Cooked Vegetables | Household Measure | Gm. |
| Barley | 1 h. tbs. | 21 | Artichokes | 1 medium | 320 |
| Buckwheat | 1 h. tbs. | 19 | Beans (baked canned) | 2 h. tbs. | 75 |
| Corn meal | 1 h. tbs. | 20 | Beans, lima | 1¼ tbs. | 50 |
| Farina | 1 h. tbs. | 20 | Beets | 6 tbs. | 200 |
| Hominy | 1 h. tbs. | 18 | Carrots | 13 tbs. | 446 |
| Macaroni | 1 h. tbs. | 20 | Okra | 4 tbs. | 200 |
| Noodles | 1½ h. tbs. | 20 | Onions | 3 tbs. | 300 |
| Oatmeal | 1 h. tbs. | 22 | Parsnips | 4 slices | 120 |
| Rice | 1 h. tbs. | 18 | Peas, green | 3 h. tbs. | 100 |
| Rye flour | 1 h. tbs. | 18 | Potatoes (baked) | ½ medium | 60 |
| Spaghetti | 1½ tbs. | 20 | Potatoes (boiled) | ½ medium | 70 |
| Vermicelli | 1½ tbs. | 21 | Potatoes (mashed) | 1½ h. tbs. | 80 |
| Wheat flour | 1 tbs. | 20 | Potatoes, sweet (boiled) | ⅓ medium | 35 |
| Squash | 2 h. tbs. | 100 | |||
| Bread and Crackers | Turnips | 3 | 210 | ||
| Bread | 1 slice | 30 | Cooked Cereal | ||
| Breakfast biscuit, | Force | 5 h. tbs. | 18 | ||
| Huntley and Palmer | 3 | 18 | Farina | 2½ h. tbs. | 125 |
| Corn bread | 1 slice | 32 | Grape-Nuts | 1½ h. tbs. | 20 |
| Roll, Vienna | 3 | 18 | Hominy | 1½ h. tbs. | 90 |
| Zwieback | 1⅓ | 20 | Macaroni | 2 h. tbs. | 100 |
| Oatmeal | 2½ h. tbs. | 130 | |||
| Rice | ½ h. tbs. | 60 | |||
| Fruits | Shredded wheat biscuit | ¾ | 22 | ||
| Apple | 1 medium | 120 | Dried Fruit | ||
| Apricots | 2 large | 120 | Apples | 3 small | 22 |
| Banana (without skin) | ½ medium | 75 | Apricots | 3 large | 24 |
| Cherries | 90 | Currants | 1½ h. tbs. | 20 | |
| Currants | 5 h. tbs. | 120 | Dates | 3 | 19 |
| Grapefruit | ½ small | 150 | Figs | 1 large | 12 |
| Huckleberries | 3½ tbs. | 90 | Prunes | 2 large | 24 |
| Lemons | 2 medium | 210 | Raisins | 10 large | 23 |
| [Pg 386]Muskmelon | ⅓ | 300 | Milk and Cream | C.C. | |
| Nectarine | 1 | 100 | Buttermilk | 1½ tumbler | 300 |
| Olives (green) | 20 | 180 | Cream, 16% | 1½ tumbler | 300 |
| Orange | ½ large | 150 | Cream, 40% | 1½ tumbler | 300 |
| Peaches | 1½ medium | 150 | Koumiss | 1½ tumbler | 300 |
| Pear | 1 small | 100 | Whole milk | 1½ tumbler | 300 |
| Pineapple | 3 slices | 150 | |||
| Plums | 3 medium | 75 | Nuts | Grams | |
| Raspberries | 4½ h. tbs. | 120 | Almonds | 60 | 90 |
| Strawberries | 8 h. tbs. | 200 | Brazil | 30 | 180 |
| Watermelon | large slice | 300 | Chestnuts (roasted) | 15 | 40 |
| Cocoanut | 1 slice (3 × 2 in.) | 50 | |||
| Filberts | 100 | 110 | |||
| Peanuts | 40 | 80 | |||
| Pecans | 35 | 110 | |||
| Pistachios | 190 | 95 | |||
| Walnuts | 30 | 125 |
Caloric equivalent of 10 gm. steak in carbohydrate-free meat or fish
| Key: | |
| A | Gm. |
| B | Fat Gm. |
| C | Protein Gm. |
| D | Calories |
| Food | A | B | C | D |
| Steak | 10 | 1.0 | 2.4 | 19 |
| Roast beef | 5 | 1.4 | 1.1 | 18 |
| Tongue | 7 | 1.4 | 1.6 | 20 |
| Lamb chop | 5 | 1.5 | 1.1 | 18 |
| Roast lamb | 8 | 1.3 | 1.6 | 20 |
| Sweetbreads | 11 | 0.1 | 4.4 | 19 |
| Boiled ham | 7 | 1.4 | 1.5 | 19 |
| Fried ham | 5 | 1.7 | 1.1 | 20 |
| Roast pork | 9 | 0.9 | 2.6 | 19 |
| Bacon | 9 | 1.7 | 0.9 | 20 |
| Chicken | 10 | 1.0 | 2.4 | 19 |
| Duck | 9 | 1.3 | 1.8 | 19 |
| Guinea hen | 12 | 0.8 | 2.8 | 19 |
| Squab | 9 | 1.1 | 2.1 | 19 |
| Turkey | 7 | 1.3 | 2.0 | 20 |
| Bluefish | 13 | 0.6 | 3.5 | 20 |
| Halibut | 16 | 0.7 | 3.3 | 20 |
| Mackerel | 15 | 1.0 | 2.5 | 20 |
| Sardines in oil | 7 | 1.4 | 1.6 | 20 |
Approximate equivalent in 30 c.c. (1 oz.) of whisky in liquors containing 2 per cent or less of carbohydrates
| C.C. | Household Measure | |
| Gin, rum, brandy | 30 | 2 tbs. |
| Claret, Burgundy Hock, Rhine and Moselle wines | 130-160 | ¾ tumbler |
The following menus are suggested as meeting the carbohydrate-free diet requirements with a nutrient value of from 200 to 500 calories:
| Breakfast— | Black coffee (cream, 20 c.c.) | 30 grams | ||
| Bacon, 2 slices (1 oz.) | ||||
| Egg—1 | ||||
| Dinner— | Broth, 6 ounces | 180 grams | ||
| Steak, 1 small piece, 1⅓ oz. | 40 grams | |||
| Stewed tomatoes, 3⅓ oz. | 100 grams | |||
| Lettuce (lemon juice and olive oil) | 25 grams | |||
| Supper— | Broth | 180 grams | ||
| Whitefish | 40 grams | |||
| Spinach | 100 grams | |||
| Cabbage salad | 100 grams | |||
| Coffee | ||||
| Breakfast— | ½ grapefruit | |||
| 1 egg | ||||
| Bacon | 40 grams | |||
| Coffee | 50 grams | |||
| Cream | 20 c.c. | |||
| Dinner— | Broth | 180 c.c. | ||
| Kohl-rabi | 100 grams | |||
| Lettuce | 25 grams | |||
| Cheese salad | 50 grams | |||
| Roast beef | 40 grams | |||
| Coffee | ||||
| Butter | 5 grams | |||
| [Pg 388]Supper— | Cold chicken | 25 grams | ||
| Baked tomatoes | 100 grams | |||
| Water cress | 50 grams | |||
| Coffee | ||||
| Cream | 20 c.c. | |||
| Butter | 5 grams | |||
| Key: | |
| A | Protein Gm. |
| B | Fat Gm. |
| C | Carbohydrate Gm. |
| D | Calories |
| Material | Measure | A | B | C | D |
| Apple | 1 medium (150 gm.) | .5 | .50 | 16.0 | 70 |
| Almonds[149] | 10 small (10 gm.) | 2.0 | 5.00 | 2.0 | 63 |
| Apricots (dried) | 1 oz. (30 gm.) | 1.5 | .28 | 17.5 | 78 |
| Asparagus | 6 large stalks (74 gm.) | 1.3 | .14 | 2.5 | 16 |
| Bacon (raw)[149] | 4 slices, 6 in. long, 2 in. wide | 10.0 | 64.00 | 636 | |
| Bacon (cooked)[149] | 4 slices, 6 in. long, 2 in. wide | 10.0 | 32 to 46 | 388 to 468 | |
| Beef juice[150] | 100 gm. | 4.9 | .60 | 25 | |
| Beef roast[149] | 1½ in. × ⅛ in. | 6.0 | 7.00 | 89 | |
| Cheese (Neufchâtel)[149] | 1 cheese 2¼ in. × 1½ in. × 1¼ in. | 16.0 | 23.00 | 1.0 | 284 |
| Cream, gravity 16% | 1 glass (7 oz.) | 5.0 | 32.00 | 10.0 | 359 |
| Cream, 40% | 30 c.c. (2 tbs.) | .6 | 12.00 | 1.0 | 114 |
| Cracker (Uneeda biscuit) | 1 biscuit | 1.0 | .50 | 1.0 | 16 |
| Dry peptonoids[150] | 1 tbs. | 6.0 | 8.0 | 57 | |
| Egg | 1 medium (45 to 50 gm.) | 54.0 | 4.20 | 60 | |
| Fowl | 3½ oz. (100 gm.) | 19.3 | 16.30 | 224 | |
| Grapefruit | ½ | 5.0 | 20 | ||
| Ham (lean) | 50 gm. | 12.4 | 7.10 | 113 | |
| Lemon juice[151] | 3 tbs. (43 gm.) | 4.2 | 19 | ||
| Lemon Jelly[152] | 3 oz. (90 gm.) | 2.6 | 1.4 | 16 | |
| Milk (whole) | 1 glass (8 oz.) 240 c.c. | 7.9 | 9.60 | 10.0 | 158 |
| [Pg 389] Oatmeal[153] | 1 tbs. (50 gm.) | 1.0 | 6.0 | 33 | |
| Oatmeal | ½ cup (3.6 oz.) | 2.1 | .10 | 8.2 | 50 |
| Potato[153] (size large egg) | 1 (100 gm.) | 2.0 | .8 | 83 | |
| 5% vegetable[153] uncooked | 1 tbs. | 2.5 | 10 | ||
| 5% vegetable (boiled once) | 1 tbs. | 1.7 | 7 | ||
| 5% vegetable (boiled thrice) | 1 tbs. | 1.0 | 4 | ||
| Orange | 1 large | 1.7 | .20 | 22.7 | 100 |
| Orange[153] | 1 medium | 1.0 | 13.0 | 57 |
Increasing the Diet.—The following menus show the manner in which the diet is increased after the starvation treatment:
First Day
Approximately 150 grams of vegetables with tea or coffee; value: protein 2, fat trace, carbohydrate 4.
| Breakfast— | String beans | 20 grams |
| Celery hearts | 20 grams | |
| Lunch— | Spinach | 25 grams |
| Lettuce | 25 grams | |
| Supper— | Tomatoes | 25 grams |
| Cucumbers | 25 grams |
Second Day
Three eggs, 150 grams of 5% vegetables, tea or coffee; value approximately: protein 18, fat 12, carbohydrate, 4, calories 198.
| [Pg 390]Breakfast— | 1 poached egg | |
| Spinach or beet tops | 50 grams | |
| Coffee or tea | ||
| Dinner— | 1 hard-cooked egg | |
| String beans | 25 grams | |
| Lettuce | 25 grams | |
| Tea | ||
| Supper— | 1 soft-cooked egg | |
| Asparagus tips | 25 grams | |
| Tomatoes | 25 grams |
Third Day
Approximately 19 grams protein, 15 grams fat, 5 grams carbohydrate, 230 calories.
| Breakfast— | 1 egg | |
| String beans | 50 grams | |
| Tomatoes | 25 grams | |
| Coffee | ||
| Dinner— | Cauliflower | 50 grams |
| Celery | 50 grams | |
| Tea | ||
| Supper— | Asparagus | 75 grams |
| Lettuce | 50 grams |
Fourth Day
Approximately 26 grams protein, 15 grams fat, 10 grams carbohydrate, 279 calories.
| Breakfast— | 1 egg | |
| String beans | 75 grams | |
| Coffee with cream | 15 c.c. | |
| Dinner— | Tomato bouillon | 6 oz. (180 c.c.) |
| 1 egg | ||
| Asparagus | 75 grams | |
| Lettuce | 25 grams | |
| Tea | ||
| [Pg 391]Supper— | 1 egg | |
| Celery | 50 grams | |
| Cauliflower | 100 grams |
Fifth Day
Approximately 20 grams protein, 46 grams fat, 15 grams carbohydrate.
| Breakfast— | Egg omelet (1 egg) | |
| Butter | 10 grams | |
| Vegetable hash | 100 grams | |
| Coffee or tea | ||
| Cream | 15 grams | |
| Dinner— | Chicken broth | 180 c.c. |
| 1 poached egg | ||
| Tomatoes | 100 grams | |
| Tea | ||
| Supper— | 1 soft-cooked egg | |
| Spinach | 100 grams | |
| Cucumbers | 50 grams | |
| Tea or Coffee | ||
| Cream | 15 grams |
Sixth Day
Approximately 33 grams protein, 35 grams fat, 12 grams carbohydrate, 495 calories.
| Breakfast— | ½ grapefruit | |
| 1 egg | ||
| Butter | 5 grams | |
| Spinach | 50 grams | |
| Coffee | ||
| Cream | 15 grams | |
| Dinner— | Broth | 180 grams |
| Fish | 50 grams | |
| String beans | 100 grams | |
| Lettuce | 50 grams | |
| Asparagus | 50 grams | |
| [Pg 392]Supper— | 2 eggs | |
| Tomato, baked (1 medium) | 75 grams | |
| Cabbage salad | 75 grams | |
| Tea | ||
| Cream | 15 grams |
Seventh Day
Approximately 38 grams protein, 45 grams fat, 17 grams carbohydrate, 625 calories.
| Breakfast— | ½ grapefruit | |
| 2 eggs | ||
| Butter | 10 grams | |
| Coffee | ||
| Cream | 15 grams | |
| Dinner— | Beef broth | 180 grams |
| 1 lamb chop | 50 grams | |
| Cauliflower | 100 grams | |
| Tomato | 150 grams | |
| Lettuce | 50 grams | |
| Butter | 10 grams | |
| Supper— | 1 egg | |
| Tuna salad | 50 grams | |
| String beans | 100 grams | |
| Butter | 5 grams | |
| Tea |
Eighth Day
Approximately 32 grams protein, 16 grams fat, 20 grams carbohydrate, 625 calories.
| Breakfast— | 1 egg | |
| String beans | 100 grams | |
| Raw tomatoes | 100 grams | |
| Coffee | ||
| Cream | 15 grams | |
| [Pg 393]Dinner— | Chicken | 50 grams |
| Cabbage | 100 grams | |
| Asparagus | 100 grams | |
| Water-cress salad | 50 grams | |
| Tea | ||
| Supper— | 1 egg | |
| Greens | 100 grams | |
| Celery salad | 50 grams | |
| Tea | ||
| Cream | 15 grams |
The following menus are used after the diet has been more or less increased:
First Day
| Breakfast— | 1 soft-cooked egg |
| 2 slices of bacon | |
| 1 bran muffin, 5 gm. butter | |
| Coffee with 15 c.c. of 40% cream | |
| Lunch— | 6 oz. tomato bouillon |
| 2 oz. (60 gm.) roast lamb | |
| 60 gm. string beans | |
| 50 gm. lettuce and celery salad | |
| 25 gm. lemon jelly with 15 gm. cream | |
| Dinner— | 60 gm. chicken |
| 75 gm. asparagus | |
| 4 olives | |
| 50 gm. cauliflower | |
| 30 gm. ice cream | |
| 1 Lister roll, 5 gm. butter | |
| Black coffee |
Second Day
| Breakfast— | ½ grapefruit |
| 1 scrambled egg | |
| 1 Lister roll, 8 gm. butter | |
| Coffee with 15 gm. cream | |
| [Pg 394]Lunch— | 60 gm. baked halibut with 10 gm. parsley butter |
| 70 gm. cauliflower | |
| 50 gm. lettuce | |
| 1 Lister roll, 8 gm. butter | |
| Tea | |
| Dinner— | 6 oz. chicken broth |
| 60 gm. roast beef | |
| 75 gm. cabbage | |
| 75 gm. string beans | |
| 30 gm. coffee jelly with 15 gm. cream | |
| Black coffee |
Third Day
| Breakfast— | 1 soft-cooked egg |
| 2 slices bacon | |
| 1 Casoid flour and bran muffin with 5 gm. butter | |
| Coffee with 15 gm. cream | |
| Lunch— | 100 gm. cabbage |
| 40 gm. corned beef | |
| 50 gm. tomato salad | |
| 1 soya meal muffin, 8 gm. butter | |
| Tea | |
| Dinner— | 60 gm. beefsteak |
| 75 gm. asparagus | |
| 75 gm. spinach | |
| 30 gm. tomato aspic | |
| 30 gm. soft (diabetic) custard | |
| Black coffee |
Fourth Day
| Breakfast— | 1 scrambled egg with 20 gm. chipped beef |
| 1 Casoid flour muffin with 8 gm. butter | |
| Coffee with 30 gm. or less cream | |
| [Pg 395]Lunch— | 6 oz. tomato bisque |
| 60 gm. tuna fish salad | |
| 75 gm. vegetable hash | |
| 1 Lister roll, 8 gm butter | |
| Tea | |
| Dinner— | 60 gm. broiled chicken |
| 75 gm. string beans | |
| 75 gm. cauliflower | |
| 30 gm. tomato and celery salad | |
| 30 gm. wine jelly, with 15 gm. whipped cream | |
| Black coffee |
Fifth Day
| Breakfast— | ½ grapefruit |
| 1 soft-cooked egg | |
| 1 bran muffin with 8 gm. butter | |
| Coffee, 15 gm. cream | |
| Lunch— | 40 gm. broiled beefsteak |
| 75 gm. spinach | |
| 75 gm. boiled onion | |
| 1 soya meal muffin with 8 gm. butter | |
| Tea | |
| Dinner— | 6 oz. tomato bouillon |
| 80 gm. baked fish with parsley sauce | |
| 75 gm. Brussels sprouts with 5 gm. butter | |
| 1 Lister roll with 5 gm. butter | |
| Coffee jelly, 30 gm., with 15 gm. whipped cream |
Sixth Day
| Breakfast— | 1 poached egg |
| 2 slices bacon | |
| 1 bran and Casoid muffin with 5 gm. butter | |
| Coffee with 15 gm. cream | |
| [Pg 396]Lunch— | Ham omelet (1 egg, 1 tbs. cream, 15 gm. minced ham) |
| 75 gm. spinach | |
| 1 soya meal muffin with 8 gm. butter | |
| Tea |
A departure from the now almost universally used “Allen-Joslin Starvation Diet,” is seen in the “Newburg-Marsh High Fat Diet.”
The use of a high fat diet in the treatment of diabetes is based primarily on one fact—namely, that if the food eaten is not sufficient for the needs of metabolism, the body itself supplies the deficiency. Fat is used as long as it lasts, body protein being drawn upon for fuel when this is exhausted. It is of distinct advantage to the patient to have a diet of sufficient fuel value to run his body machine and permit him a moderate degree of exercise. For by this means he is not obliged to use his own body substance to carry on metabolic processes. We thereby avoid the condition of extreme emaciation (though it is to be emphasized that gain in weight is to be carefully guarded against) with its constant lowering of the general health.
The system of feeding consists of a series of four diets, examples and standards of which are given below. The diet is made up of protein on the basis of approximately ⅔ of a gram per kilogram of body weight at the time the patient leaves the hospital, a quantity of carbohydrate known to be well tolerated and the balance of the calories in fat.[154]
Diabetic Diet No. 1
| Key: | |
| A | Weight Gm. |
| B | Protein Gm. |
| C | Fat Gm. |
| D | Carbohydrate Gm. |
| E | Calories |
| 18-22 Proteins | |||||
| 12-15 Carbohydrates | |||||
| 800-1000 calories | |||||
| Food | A | B | C | D | E |
| Dinner: | |||||
| Fish | 50 | 8.9 | 5.1 | 82 | |
| with Butter | 10 | .1 | 8.5 | 77 | |
| Cabbage | 50 | .8 | .1 | 2.8 | 16 |
| with mayonnaise | .7 | 38.2 | 353 | ||
| Tomatoes | 100 | 1.2 | .2 | 4.0 | 23 |
| Broth—Tea | |||||
| Supper: | |||||
| String beans | 80 | 1.8 | .2 | 5.9 | 33 |
| with bacon | 10 | 1.0 | 6.5 | 62 | |
| Spinach soup— | |||||
| Spinach | 10 | .2 | .3 | 2 | |
| Cream | 10 | .2 | 4.0 | .3 | 38 |
| Broth to fill bowl | |||||
| Celery | 20 | .2 | .7 | 4 | |
| Broth—Tea | |||||
| Breakfast: | |||||
| Omelet— | |||||
| 1 egg | 6.7 | 5.2 | 74 | ||
| with butter | 10 | .1 | 8.5 | 77 | |
| Coffee | |||||
| 21.9 | 76.5 | 14.0 | 842 | ||
Diabetic Diet No. 2
| Key: | |
| A | Weight Gm. |
| B | Protein Gm. |
| C | Fat Gm. |
| D | Carbohydrate Gm. |
| E | Calories |
| 25-30 Proteins | |||||
| 18-22 Carbohydrates | |||||
| 1200-1600 calories | |||||
| Food | A | B | C | D | E |
| Dinner: | |||||
| Pork chops | 60 | 10.0 | 18.0 | 202 | |
| Cabbage | 100 | .2 | .3 | 5.6 | 32 |
| (Use pork drippings) | |||||
| Spinach | 100 | 2.1 | .3 | 3.2 | 24 |
| with butter | 20 | .2 | 17.0 | 154 | |
| Broth—Tea | |||||
| Supper: | |||||
| Asparagus salad— | |||||
| Lettuce | 10 | .1 | .3 | 2 | |
| Asparagus | 80 | 1.2 | .1 | 2.1 | 13 |
| Mayonnaise | 50 | .7 | 38.8 | 338 | |
| Tomatoes | 100 | 1.2 | .2 | 4.0 | 23 |
| with butter | 10 | .1 | 8.5 | 77 | |
| Nut charlotte— | |||||
| Walnuts, chopped | 10 | 1.8 | 6.4 | 1.3 | 70 |
| Cream | 50 | 1.1 | 20.0 | 1.5 | 190 |
| Broth—Tea | |||||
| Breakfast: | |||||
| Bacon | 20 | 2.1 | 13.0 | 125 | |
| with 1 egg | 6.7 | 5.2 | 74 | ||
| Coffee with cream | 30 | .7 | 12.0 | .9 | 114 |
| 28.2 | 139.8 | 18.9 | 1438 | ||
Diabetic Diet No. 3
| Key: | |
| A | Weight Gm. |
| B | Protein Gm. |
| C | Fat Gm. |
| D | Carbohydrate Gm. |
| E | Calories |
| 30-35 Proteins | |||||
| 25-30 Carbohydrates | |||||
| 1600-2000 calories | |||||
| Food | A | B | C | D | E |
| Dinner: | |||||
| Beef tenderloins | 80 | 13.0 | 19.5 | 227 | |
| with butter | 10 | .1 | 8.5 | 77 | |
| Asparagus | 100 | 1.5 | .1 | 2.8 | 18 |
| with butter | 10 | .1 | 8.5 | 77 | |
| Squash | 100 | 1.4 | .5 | 9.0 | 46 |
| with butter | 10 | .1 | 8.5 | 77 | |
| Broth—Tea | |||||
| Supper: | |||||
| String bean salad— | |||||
| Lettuce | 10 | .1 | .3 | 2 | |
| String beans | 50 | 1.1 | .1 | 3.7 | 26 |
| Pimento | 10 | .2 | .4 | 2 | |
| Onion | 10 | .2 | 1.0 | 5 | |
| Mayonnaise | 30 | .5 | 23.3 | 228 | |
| Tomatoes | 120 | 1.4 | .2 | 4.8 | 28 |
| with butter | 20 | .2 | 17.0 | 154 | |
| Chocolate pudding— | |||||
| Cream | 100 | 2.2 | 40.0 | 3.0 | 381 |
| Cocoa, ½ tsp | 1 | .2 | .3 | .4 | 5 |
| Broth—Tea | |||||
| Breakfast: | |||||
| Bacon | 30 | 3.2 | 19.4 | 187 | |
| with 1 egg | 6.7 | 5.3 | 74 | ||
| Coffee with cream | 30 | .7 | 12.0 | .9 | 114 |
| 32.9 | 163.2 | 26.3 | 1728 | ||
Diabetic Diet No. 4
| Key: | |
| A | Weight Gm. |
| B | Protein Gm. |
| C | Fat Gm. |
| D | Carbohydrate Gm. |
| E | Calories |
| 50-60 Proteins | |||||
| 30-40 Carbohydrates | |||||
| 2000-2500 calories | |||||
| Food | A | B | C | D | E |
| Dinner: | |||||
| Veal steak (roast) | 100 | 19.9 | 10.8 | 177 | |
| Onions | 126 | 1.9 | .4 | 11.9 | 49 |
| with cream | 50 | 1.1 | 20.0 | 1.5 | 190 |
| Tomatoes | 150 | 1.8 | .3 | 6.0 | 35 |
| with butter | 30 | .3 | 25.5 | 231 | |
| Fruit salad— | |||||
| Lettuce | 10 | .1 | .3 | 2 | |
| Celery | 50 | .6 | 1.6 | 9 | |
| Grapefruit | 80 | .6 | .2 | 8.1 | 37 |
| Whipped cream | 30 | .7 | 12.0 | .9 | 114 |
| Tea—Broth | |||||
| Supper: | |||||
| Cream of celery soup— | |||||
| Celery | 50 | .6 | 1.6 | 9 | |
| Cream | 75 | 1.6 | 30.0 | 2.2 | 285 |
| Broth to fill bowl | |||||
| Boiled ham | 30 | 6.1 | 6.7 | 85 | |
| Custard— | |||||
| 2 egg yolks | 4.7 | 10.0 | 109 | ||
| Cream | 90 | 2.0 | 36.0 | 2.7 | 343 |
| Tea | |||||
| Breakfast: | |||||
| Eggs (2) | 13.4 | 10.5 | 148 | ||
| with butter | 30 | .3 | 25.5 | 231 | |
| Coffee with cream | 20 | .4 | 8.0 | .6 | 76 |
| Broth | |||||
| 56.1 | 195.9 | 37.4 | 2130 | ||
[Pg 401] Nurse’s Directions for Collecting and Testing the Urine in Diabetes Mellitus.—The first urine voided in the morning at 7 A.M. should be thrown away, after which the entire quantity during the ensuing twenty-four hours, including that at 7 A.M. the following morning, should be collected in a thoroughly clean, wide-mouth bottle sufficiently large to contain the entire quantity. This should be kept in a cool place to prevent decomposition. After the urine has been measured, four or five ounces are removed for testing purposes. There is no necessity for having an elaborately equipped laboratory for making the simple tests of the diabetic urine. The nurse is only required to make the simple tests, leaving the more elaborate one for the physician. The articles necessary for these tests must be kept perfectly clean in order to make the tests accurate. The bottle in which the urine is collected must be washed and sterilized daily before the collection begins. One small three-inch white enameled or porcelain dish, one 10 c.c. graduated pipette, 6 test tubes, 1 small alcohol lamp or Bunsen burner, 1 box of sodium carbonate, 1 box talcum, and the reagents necessary for making the test, namely, Benedict’s solution, Fehling’s solution, and Haines’s solution.
Diabetes Mellitus is a disease in which the body becomes more or less unable to utilize the sugars and starches, consequently there is an abnormal amount of glucose in the urine.
Manufacture of Sugar in the body from other food constituents besides carbohydrates has been proved with regard to proteins, hence the intake of nitrogenous substances must be restricted in diabetes—to a less extent, however, than the sugars and starches.
Acetone Bodies.—Diacetic acid, oxybutyric acid, and [Pg 402] acetone develop in diabetes as a result of the breaking down of the fats and the lack of certain neutralizing agents found chiefly in carbohydrate foods.
Acidosis is a form of intoxication due to the retention of these toxic acids in the body. If not combated and overcome, it will result in the diabetic coma which is fatal in so many cases.
Diet Treatments.—The best known treatments are those devised and used by Drs. Allen and Joslin “The Starvation Treatment for Diabetes Mellitus,” and the “High Fat Diet” formulated by Drs. Newburg and Marsh. All cases cannot be handled alike and it is for the physician to determine the treatment calculated to give the best results in the definite case.
Training for Diabetic Nursing.—So much depends upon the administration of the treatment in this pathological condition that in many hospitals special training is being given to the nurses in the care of diabetic patients that they may be able intelligently to carry out the necessary régime, both in the hospital and in private practice.
Symptoms.—She must be able to recognize symptoms both from the findings resulting from the urinalysis and from those manifested otherwise by the patient.
The Record.—She must keep an absolute record of all that occurs during the course of treatment and instantly report any unusual happening.
Urine Tests.—It is advisable to make the tests in the morning; those for sugar and diacetic acid should be made every day or, in some cases, every other day, as directed by the physician, and those for ammonia and albumen about once a week.
Weighing the Patient.—Patient should be weighed each day before breakfast, and the weight of the clothes also carefully recorded separately.
[Pg 403] The Bowels must move daily, even if it is necessary to resort to mild laxatives or an enema.
Formulating and Calculating the Dietary.—The menus of the day must be formulated and the chemical composition and nutrient value of the foods calculated. The vegetables belonging to the five per cent. group should be in readiness and the amount to be used weighed after they have been boiled in clean, separate water to reduce their carbohydrate content still further.
Commercial Diabetic Foods.—It may be well to mention the danger of putting faith in the so-called diabetic foods so widely advertised. Some of these foods are of undoubted worth, but it is never safe for the nurse or the patient to judge of the merits of the various diabetic foods without first knowing their chemical composition, and not even then without the definite directions from the physician.
Diabetic Flours.—The diabetic flours used in the recipes included in this text have been approved by some of the leading specialists in diabetes in this country, but the nurse should not include them in the diet for her patient unless they are prescribed by the physician in charge.
(a) Outline test diets for determining the severity of the disturbance.
(b) Give examples of diets used in testing for tolerance of carbohydrates, fats, proteins.
(c) Give an example of a diet order showing the use of the high fat method of feeding. Why is it used?
[137] Allen’s Paradoxical Law, quoted from “Treatment of Diabetes Mellitus,” p. 18, by Joslin.
[138] “Treatment of Diabetes Mellitus,” p. 305, Joslin.
[139] “Food for the Sick,” by Strouse and Perry.
[140] Courtesy of Dr. Joslin and Thomas Groom & Co., Boston.
[141] The giving of coffee or clear broth, with or without whisky, does not materially affect the starvation and serves to make the patient more comfortable during this trying period.
[142] Dr. Joslin has given a very complete schedule in his “Treatment of Diabetes Mellitus,” from which the above schedule is taken.
[143] Hill and Eckman’s “Starvation (Allen) Treatment of Diabetes.”
[145] Table used by Dr. Joslin in his treatment of diabetes mellitus. It is convenient, and many changes in the diet may be made by substituting one food for another of like carbohydrate content. This table can be purchased on cards from Thomas Groom & Co., Boston, Mass.
[146] Table devised by H. O. Mosenthal showing accessory diets rich in carbohydrates. “Medical Clinics of North America,” July, 1917.
[147] “h” represents household measure.
[148] Mosenthal: “Medical Clinics of North America,” July, 1917.
[149] “Starvation Treatment of Diabetes,” by Hill and Eckman.
[150] “Practical Dietetics,” by Alidia Pattee.
[151] “Food for the Sick,” p. 62, by Strouse and Perry.
[152] Sweetened with saccharin.
[153] “Starvation Treatment of Diabetes,” by Hill and Eckman.
[154] Courtesy of R. Eckman and D. M. Stewart, University of Michigan Hospital, Ann Arbor, Michigan.
Much of the so-called biliousness from which the human family is so prone to suffer is nothing more or less than one of Nature’s danger signals by means of which man may understand that some part of the delicate organism called the human body is being overworked. Close investigation of these conditions has proved that it is the liver which has been overtaxed, in many cases to such an extent that in a measure it slows down, as any overtaxed machine will do, and has become clogged with material which, owing to its condition, it is not able to prepare properly and send out on time.
Work of the Liver.—When one considers the vast amount of work performed by this organ, one marvels that so little trouble is manifested. In another part of this text the functions of the liver were defined. It was found to be the largest secretory organ in the body, producing a constant supply of bile by means of which the fats were dissolved and the digestion and absorption of the other food materials facilitated. We likewise found that the greater part of the fuel foods was transformed within this organ into available energy, either for immediate or future use.
As a Detoxifying Agent.—To the liver must also be credited the detoxifying of the various poisons produced within the body during the process of metabolism or brought in by way of food. Too much cannot be said as to the value of the liver in this respect, the importance of which is made known as soon as anything happens to the organ to put it even temporarily out of commission.
[Pg 405] Causes of Liver Disorders.—Is it any wonder, then, that with such abuses as overeating and drinking, especially of those foods rich in fats and carbohydrates which depend upon the liver for their availability in the body, Nature cries aloud for help and for the comparative rest of this, her largest organ?
The taking of alcohol in excess has been found to bring about tissue changes in the liver. Hence it must be avoided by individuals with a tendency to biliousness or to any disease in which the liver is involved.
The Bowels.—The bowels are as a rule constipated, and one of the first means of relief is the overcoming of this condition. The method of doing this depends upon the individual, and the treatment must be decided on by the physician.
Dietetic Treatment.—The dietetic treatment consists in abstaining from food or reducing the amount to a minimum while the attack lasts and while the intestines are being thoroughly emptied. All stagnant material which has clogged the bowels and which has been subjected to the activities of putrefactive bacteria must be gotten rid of. The diet must be especially low in fat. Oyster or clam broth, soft-cooked eggs, toast, cereal, or rice, with a little milk instead of cream and very little sugar, tea, and baked apple or stewed prunes are given.
Convalescent Diet.—After the attack the diet may be gradually increased until it is again normal. Moderation must be observed in the amount of food eaten; no highly seasoned or spiced foods, pickles, or condiments, such as peppers, mustard, or horseradish, should be taken. Salads should be dressed without oil. Lean beef, lamb chops, fish, chicken, sweetbreads, quail, squab, eggs (except fried or hard cooked), green vegetables (except radishes, onions, water-cress, and celery) in abundance, a small amount of potato, rice, or tapioca, fresh and cooked fruit with little, if [Pg 406] any sugar, junket, custards, fruit jellies, weak tea and coffee should constitute the diet. Certain individuals find that milk increases the tendency to constipation; this is probably due to the small amount taken; large quantities do not as a rule produce this effect. Buttermilk, koumiss, and modified milk are advised in severe cases.
Diet for Constipation.—Individuals inclined to biliousness should endeavor to overcome the constipation which is one of the most prominent features. This is done by proper diet more successfully than by drugs (cathartics): bran bread, vegetable soup, fresh fruit, stewed fruit, fruit beverages, plenty of water. The following menus are suggested:
| Breakfast— | Stewed prunes |
| Oatmeal with milk (no sugar) | |
| Weak tea or coffee | |
| Toast (milk toast or dry toast) | |
| Lunch— | Tomato soup |
| 1 small baked potato | |
| 1 lean lamb chop (broiled) or a poached egg on toast | |
| Cup of weak tea | |
| Dinner— | Vegetable soup |
| 1 slice of lean, rare beef (cut from the inside of the roast) | |
| Spinach | |
| Rice | |
| Lettuce and tomato salad | |
| Lemon jelly | |
| Breakfast— | Grapefruit |
| Hominy with milk | |
| Poached egg on toast | |
| Weak coffee (milk and little sugar) | |
| [Pg 407]Lunch— | Cream of green pea soup |
| Tomato jelly | |
| Broiled sweetbreads | |
| Weak tea | |
| Toast | |
| Dinner— | Small portion of lean lamb or chicken |
| Boiled or mashed potatoes | |
| String beans | |
| Sliced tomatoes | |
| Prune whip |
Advice to Patient.—The above menus are merely suggested. The diet may be selected from the list of foods already mentioned. The patient must be warned against overeating and drinking. Pastry, rich cakes and puddings, confectionery, gravies, etc., must be avoided. In certain individuals beer will induce a bilious attack. By them it should be avoided.
The cause of this disease and the stage in which it exists must determine the treatment necessary. However, it matters not what produced the disease, whether it is the result of alcoholism, syphilis, etc., the diet plays an important rôle in its cure.
The Diet.—The diet in this disease, as in any other, must be determined by the condition of the patient. Unfortunately, many patients do not know of their condition until the disease is well advanced and symptoms of obstruction are prominent. A study of these must be made before the diet can be formulated. When the symptoms are mainly those arising from disturbed digestion of the stomach and intestines, without kidney or heart complication, the diet for chronic gastritis is used.
Restricting the Fluids.—When the heart is involved, it [Pg 408] is sometimes found necessary to restrict the fluids (dry diet) to 1 quart (about 1000 c.c.) per day. The Karell Cure has been used advantageously in many of these cases. In cases where the kidneys are involved, the diet will depend upon the condition of these organs.
Restricting the Diet.—The diet in any case must be restricted. Individuals with a tendency to cirrhosis and those coming of a family in which liver diseases are frequent should be especially warned about the dangers of overeating and drinking. Alcohol should be avoided especially by such individuals. They should keep their diet simple in character and moderate in amounts.
Avoidable Foods.—All foods, such as condiments and spices, meat extracts, the outside browned portions of roasted meat, alcoholic beverages, which exert a stimulating or irritating effect upon the liver, should be studiously avoided and the fats and carbohydrates restricted, since, as it has already been demonstrated, it is upon the liver that the body depends for the preparation of these substances for their utilization. When, for example, the flow of bile is lessened, an incomplete emulsification of the fats exists and the fatty acids which are highly acid in character cannot be efficiently dissolved or neutralized, or when the liver is diseased and for this reason the conversion of glycogen into glucose is interfered with, the utilization of the carbohydrate foods is thus impaired.
Factors Influencing Their Formation.—According to Friedenwald and Ruhräh[155] the two factors that in all probability exert the most influence on the formation of gallstones are the stasis of bile and the inflammation of the bile passages and gall bladder.
Dietary Rules.—There are certain dietary rules which [Pg 409] should be observed by all persons who have had gallstone attacks. These are (1) to prevent stasis of bile, (2) to avoid fats. Everything should be done to prevent the formation of the stones, and this can only be accomplished by observing these rules. The flow of bile must be free; this is encouraged by keeping the intestinal tract in good condition.
Stimulating Peristalsis.—Peristalsis must not be allowed to become sluggish, for it is only during the process of digestion when the food mass passes along the intestinal canal that there is an ejection of bile into the intestines. When the passage is abnormally slow the bile is in a measure dammed back with a formation of gallstones as a result. The restriction of the fats has already been discussed in another part of the chapter. It has been demonstrated that these substances have a chemical influence upon the formation of gallstones as well as upon the intestinal stasis which leads to their formation.
Dietetic Treatment.—Hence the diet should be so directed as to (1) increase the flow of bile, and (2) to avoid all foods that are liable to cause indigestion which may bring about putrefaction in the intestinal tract and a consequent irritation and inflammation of the bile passages and gall bladder.
The meals should be regular and an abundant diet advised to increase the flow of bile and stimulate peristalsis in the intestines.
Exercise.—Exercise is especially recommended. Horseback riding, swimming, rowing, golf, and tennis are especially valuable in forcing the bile from the gall bladder and liver.
The Clothing.—The clothing should be loose enough to be perfectly comfortable. Certain cases of gallstone attacks in women have been said to have been traced to tight lacing, which interfered with the normal flow of the bile.
[Pg 410] The Bowels.—Constipation should be avoided, and the diet should be directed with this point in view. The meals must be frequent, ranging from four to six a day. In this way only is the flow of bile encouraged. The breakfast should be ample in order to utilize the bile secreted in the night season. With all this, care must be observed not to give more food than can be adequately handled by the digestive apparatus, since food which is not digested becomes a prey to the actions of the putrefactive bacteria which infest it, and the toxic substance thus formed produces the very result which all of our efforts are directed to prevent.
Available Foods.—The following foods low in fats may be used in formulating the diet:
Soups: Meat broth (made from lean meat) from which all the fat has been removed.
Meats: Lean beef, lamb, chicken, squab, quail, lean fish (in small quantities and not too frequently).
Green vegetables: Except peas and carrots; beets and turnips may be taken sparingly.
Fruits: Oranges, lemons, grapefruit, and unsweetened stewed fruit.
Cereals: Wheat cereals, oatmeal, rice, and tapioca in moderation.
Bread: Whole wheat, white, rye, and graham bread, toast, and crackers.
Fluids: Weak tea and coffee (without cream, and a little sugar), orange and lemonade, mineral waters, water, skimmed milk, whey.
Eggs: (except hard-cooked or fried).
Desserts: Fruit gelatin, fruit whips, raw or stewed fruit.
Avoid the following foods: Fats, oils, mutton, liver, brains, sardines, and caviar, oily fish, rich gravies and sauces, sweet fruit, peas, carrots, condiments and spices, pastry and confectionery, pickles, alcoholic beverages. Restrict [Pg 411] carbohydrates, yolks of eggs, milk (cream must be skimmed off if too rich).
I
| Breakfast— | Baked apple with milk |
| Cream of wheat with milk | |
| Weak coffee or tea | |
| Dry toast | |
| 11:30 A.M.— | 6 oz. orange juice, 1 egg white |
| Dinner— | Beef broth (well skimmed) with crackers |
| Rice | |
| Stewed pears | |
| Weak tea | |
| Toast or rolls | |
| 3:30 P.M.— | Albumenized fruit juice with crackers |
| Supper— | Wheatena with milk |
| Milk toast | |
| Stewed prunes | |
| Toast and tea | |
| 9 P.M.— | Well-skimmed chicken broth with crackers |
II
| Breakfast— | Stewed apples with milk |
| Milk toast | |
| Coffee without cream | |
| 10:30 A.M.— | Well-skimmed broth with crackers |
| Dinner— | Tomato bouillon with crackers |
| Baked potato—1 small potato | |
| Purée of spinach | |
| Orange gelatin | |
| Toast | |
| [Pg 412]3 P.M.— | Albumenized lemonade |
| Supper— | Oatmeal or cream of wheat with milk |
| Toast | |
| Tea | |
| Stewed fruit | |
| 9 P.M.— | Well-skimmed broth with crackers |
III
| Breakfast— | Grapefruit |
| Oatmeal with milk | |
| Toast | |
| Weak coffee | |
| 10:30 A.M.— | Orangeade with graham crackers |
| Dinner— | Cream of spinach soup (skimmed milk) |
| Small piece of the breast of chicken | |
| Mashed or boiled potatoes | |
| Asparagus on toast | |
| Sliced oranges | |
| 3:30 P.M.— | Well-skimmed broth with crackers |
| Supper— | Farina or cream of wheat or wheatena, with milk |
| Baked potato | |
| Baked apple with milk | |
| Toast and tea | |
| 9 P.M.— | Albumenized orange juice |
IV
| Breakfast— | Sliced oranges |
| Oatmeal | |
| Toast | |
| Coffee | |
| [Pg 413]10:30 A.M.— | Beef gruel, 6 oz. |
| Dinner— | Cream of asparagus soup, skimmed milk |
| Thin slice of roast beef or whitefish | |
| Rice or potatoes | |
| Tender string beans | |
| Fruit | |
| Toast | |
| Buttermilk | |
| 3:30 P.M.— | Orangeade |
| Supper— | Stewed fruit with puffed wheat or rice |
| Milk toast | |
| Tea | |
| 9 P.M.— | Broth |
Functions of Liver.—To transform fuel foods into available energy; to detoxify those poisonous substances produced as the result of metabolism of body tissue or brought in in food, and to select those available for use; to secrete bile.
Factors Influencing Disorder of Liver.—Errors in diet: (a) overeating; (b) excessive drinking; and (c) unbalanced diet, especially as regards the amount of fats and carbohydrates in the diet.
The Bowels, in most of the disturbances affecting the liver, become constipated, thus causing much additional work on the part of the liver in handling the products produced as the result of putrefactive bacteria upon the accumulated mass in the colon.
Tissue Changes in the liver have been caused by the taking of alcohol, which should therefore be avoided by all individuals having any disease involving the liver and by those with a predisposition to liver disturbances.
[Pg 414] Exercise and Lack of Exercise are potent factors in the treatment of conditions involving the liver. First, because the liver requires exercise to enable it to empty itself more completely and assure a free flow of bile; second, because exercise directly affects the energy output of the body, causing an increased rate of metabolism and a better utilization of the food ingested. Lack of exercise acts in exactly the opposite direction, and it has been found that with the majority of patients suffering from diseases of the liver too little exercise and too much food are at the bottom of the trouble.
Dietetic Treatment in the majority of diseases affecting the liver is much the same. The keynote in each is a balanced diet. Constant overeating and excessive drinking have proved the foundation of the majority of such diseases, especially of the bilious type, while an excess of fat and carbohydrates in the diet lead to the more serious disorders.
Biliousness requires abstinence from food for a short period and a cleansing of the entire gastro-intestinal tract, the measures being directed by the physician. After the bilious symptoms have subsided, a simple, well-regulated diet should be established, in which no rich foods of any sort are allowed. All condiments and spices which have an astringent effect upon the bowels are strictly prohibited, and alcoholic beverages had best be eliminated from the diet.
Cirrhosis of the liver is apt to be insidious in its development, taking a firm hold before the character of the disorder is discovered. Dietetic treatment of this disturbance is most important and should be directed toward overcoming not only the liver symptoms but other symptoms as well.
Gastro-intestinal Disturbances, manifested in cirrhosis of the liver, are treated by the diet used in chronic gastritis (see p. 250).
Heart Symptoms sometimes occur during the course of [Pg 415] the disease and require especial attention to the diet. The fluids at times must be restricted, in which case a modification of the Karell Cure will prove valuable (see p. 342).
Kidney Complications develop in a certain percentage of cases, and it then becomes necessary to institute one of the various diets devised to meet the needs of those special conditions (see Chapter XVIII).
Restricting the Diet will be found to be necessary for those individuals showing a tendency to cirrhosis, also for those in whose family diseases of the liver are of frequent occurrence. Such individuals should be warned of the dangers arising from overindulgence in food or alcoholic beverages.
Prohibited Foods are those which by reason of their astringent qualities favor the development of constipation, such as condiments and spices; those foods which exert a stimulating and irritating effect upon the liver and bile passages, such as alcohol, malt extractives, etc.; and fats and carbohydrates in excessive quantities, on account of the extra amount of work required of the liver in order to make them available in the body.
Gallstones develop as the result of inflammation or clogging of the bile passages.
Treatment is dietetic in character and is directed toward relieving or preventing inflammation in the bile passages, also in stimulating the flow of bile in order that it may not become sluggish and thus give rise to the development of the gallstones.
The Fats, therefore must be restricted in the diet, as they, more than any of the other food constituents, favor the above conditions.
Peristalsis in the intestinal tract must be stimulated to facilitate a free flow of bile, which will not occur where the movements are sluggish. Stasis of the bile must be prevented or stones will be apt to form.
[Pg 416] Dietetic Treatment for gallstones is therefore directed to increase the flow of bile and to avoid the inflammation of the gall bladder and bile passages which may result from the product of intestinal putrefaction.
The Diet consists of foods simple in character, low in fats, but abundant in quantity, in order to prevent constipation. It must be selected carefully that digestional disturbances may not develop.
The Meals should be frequent, from four to six a day, in order to encourage a free flow of bile.
Breakfast should be ample in order that the bile secreted and accumulated during the night may be utilized as soon as possible.
Constipation must be avoided, and the foods particularly adapted to prevent or overcome this condition should have a prominent place in the diet. Any accumulation of unabsorbed food in the lower intestines becomes a breeding ground for putrefactive bacteria, the product of whose activity imposes a serious tax upon an already overworked organ.
(a) Formulate a diet for a patient suffering from gallstones. Outline method of administration.
(b) List available foods for diets used in disturbances of the liver. List the foods to be avoided in such cases.
[155] “Diet in Health and Disease,” p. 399, by Friedenwald and Ruhräh.
Gout is a constitutional disease characterized by an inflammatory condition of the joints. It is caused by or associated with a retention of uric acid in the blood. Gout is also characterized by the deposit of uric acid or sodium salts which occurs in different parts of the body, the joints, the lobe of the ear, the knee and the elbow being common points where the deposit of these salts ordinarily occurs. The amount of uric acid is lessened in the urine in cases of true gout, except in acute attacks, and in this way it is distinguished from the so-called goutiness in which a urinalysis shows an excess of uric acid. According to Strouse, this excess of uric acid in the urine “means a physical-chemical change in the urine and is quite different from the small amount usually excreted.”[156]
Source of Uric Acid.—In man the uric acid which is eliminated in the urine is derived from two sources. It may be taken with the body as purins in food, in which case it is spoken of as being an “exogenous” product, or it may be formed in the body from the breaking down of the nucleoproteins (the highly nucleated cells of the glandular organs particularly). When the uric acid is formed in this manner as the result of the metabolism of the body tissues, it is known as “endogenous.” In the normal body approximately one-half of the uric acid formed is oxidized, while the remaining half is eliminated from the body by way of the urine.
Elimination of Uric Acid.—In gout such is not the case, the body loses to a certain extent the ability to eliminate [Pg 418] the uric acid, hence it is retained within the body, causing an excess in the blood stream, and it is this excess uric acid in the blood which causes the acute attacks and general pain and discomfort which inevitably occur in chronic gout.
Purin-bearing Foods as Sources of Uric Acid.—Formerly no difference was made in food; all were supposed to cause uric acid formation, but with the exhaustive investigation of food materials this sweeping condemnation has been to a great extent removed or narrowed down to a few foods, those rich in purins being the chief offenders.
Chief Causes of Gout.—Without a doubt, overeating, overindulgence in alcoholic stimulation, lack of exercise, etc., are chiefly to blame for the large percentage of the cases, but upon investigation it will be seen that those individuals are as a rule large protein eaters and that their mode of living is not such as to assist the body in throwing off the poisons which form as the result of their self-indulgence.
Rules to Combat Gout.—To successfully combat the retention of a large percentage of uric acid in the blood there are certain definite rules to be observed: (1) The general diet must be reduced not only in amount but also in purin-bearing foods; (2) All foods which are liable to cause digestional disturbances, with the attending evils of intestinal putrefaction and constipation, must be avoided.
Alcohol in Gout.—If the patient is accustomed to alcoholic stimulants and has been in the habit of taking them constantly for years, the amount of alcohol consumed daily must be radically reduced and only the amount prescribed by the physician taken. Alcohol without a doubt assists in the retention and increases the difficulty of uric acid elimination by the body. In view of the present knowledge of the cause and effect of uric acid in the body, the treatment of gout is directed with the object of relieving the condition (1) by facilitating the elimination of uric [Pg 419] acid from the body, and (2) by so regulating the diet as to exclude as far as possible those purin-bearing foods which, by reason of their chemical composition, augment the general amount of uric acid formed within the organism.
In gout, as in other abnormal conditions, no set rule can be laid down to cover the treatment of every case. The individual must be taken into consideration, his daily habits studied and the extent and character of the disease known before it is possible to prescribe a treatment or formulate a diet which would adequately meet his needs under the existing conditions.
Obesity and Glycosuria.—Gouty individuals often become obese and show evidences of glycosuria. Consequently it is important to regulate the carbohydrates as well as the purin-bearing foods in the diet. Only the simplest foods are permissible. In acute attacks it has been found that milk and alcohol cause less disturbance than meat and alcohol. While the acute symptoms exist all meat should be avoided and the daily allowance of alcohol cut down. Tea and coffee both contain purins and should be avoided while the acute stage of the disease continues. Cereal coffee, hot water tea, hot milk or buttermilk may be substituted.
Purin-free Diet.—A purin-free diet is advisable during the acute attack. The following is a sample menu of such a diet:
| Breakfast— | Banana, apple, grapefruit, orange or peach, etc. |
| Cereals: farina, hominy, or cream of wheat with cream and sugar | |
| 1 egg, soft-cooked | |
| Buttered toast | |
| Cereal, coffee with sugar and cream or hot water tea (milk and hot water) with cream and sugar | |
| [Pg 420]Lunch or Dinner— | Poached egg on toast, 1 large baked potato with butter, 1 mold of fruit jelly with cream |
| Supper— | Rice and butter, bread or toast with hot milk |
| Apple sauce with cream |
| Purin Per Cent. | ||
| Cocoa | contains | 1.00 per pint |
| Tea | “ | 1.20 per pint |
| Coffee | “ | 1.70 per pint |
Purins are soluble in water, hence those foods that are boiled contain less than those prepared by other methods of cookery.
Foods More or Less Condemned.—Salt has a tendency to bring about a deposit of sodium urates in the body, and for this reason should be sparingly used in the preparation of the diet. Alkaline waters are inclined to produce a like result, consequently should be avoided by the gouty individual. Condiments and spices are conducive to constipation, a condition to be avoided if possible under the circumstances. Certain physicians prohibit the use of oranges in the diet of gout, while others do not. Strawberries are likewise condemned and should be eliminated from the diet for both chronic and acute gout.
Diet in Chronic Gout.—In chronic gout it is necessary to maintain the general health of the patient by a well-balanced diet. This is not difficult even if the dietary is so regulated as to be well within the limits of his energy requirements. It is necessary to limit the purin-bearing foods. Meats are used sparingly and these should be boiled rather than roasted or broiled. Eggs and cheese and milk should be substituted for at least part of the regular allowance of meat.
Exercise and Massage.—The patient should be recommended to take a certain amount of mild exercise in the [Pg 421] open air, or massage if he is accustomed to living an indoor life or is confined to office work. He must be warned against overindulgences of all kinds, especially of overeating and drinking. A glass or two of hot water before breakfast is recommended.
Treatment of Obesity.—The treatment of obesity when occurring in gouty patients is much like that used in other conditions. Ebstein regards obesity under such circumstances as an unfavorable symptom. He advises a reduction in the carbohydrates to the smallest possible amount and allows meat and fats in the diet.
Allowable Foods.—The following foods are practically purin-free and may be used in the diet of gout:[157] Milk, cheese, butter, eggs, nuts, gelatin, fruits, sugar, breads made with white flour, cereals, cream of wheat, farina, rice, hominy, tapioca, cornstarch, potatoes and other root vegetables, green vegetables, except asparagus, spinach, and all fats.
Avoidable Foods.—The following foods are rich in purins and should be avoided in the diet for gout: Sweetbreads, liver, kidneys, beef, mutton, veal, pork, turkey, chicken, goose, rabbit, duck and other game, fish, with the exception of cod, sardines, and anchovies, tea, coffee, and cocoa.
The following list shows the purin content of some of the above-mentioned foods. The purins are computed by Hall as follows: 1 kilogram contains,
| Grams Purin | |
| Milk | |
| Butter | |
| Eggs | |
| Cheese | |
| Farina | |
| Rice | |
| Hominy | |
| Potato | 0.02 |
| Flour | |
| Bread | |
| Cauliflower | |
| Eggplant | |
| Cabbage | |
| Lettuce | |
| Sugar | |
| Peas | 0.39 |
| [Pg 422]Asparagus | 0.21 |
| Lentils | 0.38 |
| Halibut | 1.00 |
| Cod | .05 |
| Salmon | 1.00 |
| Mutton | 0.96 |
| Beef | 1.10-2.00 |
| Veal | 1.10 |
| Ham | 1.10 |
| Pork | 1.20 |
| Oatmeal | 0.53 |
| Beans | 0.63 |
| Chicken | 1.20 |
| Sherry | |
| Claret | |
| Whisky | |
| Brandy | |
| Beer | 0.12 |
| Porter | 0.14 |
| Ale | 0.14 |
| Chocolate | per pint 0.70 |
To keep the body in good condition and to help rid it of accumulated poisons, the following diet lists are recommended:
Daily Dietaries:
| 7 A.M.— | Hot water, 8 oz. |
| 8 A.M. Breakfast— | Stewed prunes, wheatena and cream |
| 2 eggs | |
| 2 slices of buttered toast | |
| 1 cup of milk flavored with cocoa or coffee or 1 cup of cereal coffee with cream | |
| Dinner— | Cream of pea soup |
| Boiled codfish with cream sauce | |
| Mashed potatoes | |
| Cauliflower | |
| Rice pudding | |
| Supper— | Cream toast |
| Baked potatoes | |
| Egg nest | |
| Apple sauce | |
| Hot milk flavored with coffee, cocoa, or 1 cup of cereal coffee | |
| 7 A.M.— | Hot water, 8 oz. |
| [Pg 423]8 A.M. Breakfast— | Grapefruit |
| Cereal and cream | |
| Soft scrambled eggs | |
| Cereal coffee, or milk and coffee | |
| Buttered toast | |
| 12:30 Lunch— | Cream of tomato soup |
| Cottage cheese and cream | |
| Baked potato | |
| Baked apple | |
| Bread and butter | |
| 6 P.M. Dinner— | Chicken, small piece, no gravy or rich dressing |
| Candied sweet potatoes | |
| Baked eggplant | |
| Lettuce salad (lemon juice instead of vinegar) | |
| Bread and butter | |
| Orange or wine jelly | |
| Milk | |
| Breakfast— | Cereal and cream |
| Baked apple with cream | |
| 1 slice of bacon | |
| 1 soft-cooked egg | |
| Toast—butter | |
| Cereal coffee, or milk flavored with coffee | |
| Lunch— | Vegetable soup |
| Scalloped potatoes | |
| Cream cheese | |
| Bread, butter | |
| Stewed pears | |
| [Pg 424]Dinner— | Halibut steak |
| Creamed potatoes | |
| String beans | |
| Fruit salad | |
| Sponge cake, orange sauce | |
| Small coffee |
Probably no one problem affecting the human family is more widely discussed than that of obesity. There are numberless “cures” suggested, most of which contain some good, but they are as a rule more strenuous than the average fat person cares to attempt, or, if attempted, persist in.
Causes of Obesity.—It is stated that at least fifty per cent. of the obesity is of hereditary origin, while the rest may be due to overeating and drinking, unbalanced diets, metabolic changes due to the approach of menopause in women, and diseases such as gout in which there is a certain amount of disturbance in the blood and excretory organs and in which the diet or the disease may be accountable for the gain of surplus adipose tissue. Women approaching menopause may not change their diet in the least and there may still be the noticeable increase of fat.
Obesity Cures.—A great number of the “cures” are undertaken not from a health standpoint but from the esthetic point entirely. It makes no difference what reason is brought forward for instituting the treatment, it is the results which count. Of the cures undertaken which are in themselves good, but which are too strenuous for the average “fat person” to stick to may be mentioned some of the early cures instituted and recommended by Banting, Oertel, and Ebstein. Obesity, then, may be said to be due to (1) heredity, (2) overeating and drinking, (3) lack of exercise (sedentary life), (4) a combination of the above causes. Whether the obesity is due to the lack of exercise or the [Pg 425] lack of exercise is due to the accumulation of fat which causes a disinclination to move on the part of the individual, can only be judged when a thorough examination into the life and habits of the patient is made.
Comparison of Food Intake and Energy Output.—Many fat people who claim to be small eaters in reality constantly consume more food than their age, weight, or mode of living would necessitate. If such patients could be prevailed upon to keep a correct chart of their daily intake of food and the amount of exercise taken, they would be astounded to find how much greater was the intake in comparison to the output of energy, in other words, how much more food they ate than they required to keep them in health. A glance at the first tables in this text will show which foods are utilized by the body chiefly as a source of energy.
Uses of Food in Body.—Physiological chemistry proves that when more food is taken than is needed for the internal and external work of the body, the surplus is stored for future use, first, in the liver and muscles as glycogen for the general expenditures, and, second, as adipose tissue for future use. Thus it is seen that when the intake is constantly greater than the energy expenditure there must necessarily be some way in which the body can store up the surplus fuel, and so long as the digestion remains good and the amount of exercise limited there is no reason why there should not be a constant and steady accumulation of surplus fat which inevitably terminates in obesity.
Water as a Fat Maker.—That water is in itself fattening is of course untrue. A chemical analysis of this fluid shows that it is inorganic in character and cannot alone either produce energy or build tissue. However, this food constituent plays a most important part in all the functions of the body. In the first place the body cannot utilize food unless it is in solution; water is also one of the best known [Pg 426] stimuli to the flow of gastric juice, and for this reason is an important factor in the preparation of the food for its absorption and utilization; since water forms the bulk of the blood, it acts as a distributor or carrier of food to the different parts of the body.
Limiting the Fluids in Obesity.—Thus it is seen that when the intake of fluids is limited, the body will call upon that surplus which is stored in every nerve, tissue, and fluid throughout the entire organism to assist in the necessary work of the organs, thus reducing the body weight just that much.
Exercise.—The athlete who is overweight, due to adipose tissue, increases his exercise at times, even adding to the weight of his clothing, causing an increased energy output, profuse perspiration, etc., all of which causes the body to use its surplus fuel in the form of the stored fat. Exercise does not break down a muscle, it builds it up. Thus many individuals who increase the strenuousness of their exercise complain that their weight is increased even when they observe a noticeable improvement in their general feelings and appearance.
The Appetite.—The great trouble with most women who undertake an obesity cure which calls for an increased amount of energy is that they will develop an increased appetite thereby which they appease with food instead of forcing the body to use the store in hand, thus entirely doing away with any good the treatment might have accomplished. No amount of exercise without a proper regulation of the diet will prove satisfactory as far as the reduction of fat is concerned. The following methods recommended by Banting, Oertel, and Ebstein are included here.
Banting Method.—This method is said to be unsuited to those with weak digestions. Following its use such [Pg 427] individuals have been known to develop renal colic or gallstones; constipation may be present and the entire system may become so deranged as to render the patient liable to disease.[158]
Banting Diet for Obesity.—Breakfast at 9 A.M., consisting of 5-6 ounces of animal food, meat or boiled fish (except pork or veal), 1 small biscuit or 1 ounce dry toast. Total solids, 5-6 ounces. Coffee or tea (without milk or sugar), 9 ounces.
2 P.M.—Dinner: Fish or meat (salmon, eels, herring, pork, and veal excepted), poultry or game; any vegetable except potatoes, parsnips, carrots, turnips, or beet roots; dry toast, 1 ounce; fruit cooked and unsweetened; good claret, sherry, or Madeira, 10 ounces. Total solids, 10-12 ounces.
6 P.M.—Tea: 2-3 ounces cooked fruit; 1-2 ounces rusks; 2-4 ounces solids; 9 ounces tea, without milk or sugar.
7 P.M.—Supper: Meat or fish as at dinner; claret or sherry and water, 7 ounces.
Total daily solids, 21-27 ounces.
Total fluids, 35 ounces.
Oertel pointed out the great benefits which might be derived by those individuals suffering from certain types of heart disease which are accompanied by obesity. He made it distinctly understood that while the treatment in no way affected the heart lesion,—that is, in so far as altering the character of the disease,—it greatly reduced the work imposed upon the circulatory organ and permitted a more complete oxidation of the blood.[159]
Oertel’s Method.—Oertel bases his dietetic treatment of obesity upon the heart changes and those which naturally follow in the circulation. He makes the following suggestions, taking always into consideration the condition of the patient, whether he is anemic or plethoric.
[Pg 428] “(a) Where there is an abnormally increased amount of fat in plethoric patients with unimpaired or only beginning changes in the heart action, the diet should aim at:
(1) An increased supply of protein.
(2) A decrease in the fat-forming substances.
(3) Little or no diminution in the supply of liquids below the physiologic amount (1500 c.c.—3 pt.)
(b) Where there is obesity in anemic patients, viz. serious plethora, the diet should aim at:
(1) An increase in the quantity of proteins.
(2) A diminution in amount of fat-forming substances and eventually
(3) a decrease in the amount of fluid.
(c) Where there is obesity in adults with anemic symptoms in whom not only the amount of protein but also the abnormally increased amount of fat is slowly wasting away, they require:
(1) An increase in the amount of protein taken.
(2) A sufficient amount of fat and carbohydrates or even an increase of same to prevent the falling off of fat.
(3) A diminution in the amount of fluid taken.”
Oertel claims that the simplest method of reducing the fat-forming elements in a diet is to decrease the amount of fat and allow a certain amount of carbohydrates, regulating the diet according to the individual. The following table is given by him as showing the minimum and maximum amount of the different food constituents constituting the obesity diet:
| Protein | Fat | Carbohydrate | Calories | |
| Gm. | Gm. | Gm. | ||
| Minimum | 156 | 25 | 75 | 1180 |
| Maximum | 170 | 45 | 120 | 1608 |
[Pg 429] In instituting a treatment for obesity Oertel insists upon a certain amount of exercise daily in the open air, the amount to be regulated by the physician according to the individual case. He suggests that five or six small meals a day be given rather than a few large meals. He eliminates soups, tea, and coffee while the cure is being given.
Ebstein suggests a diet in which the carbohydrates and fluids are reduced but in which the fats are allowed to a considerable extent. The diet consists of meat, eggs, fish, vegetables (green) and fruits. The following menu demonstrates his dietary régime:
Breakfast: Large cup of tea (no milk or sugar); 2 oz. bread with plenty of butter.
Dinner: Soup 4½ to 5½ oz.; meat with fat sauce; green vegetables; fresh fruit; 2-3 glasses light wine.
Afternoon: Tea as at breakfast.
Supper: Tea, 1 egg, fat roast meat or ham, smoked fish; about 1 oz. bread with plenty of butter; a little cheese and fresh fruit; potatoes, sweets and sugars forbidden.
Dietetic Treatment.—The following menus are suggested by the author: The carbohydrates and fats are restricted and the fluids reduced to a minimum. The meals as far as possible are kept “dry”; soups, milk, cocoa are avoided; water is not permitted at meals; alcoholic beverages, white bread, butter, potatoes, sugar, candy, pastry, cakes, puddings, gravies, sauces, bread dressings, griddle cakes, sirups, molasses, honey, ice cream, cereals, pork of all sorts, ham, bacon pork chops, etc., olive oil, spaghetti, macaroni, and noodles are prohibited.
Allowable Foods.—The following foods are allowed: Black coffee or tea, small cup twice daily without milk, cream, or sugar—saccharin may be used to sweeten if desired; fresh or stewed fruit with the exception of bananas, raisins, and dates, served without sugar; all green vegetables [Pg 430] cooked or served without butter or fat of any description; salads, except potato or banana, served with a special dressing (no oil or sugar); water ices; watermelon and other melons served without sugar; 1 egg a day; gluten toast, no butter; brown bread or muffins made with gluten flour and prepared bran.
The following menus may be used as guides in the treatment of obesity:
| Breakfast— | 1 sliced orange (no sugar) |
| 1 small cup coffee or tea without cream, milk, or sugar (sweeten with saccharin if desired) | |
| 1 poached egg on 1 slice of gluten toast (no butter) | |
| Lunch— | Cottage cheese and lettuce salad with special dressing |
| 2 broiled lamb chops | |
| 1 slice gluten bread; 3 ounces (1 serving) apple sauce (sweetened if necessary with saccharin) | |
| Dinner— | Roast beef |
| Spinach or greens (cooked without fat meat) | |
| Green peas | |
| Tomato and lettuce salad with special dressing | |
| Orange or wine jelly (sweetened with saccharin) | |
| 1 slice of gluten bread or toast | |
| 7 A.M. or 1 hour before breakfast— | 1 cup of water containing juice of ½ lemon |
| Breakfast— | ½ grapefruit without sugar |
| 1 small cup black coffee or tea | |
| Beefsteak broiled and served without butter (lean) | |
| 1 slice of gluten toast | |
| [Pg 431]Lunch— | Tuna fish salad (no olive oil in dressing) |
| 1 bran muffin or 1 slice (1 oz.) gluten toast | |
| 1 baked apple (without cream or sugar) | |
| Dinner— | Roast or boiled chicken (no gravy or bread dressing) |
| Green vegetables (peas, string beans, cabbage,[160] turnips, artichokes (without butter)) | |
| Fruit salad (special dressing) | |
| Lemon ice |
Amount of Food.—The amount of food is limited to a certain extent. Green vegetables may be eaten in abundance, but the protein foods such as meat, fish and eggs must be limited.[161] The bread (even gluten and bran breads) must be limited to 1-2 slices at each meal. All meals are eaten without fluids except breakfast, when one small cup of coffee or tea without milk, cream, or sugar is allowed. If fruit juice is to be served instead of fruit, it must be prepared with little if any water and no sugar. The juice may be poured over cracked ice, if desired.
The following reducing diet is suggested by Dr. Rose for the use of over-fat women:
Fuel value 1052 calories—ordinary requirements 2200 calories
| Key: | |
| A | Weight Oz. |
| B | Protein Calories |
| C | Total Calories |
| Measure | A | B | C | |
| Breakfast: | ||||
| Apple | 1 medium | 4.9 | 2 | 65 |
| Egg | 1 egg | 2.4 | 27 | 75 |
| Toast | 1 slice | 0.5 | 7 | 50 |
| Coffee[163] | 1 cup | |||
| Skim milk | 1½ tbs. | 1.0 | 3 | 10 |
| 10:30 A.M. | ||||
| Bouillon | ½ cup | 4.0 | 10 | 12 |
| Water cracker | 1 cracker | 0.1 | 1 | 10 |
| Luncheon: | ||||
| Lean cold roast beef | Medium serving | 3.5 | 97 | 150 |
| Rye bread | 2 thin slices | 0.7 | 7 | 50 |
| Lettuce and cottage cheese salad: | ||||
| Lettuce | Ad libitum | 40 | 85 | |
| Cheese | 2½ tbs. | |||
| 4:30 P.M. | ||||
| Tea with lemon[163] | 1 cup | |||
| Water cracker | 1 cracker | 0.1 | 1 | 10 |
| Dinner: | ||||
| Boiled cod with lemon | Large serving | 8.2 | 209 | 225 |
| Boiled potato | ½ medium | 1.8 | 6 | 50 |
| Cauliflower (plain) | Large serving | 3.0 | 6 | 25 |
| Butter | 1 tsp. (scant) | 0.1 | 30 | |
| Water-cress and egg salad: | ||||
| Water-cress | Ad libitum | |||
| Egg | 1 egg | 27 | 110 | |
| French dressing | ½ tbs. | |||
| Orange | ½ large | 4.7 | 3 | 50 |
| Black coffee | Demi-tasse | |||
| 10:30 P.M. | ||||
| Hot skim milk | ½ cup | 4.3 | 16 | 45 |
| Total calories | 1052 |
Approximate fuel value 965.5 calories
| Key: | |
| A | Protein Gm. |
| B | Carbohydrate Gm. |
| C | Fat Gm. |
| D | Calories |
| Material | Amount | A | B | C | D |
| Breakfast: | |||||
| Orange | 1 medium | 1.5 | 17.4 | 0.3 | 78.3 |
| Poached egg | 1 egg | 5.3 | 4.6 | 62.6 | |
| on Toast (gluten) | 1 slice (1 oz.) | 8.4 | 8.5 | 0.3 | 70.3 |
| Coffee (black) | 1 cup | ||||
| 211.2 | |||||
| Luncheon: | |||||
| Lettuce and cottage cheese salad: | |||||
| Lettuce | Ad libitum | ||||
| Cheese | 2 tbs. | 5.9 | 1.2 | 0.2 | 30.2 |
| Dressing | 1 tbs. | 1.5 | 3.4 | 36.6 | |
| Lamb chop | 1 chop | 9.2 | 12.7 | 151.3 | |
| Gluten bread or toast | 1 slice | 8.9 | 8.5 | 0.3 | 70.3 |
| Apple sauce | 1 serving, about ⅛ cup | 0.6 | 22.5 | 0.7 | 97.5 |
| 385.9 | |||||
| Dinner: | |||||
| Roast beef | 2 thin slices (2 oz.) | 11.4 | 4.8 | 88.8 | |
| Spinach | ½ cup | 2.3 | 3.6 | 0.3 | 26.3 |
| Green peas | ½ cup | 4.8 | 11.1 | 0.2 | 65.4 |
| Lettuce | Ad libitum | ||||
| Tomato | 1 medium | 0.4 | 3.1 | 0.2 | 15.8 |
| Dressing | 1 tbs. | 1.5 | 3.4 | 36.6 | |
| Orange jelly: | |||||
| Orange juice | ½ cup (8 tbs.) | 14.2 | 56.8 | ||
| Lemon juice | 1 tbs. | ||||
| Gelatin | 1 tsp. | 2.1 | 8.4 | ||
| Water | 1 tbs. | ||||
| Saccharin | 1 tablet or less | ||||
| (gluten) | 1 slice | 8.4 | 8.5 | 0.3 | 70.3 |
| Total grams | 72.2 | 98.6 | 31.7 | 368.4 | |
| Total calories | 965.5 |
Approximate fuel value 930.5 calories
| Key: | |
| A | Protein Gm. |
| B | Carbohydrate Gm. |
| C | Fat Gm. |
| D | Calories |
| Material | Amount | A | B | C | D |
| Breakfast: | |||||
| Fruit | 1 orange | 0.850 | 12.050 | 0.150 | 53.0 |
| Gluten toast | 2 slices | 17.800 | 17.000 | 0.600 | 140.0 |
| Egg (poached or soft-cooked) | 1 egg | 5.300 | 4.600 | 60.0 | |
| Coffee (black) | 1 cup | ||||
| 253.0 | |||||
| Luncheon: | |||||
| Oyster cocktail | 6 oysters | 3.500 | 4.200 | 0.680 | 37.0 |
| Cold roast beef | 1 slice (1 oz.) | 5.700 | 2.400 | 44.0 | |
| Cold slaw: | ½ cup | ||||
| Cabbage | ½ cup | 0.002 | 0.001 | 0.034 | 4.5 |
| Dressing | 1 tbs. | 1.500 | 3.400 | 36.0 | |
| Gluten toast | 2 slices | 17.800 | 17.000 | 0.600 | 140.0 |
| 261.5 | |||||
| Dinner: | |||||
| Chicken (without stuffing) | 3 oz. one serving | 18.200 | 2.100 | 92.0 | |
| Broiled mushrooms | 6 medium size | 1.500 | 3.000 | 0.180 | 19.0 |
| String beans | 3 oz. one serving | 1.950 | 6.290 | 2.290 | 34.4 |
| Pineapple salad: | |||||
| Lettuce | Ad libitum | ||||
| Pineapple | 1 slice | 4.000 | 31.000 | 0.600 | 129.5 |
| Dressing | 1 tbs. | 1.500 | 2.400 | 37.0 | |
| Apple float: | |||||
| 1 apple | 1 apple | 0.600 | 22.200 | 0.770 | 98.1 |
| ½ egg white | ½ egg white | 1.500 | 0.020 | 6.0 | |
| Saccharin to sweeten | |||||
| Total grams | 416.0 | ||||
| Total calories | 930.5 |
Rules and Regulations.—The following directions and menus are given to be used when a reduction in weight is [Pg 435] necessary. Care must be taken not to allow large amounts of even the non-fat-forming foods in the dietary, since under certain conditions the body will manufacture adipose tissue of any surplus organic material ingested. Breakfast must be limited as demonstrated in the tabulated diet sheet.
Keeping the Weight Down.—After the individual has been reduced to approximately the desired weight the diet may be made a trifle more liberal, keeping in mind, however, that moderation is the keynote in the obesity régime and will have to be practised to a certain extent always. It is wise to continue the dry meals and to limit the amount of butter, cream, and other “fatty foods,” to a certain extent. Pork, with the exception of crisp bacon several times a week at breakfast, had best be avoided, and alcoholic beverages should be omitted entirely except when prescribed by the physician. The outdoor exercise should be continued and only the amount of sleep requisite to health indulged in. If the individual will faithfully carry out these directions, there is no reason why the weight should continue to be a burden. It must be remembered that it is never safe to diet indiscriminately and without the advice of a physician, since much harm may come of so doing.
Value of Massage.—Massage is an advisable accompaniment to an obesity diet and will help to prevent a sagging of the tissues which have been deprived of the supporting fat. The tissues of the face, neck, and breast are especially apt to wrinkle unless given the exercise and stimulation from massage. Cold baths are likewise advisable, since they stimulate the body to burn up the fat.
| Lunch— | Tuna fish salad |
| Cauliflower | |
| Baked apple | |
| [Pg 436]Dinner— | Soft-shell crabs |
| Roast lamb | |
| Spinach | |
| Tomato jelly | |
| Grapefruit | |
| Lunch— | Corned beef and cabbage |
| Stewed pears | |
| Dinner— | Clam cocktail |
| Roast chicken | |
| Asparagus | |
| Fruit salad | |
| Lunch— | Broiled oysters; cold lamb |
| Boiled turnips | |
| Water-cress salad | |
| Dinner— | Roast beef |
| Stewed tomatoes | |
| String beans | |
| Lettuce and tomato salad | |
| Sliced peaches | |
| Lunch— | Broiled calves’ liver |
| Greens (mustard, turnip, beet tops, or dandelion) | |
| Orange jelly | |
| Dinner— | Crab-flake cocktail |
| Broiled squab | |
| Artichokes | |
| Stewed celery | |
| Lettuce, Russian dressing | |
| Lunch— | Kippered herring |
| Veal croquettes (baked instead of fried, with tomato sauce; this dressing is made by adding [Pg 437] 1 teaspoonful of chili sauce to the regular dressing used in obesity diets) | |
| Asparagus | |
| Apple sauce | |
| Dinner— | Baked halibut steak, stuffed with oysters |
| Boiled onions | |
| Boiled carrots | |
| Pineapple and grapefruit salad | |
| Lunch— | Broiled calves’ brains |
| Vegetable salad | |
| Melon | |
| Dinner— | Broiled chicken |
| Boiled beets | |
| String beans | |
| Cucumber and young onion salad | |
| Raspberry ice | |
| Lunch— | Stuffed eggs |
| Sliced tongue with spinach or greens | |
| Carrots or beets | |
| Fruit | |
| Dinner— | Roast turkey, cranberry sauce |
| Cauliflower | |
| Tomatoes stuffed with celery, green peppers and onion dressing | |
| Peach whip | |
| Lunch— | Hashed beef |
| Boiled onions | |
| Stewed prunes | |
| Dinner— | Oysters |
| Baked rabbit | |
| Eggplant (baked) | |
| Spinach | |
| Fruit jelly |
Emaciation as a rule is a symptom of an abnormal condition rather than a disease in itself. Certain individuals are said to be “constitutionally thin” and upon investigation it is often found that this thinness extends back in many cases for generations, many members of a family being thin no matter what measures are taken to overcome the condition. However, constitutional emaciation is not so prevalent as constitutional obesity and, as has already been stated, is more often a symptom of some metabolic disturbance or pathological condition.
Causes of Emaciation.—Errors in diet—insufficient or improper food—are accountable for most of the cases seen in infants and children. Over-exercise, that is, when the amount of exercise taken is not commensurate with the intake of food, is accountable for other cases. This type of emaciation is found especially in growing children.
Disease as a Cause.—Wasting diseases, such as tuberculosis and anemia, bring about a loss of weight, while in fevers in general and typhoid fever especially not only the febrile condition hastens the metabolic processes but also the activities of the bacteria act together and break down the tissues of the body, causing a falling off from the normal body weight. Loss of sleep, unhygienic or unsanitary surroundings, and capricious appetites probably cause some of the cases of excessive thinness.
Thinness in Children.—Parents are to blame for much of the thinness seen in children, especially the nervous high-strung children whose energies outweigh their desire for food or, as is more often the case, their willingness to eat the proper foods. It is a mistaken kindness to cater to the whims and fancies of a child’s appetite, and much harm is wrought by allowing the “trash” to overbalance the necessary building or repair food in the dietary. Not that sugar is not necessary, for it is particularly so at the age when [Pg 439] the metabolic processes are faster than later in life, but it must be remembered that the body is being built up both in height and breadth.
The Need for Building Foods.—The skeleton and the muscular tissues cannot be constructed from sugar, hence the diet which consists chiefly of this food constituent is unbalanced and will sooner or later bring about disturbances which are very apt to result in emaciation. The causes of emaciation may be summarized as follows:
(1) Those cases which are due to pathological conditions such as tuberculosis, anemia, typhoid fever, etc.;
(2) Those induced by errors in diet and bad habits such as insufficient or improper food, loss of sleep, over-exercise, lack of ventilation in the sleeping apartment, which destroys the appetite;
(3) Malformation or deformities of mouth, throat, or stomach which make it impossible for the individual to partake of sufficient food to cover the needs of the body;
(4) Heredity (“constitutional thinness”).
Regulating the Diet.—As has been stated in a former chapter, any persistent loss of weight or failure to gain on the part of an infant whose chief business in life should be to grow, should be given immediate and careful attention. As a rule the diet is to blame; it is either improperly balanced, insufficient in amount, or poorly prepared, any of which might readily cause a disturbance to the delicate apparatus of the child.
Diet and Habits.—In adults, the diet and habits of life are in many cases to blame for the excessive thinness seen in many individuals. If the trouble can be traced to some abnormal condition, it can only be removed by relieving or checking the disease which induced it. The older methods of treating typhoid fever, for example, did nothing to prevent the progressive emaciation which was the result not only of the accelerated metabolism from the fever but [Pg 440] also from the invasion of the intestinal tract by the specific bacteria which brought about a like result. In tuberculosis a similar breaking down of the tissues occurs, as is likewise the case in anemia and other diseases in which the functions of the blood-making organs are interfered with. Any of the above diseases may cause emaciation, and the treatment in most of the cases resolves itself in removing the cause as far as possible and in adjusting the diet.
Selection of Food.—The dietetic treatment for emaciation is practically the only one which will materially change the weight of the individual, since by food alone is the body built. Certain foods are more capable of being readily converted into adipose tissue than others, and these must have a prominent place in the dietary.
Rules and Regulations.—In obesity it was found that it was necessary to curtail the sleep and rest, increase the amount of exercise and decrease the amount of food. In emaciation practically an opposite régime is adopted. The patient is urged to eat plenteously, drink copiously of water and nutrient beverages, soup, etc., avoid worry and excitement, over-exertion and indigestion, to take one or two naps every day, to retire early, to avoid hot baths and take a warm cleansing bath followed by a cold shower or sponge bath. Exercise must be of a mild character; the patient must be warned against becoming exhausted, since this condition precludes a gain in weight.
Dietetic Treatment.—The meals must be carefully selected, well prepared and daintily served, that all of the psychical benefits from such efforts may be attained. A nutrient beverage such as cream, egg, and vichy, reënforced fruit beverages, malted milk, with egg and chocolate, cereal and milk gruels, etc., may be given between breakfast and lunch, lunch and dinner and before retiring. The meals must consist of the simplest foods that the digestion may not be overtaxed by the quantity ingested.
[Pg 441] Allowable Foods.—The following foods may be used in the treatment of emaciation: All dairy products, milk, cream, butter and cheese, eggs cooked in various ways, soups of all kinds, meats in moderation, vegetables, especially potatoes, olive oil, and the various salad oils, cereals, tapioca, macaroni, spaghetti, noodles, rice, bread of every description, fruit including bananas, grapes, dates, raisins, prunes, etc., ice creams, farinaceous puddings, sauces, except those containing vinegar, grape juice and other fruit juices sweetened with sugar, cocoa and chocolate, malted milk and proprietary infant foods, honey, molasses and sirups, cakes, cookies and pastry in moderation. It is advisable to make milk the chief fluid food; to this is added cream, malted milk, lactose, eggs, and other reënforcing agents.
Milk Cure.—Certain physicians advise milk alone, giving from one to two gallons a day for three weeks or longer. Many individuals complain that “milk makes them bilious” but, as a rule, this is because the amount taken is small and the solids insufficient to lend the necessary bulk to the feces, consequently the peristaltic action becomes sluggish and the passage of the food mass delayed in the intestinal tract, furnishing a medium for bacterial growth and activity. When larger quantities are ingested such is not the case and the fluid so high in nutrient qualities is utilized by the body for the building up of the depleted tissues. When the emaciation is the result of disease the diet is necessarily adjusted to meet the condition. At times it is most difficult to overcome the anemia and accompanying emaciation on account of the disease precluding the giving of the foods especially designed by nature to produce flesh. This is especially the case in the progressive emaciation in diabetes. However, in this case the Allen starvation treatment, with the reëducation of the organs to a toleration for [Pg 442] carbohydrates, has gone far toward overcoming this distressing condition.
Readjusting the Habits.—When the loss of weight is found to be the result of close application to work, lack of fresh air and sleep, or from errors in diet, a change of climate and occupation should be made, together with a readjustment of the daily habits, such as substituting a cool bath for the regular hot one, and sleeping out of doors or on a sleeping porch instead of in a poorly ventilated bedroom.
The patient must be urged to eat, regardless of appetite, for in this way only can the body weight be increased. The dietary must be made up largely of the fat-forming foods, but not to such an extent as to upset the nitrogen equilibrium.
The following diet sheet is given to be used as a guide in the treatment of emaciation. Other foods of a similar composition and fuel value may be substituted for those given here, to vary the diet.
Approximately 5106 calories
| Key: | |
| A | Protein Gm. |
| B | Carbohydrate Gm. |
| C | Fat Gm. |
| D | Total Calories |
| Material | Amount | A | B | C | D | ||||
| Breakfast: | |||||||||
| Stewed prunes | 6 prunes | 1.02 | 35.26 | 145.0 | |||||
| Sugar | 1 tbs. | 14.70 | 56.6 | ||||||
| Oatmeal | 1 tbs. (dry) | 3.20 | 25.00 | 6.60 | 172.2 | ||||
| with cream and | 2 tbs. cream | ||||||||
| sugar | 1 tbs. sugar | ||||||||
| Poached egg | 1 egg | 5.35 | 4.16 | 58.8 | |||||
| Toast | 3 slices | 7.90 | 44.70 | 13.00 | 328.0 | ||||
| Butter | 1 tbs. | ||||||||
| Coffee | 1 cup | ||||||||
| with cream and | 1 tbs. cream | .40 | .40 | 2.80 | 53.9 | ||||
| sugar | 2 tsp. | 9.45 | |||||||
| Milk and cream | ⅔ cup milk | 389.0 | |||||||
| ⅓ cup cream | |||||||||
| [Pg 443] | |||||||||
| 11 A.M. | |||||||||
| Cereal milk gruel | 8 oz. (1 cup) | 248.0 | |||||||
| with cream | 1 ounce | ||||||||
| Lunch, 1 P.M. | |||||||||
| Cream of pea soup | 8 oz. (1 cup) | 6.00 | 17.65 | 7.66 | 185.9 | ||||
| Potato salad | 3.5 oz. (1 serving) | 1.75 | 15.50 | 15.33 | 210.0 | ||||
| Bread | 3 slices | 7.80 | 44.70 | 1.04 | 328.0 | ||||
| Butter | 1 tbs. | .80 | 1.40 | 5.60 | |||||
| Cocoa made with milk | 1 cup | 27.00 | 27.60 | 41.40 | 661.0 | ||||
| Sugar | 2 tsp. | ||||||||
| Milk | ⅔ cup | ||||||||
| Cream | ⅓ cup | 329.0 | |||||||
| 3:30 P.M. | |||||||||
| Cream, egg, vichy | 8 oz. | 4.90 | 12.40 | 36.00 | 393.0 | ||||
| Dinner: | |||||||||
| Tomato bouillon | 1 cup | 38.0 | |||||||
| with whipped cream | 1 tbs. | .30 | .42 | 5.67 | 53.9 | ||||
| Beefsteak | 1 serving (3 oz.) | 18.60 | 17.34 | 230.5 | |||||
| Mashed potatoes | ⅓ cup | 1.16 | 7.50 | 3.50 | 66.5 | ||||
| Cauliflower | 1 serving | 1.53 | 2.99 | .42 | 21.8 | ||||
| Asparagus salad | 6 stalks | 2.00 | 3.72 | .24 | 111.8 | ||||
| with mayonnaise | 2 tsp. | .01 | 1.45 | 9.00 | |||||
| Bread | 2 slices | 5.20 | 29.80 | .68 | 419.0 | ||||
| Butter | 2 tbs. | .28 | 24.09 | ||||||
| Charlotte russe | 1 serving | 2.30 | 11.10 | 22.60 | 257.0 | ||||
| Milk | ⅔ cup | 389.0 | |||||||
| and cream | ⅓ cup | ||||||||
| Black coffee if desired | ½ cup | ||||||||
| At bed time: | |||||||||
| Malted milk made with milk | 1 cup | 8.40 | 41.00 | 10.20 | 288.5 | ||||
| and reënforced with lactose | 1 ounce | ||||||||
[Pg 444] Methods of Increasing the Diet.—The above diet furnishes three times as much food as is needed to maintain the body living a sedentary life, or about as much as would be needed to maintain a lumberman at hard outdoor labor in the Maine woods. It would be impossible for an ordinary individual to handle such an abundant diet without making the increase in the diet gradually. This is best done by adding the milk and cream at the end of each meal and a glass of milk between meals and at bedtime, then gradually adding the fattening foods already mentioned until the diet approximates the diet sheet here computed.
Gout is a constitutional disease characterized by an inflammatory condition of the joints.
The Joints are the seat of chalky deposits of uric acid or sodium salts.
Metabolism in gout is disturbed, with a consequent retention instead of elimination of uric acid by the body.
The Blood contains an excess of uric acid which increases greatly during an acute attack.
The Urine in true gout does not contain an excess of uric acid except during an acute attack, whereas in the so-called goutiness there is a constant excess of this acid.
Uric Acid is produced as the result of the metabolism in the human body of the nucleoproteins and in food of the purin bodies.
Alcohol undoubtedly assists in the retention and increases the difficulty of uric acid elimination by the body.
Chief Causes of Gout.—Overeating, excessive alcoholism, and too little exercise, especially in the open air.
Treatment consists in regulating the diet both as to the quantity and type of food eaten; reducing or eliminating [Pg 445] the alcohol in the dietary, and increasing the amount of outdoor exercise.
Dietetic Treatment.—The best results are obtained by reducing the size of the meals and avoiding the purin-bearing foods as far as possible. Eggs are purin-free and may be substituted for much of the meat in the diet. In chronic gout it is impossible to eliminate meat entirely from the diet, but the quantity can be materially reduced and that which is eaten may be rendered less harmful if it is boiled instead of roasted or broiled, as in this way much of the purin is dissolved out. Highly spiced and seasoned foods, rich gravies, etc., are apt to cause an acute attack and should be omitted. Excesses of all kinds must be avoided to enable the patient to live a fairly comfortable life, free from frequent painful attacks of gout.
Causes.—Heredity, overeating, unbalanced diet, chronic alcoholism, and disturbed metabolism, as manifested in gout and other pathological conditions.
Cures are more or less of a risk, except when undertaken upon the advice and under the care of a competent physician. As a rule they are too strenuous to be carried out alone and are of no good unless persisted in. Among the best known obesity cures may be mentioned those formulated by Banting, Oertel and Ebstein.
Most physicians have their own methods of treating obesity, but all are based primarily on diet and exercise.
Food is the chief cause of obesity and since some foods are more readily converted into adipose tissue than others, it is necessary to understand the behavior and functions of the various food combinations in the body before it is possible to say which are the offending articles of diet.
Water has no fattening properties of its own. This is proved by a glance at its chemical composition, but as it [Pg 446] acts as a distributor and carrier of food to the various parts of the body and since the bulk of all the secretions is composed of water and every tissue in the body stores this fluid, thus adding to the weight, a consideration of the intake of water for obesity patients is most essential.
Appetite requires attention. The majority of obese patients eat more than their energy output calls for, consequently it is necessary to curb the appetite and increase the energy output in order to utilize the material on hand in the form of adipose tissue.
Exercise is absolutely essential in order to force the body to burn up its surplus fat as fuel. The best form of exercise is that which is taken out of doors. The well-worked muscle is heavier than one which is unaccustomed to exercise. The latter is infiltrated with fat and weighs less than muscular tissue, but a muscular body can endure more than one which is covered with adipose tissue.
The Heart of obese patients becomes more or less affected as obesity advances and it becomes absolutely necessary in many cases to get rid of some of the surplus fat in order that the patient may live. This is best accomplished by dietetic treatment.
Circulatory Changes likewise occur as the heart becomes affected, making it necessary to institute some dietary measures at once.
Glycosuria in obese patients suffering from gout is not at all unusual and to relieve this condition the carbohydrates in the diet must be at once reduced.
Dietetic Treatment is most important. It constitutes the only rational method of ridding the body of its surplus fat. To do this it is necessary to regulate the diet both as to quantity and type. Fat-forming foods are those which the body utilizes most easily for the production and storage of fat. Any food, no matter whether it is fat-forming or [Pg 447] not, if taken greatly in excess of the needs of the body, will be stored as adipose tissue.
Chief Points to be remembered in formulating a diet and instituting an obesity treatment are the necessity for small meals and dry meals, no fluid given at all during the meal except perhaps one or two small cups of coffee per day, without sugar or cream, the avoidance of fat-forming foods, sugars and starches in all forms, milk, cream, butter and oil, potatoes, bananas, fat meats of all descriptions, especially pork, soups of every description and alcoholic or malted beverages. It is necessary to limit the amount of sleep, prohibiting naps during the day, and to increase the amount of outdoor exercise.
Massage is advisable, especially in those patients who are unable, on account of their excessive weight or heart symptoms, to take the requisite amount of exercise necessary for their future welfare. Massage likewise makes the muscles firmer, often preventing the disfiguring sagging of the skin caused by depriving it of its padding of fat.
Causes.—Errors in diet, overwork, over-exercise, heredity, nervousness, worry, malformation of the mouth, throat, or stomach, heredity and certain pathological conditions, such as typhoid fever, tuberculosis, anemia, dysentery, etc., in which the breaking down of the tissues occurs more rapidly than they can be rebuilt.
Children are often emaciated on account of their unbalanced diet. They receive an insufficient amount of building food to cover their growth and development requirements. Parents are often to blame for allowing the child to overeat of some of the food constituents at the expense of others. Sugar, for example, is very necessary in the diet of a growing active child, but all sugar and very little milk and eggs [Pg 448] will lead to an unbalanced diet which may bring about a condition of extreme thinness later on.
In Adults the constant eating of the wrong foods, overworking and persistent worrying, all contribute to the breaking down of the tissues which ends in emaciation.
Weight is an index to health. Any persistent loss of weight on the part of an adult or loss or even failure to gain in a growing child, are indications that all is not right and immediate measures must be taken to locate and relieve the trouble.
Loss of Weight due to pathological conditions can only be relieved by removing the cause, after which the diet may be adjusted to suit the condition.
Dietetic Treatment is practically the only means of combating and overcoming emaciation, since it is by food alone that the body is built.
Fat-forming foods, which in obesity were prohibited, have a prominent place in the diet for emaciation. Padding the nerves and organs with a layer or covering of fat protects them from the jars and shocks incidental to daily life, besides lending grace and contour to the body.
Foods Which Produce Fat are nutrient beverages of all sorts; milk, malted milk and cream are especially valuable; water, because of its particular properties and functions in the body; and fruit beverages, which are made chiefly of water and sugar, are always included in the dietary. Milk and cream, soups and milk gruels, as well as all dishes made with milk or cream, add materially to the fat-forming quality of the diet. Butter, olive and other salad oils, as well as cereals, potatoes, bread and simple desserts are advised. The diet must be bountiful, the meals frequent, and lunches consisting of milk or cream with crackers will hasten the gain in weight.
Rest, preferably lying down, is absolutely essential. A period of relaxation covering from fifteen to thirty minutes [Pg 449] should be taken before or after each meal. The body derives the use of the food for the storage of fat which would otherwise be required to cover its energy expenditures.
Sleep is essential to gain, consequently the patient should retire early and take one or two naps during the day.
Baths should be warm, not hot, followed by a cold shower or sponge.
Exercise must be mild in character; over-exertion precludes a gain in weight and exhaustion undermines the forces which make it possible for the body to store fat as adipose tissue.
Nervous Excitement and Worry must be avoided.
Gastro-intestinal Disturbances should be guarded against, since all the pounds gained through months of treatment may be quickly lost during one acute attack of diarrhea or auto-intoxication.
Massage is advised. The kneading and gentle manipulation of the muscles stimulates them to utilize more food material, besides enabling the patient to eat more by reason of an increased appetite.
The Milk Cure has been used extensively in overcoming extreme emaciation. It consists in the taking of large quantities, ranging from one to two gallons per day. It is given every hour or oftener for a period of one month to six weeks.
Reënforcing the Diet with eggs and lactose is often found of great value in increasing the weight quickly, as is the giving of one-third of a glass of cream and two-thirds of a glass of milk after each meal and at bedtime. The whole scheme of putting on pounds resolves itself into the giving of proper food in larger quantities than are ordinarily given, but dividing it up into frequent meals in order not to upset the digestion and do away with the good already accomplished.
(a) Formulate a diet order for a patient with gout in which the purin foods are eliminated.
(b) Formulate a diet order for an obese patient whose heart is more or less affected.
(c) List the foods of special value in the diet for emaciation. Write a diet order for day suitable for a patient (woman) weighing 110 pounds, whose normal weight is 135 pounds.
[156] “Food for the Sick,” p. 97, by Strouse and Perry.
[157] The amount of food must be limited, since overeating will precipitate an acute attack. It is best to limit the amount to about a maintenance allowance or a little more, temporarily.
[158] “Diet in Health and Disease,” by Freidenwald and Ruhräh.
[159] Ibid., p. 544.
[160] Boiled vegetable dinners must be prepared without fat meat and potatoes.
[161] Scientific investigation has proved that both carbohydrates and fats may be formed in the body from protein. Hence any excess above that required to keep the body in nitrogen equilibrium is utilized by the organism for fuel or stored as fat.
[162] “Feeding the Family,” p. 84, by Mary Swartz Rose.
[163] Saccharin may be used to sweeten.
The poisoning due to ptomaine is very similar to that brought about by overeating and other dietetic errors. However, it is not so easy to avoid being poisoned by ptomaines as it is to observe moderation in the quantity of food eaten.
Origin.—These substances are believed to be of an infective bacterial origin and may be present in foods which are otherwise seemingly fresh and good. The fact that they cannot be detected in food without an analysis makes them more of a menace than they would otherwise be, for any substance which is not discernible to our senses, the taste, sight, or smell, and which exerts a baleful influence, such as ptomaine, cannot be anything but a menace to humanity.
Infected Food Materials.—We may congratulate ourselves in the knowledge that these substances are not present in many foods, and if we avoid eating nitrogenous materials, which may have become polluted, either through imperfect canning or by standing in unclean vessels, we may avoid much of the poisoning which may otherwise be due to the action of ptomaines.
Chicken Salad and Ice Cream Poisoning.—Certain violent attacks of so-called ptomaine poisoning may be traced to chicken salad which has been allowed to stand overnight in tin receptacles or to ice cream which has melted [Pg 452] and been re-frozen. In any case the treatment remains the same.
Treatment.—The patient is put to bed and the intestinal tract cleansed by means of enemas and in many cases purgatives (salts, castor oil, etc.) as directed by physician.
The symptoms usually present in those suffering from ptomaine poisoning are nausea, vomiting, dizziness, pain more or less violent in character, and prostration which is at times alarming.
Dietetic Treatment.—The treatment instituted under the circumstances is very much the same as that used in other forms of acute poisoning. All food is withheld for a period; the duration of this starvation must necessarily depend upon the condition of the patient, the violence of the poison and the extent of the prostration.
Rectal Feeding.—When the prostration is great, it is sometimes necessary to give saline enemas and even rectal alimentation to prevent collapse.
Fluid Diet.—After the violent attack subsides, the patient is placed upon a fluid diet similar to that used in auto-intoxication and practically the same as the diet for acute infectious diseases. The diet must be gradually increased until it becomes normal and the nurse must remember that the patient is in a condition to suffer a relapse with the least indiscretion. It is advisable to have a thorough investigation made to ascertain the source of the original attack, that the patient may be able to avoid future trouble from partaking of the same food.
Personal Idiosyncrasies.—It may be that there is a personal idiosyncrasy against one particular food, and in this case it becomes more or less of a simple matter to prevent future attacks. Certain individuals are, for example, invariably poisoned by eating shellfish, others manifest a similar idiosyncrasy against strawberries. Thus is the old proverb demonstrated: “What is one man’s meat is [Pg 453] another man’s poison.” And he who wantonly flies in the face of the danger signals Nature provides for his guidance must necessarily suffer the consequences of his folly.
It has been proved with certain individuals that the foods that at one time cause an attack of poison at another time may be eaten with impunity. Thus it would seem to remain a question not so much of the type of poison, ptomaines, etc., as the amount of resistance manifested at the time by the individual partaking of the infected food.
Metabolism of Fats.—Acidosis is a condition believed to be due primarily to some impairment in the metabolism of fat in the body, in consequence of which there is an accumulation of substances more or less irritating and at times toxic in character in the blood. These substances, known as acetone bodies, are especially apt to appear in the urine of individuals suffering from diabetes, likewise in those undergoing starvation, whether as a result of treatment to overcome a definite pathological condition, as in diabetes, or as the result of disease itself.
Malnutrition as a Source.—Certain individuals, children especially, develop symptoms of acidosis under many different circumstances; for example, in many cases of malnutrition the evidences of acidosis are almost invariable. The treatment in these cases must be, of course, prompt in order that the condition may not assume a serious aspect.
Dietetic Treatment.—The diet is adjusted in order to neutralize the effect of the acid in the blood. This is done in two ways: first, by reducing the fat, and second, by increasing the amount of base-forming foods in the diet.
The following table[164] illustrates the foods in which the acid-forming elements and base-forming elements predominate:
Foods in Which Acid-Forming Elements Predominate
Estimated Excess Acid-forming Elements Equivalent to C.C. Normal Acid per 100 Calories
| Beef, free from visible fat | 10.0 |
| Eggs | .9 |
| Round steak | 6.7 |
| Oatmeal | 3.2 |
| Wheat flour | 2.7 |
| Wheat, entire grain | 2.6 |
| Rice | 2.4 |
| Bacon | 1.0 |
| Corn, entire grain (high protein) | .1 |
Foods in Which Base-Forming Elements Predominate
Estimated Excess Base-forming Elements Equivalent to C.C. Normal Alkali per 100 Calories
| Celery | 40.0 |
| Cabbage | 10-13.6 |
| Potatoes | 9-12.0 |
| Prunes | 7.9 |
| Turnips | 6.6-12.5 |
| Apples | 5.0 |
| Milk | 3.3 |
| Beans | 2.9-6.8 |
| Peas | 1.9 |
| Corn, entire grain (low protein) | .8 |
The fruits likewise show a predominance of base-forming elements over acid-forming elements and for this reason may be used to balance the diet.
Diabetic Acidosis.—The acidosis during diabetes has been already discussed in the chapter devoted to that disease.
It has been found advisable in the majority of cases of acidosis to restrict the fat in the diet of all patients who, during the course of a disease, have given evidence of this condition; at the same time it is well to remember that fat is one of the essential food constituents and absolutely necessary to the welfare of the individual, consequently it is impossible to eliminate it from the diet entirely. The only feasible method, then, to pursue under the circumstances [Pg 455] is to restrict the fats in the diet so long as there are symptoms of acidosis and to add them gradually and in very small amounts until the individual’s tolerance for fats is determined.
Balancing the Diet.—In many cases of acidosis due to starvation, no matter what the cause, the diet must be necessarily regulated and properly balanced. It would be decidedly unwise to attempt to build up the body by giving building foods alone, without due consideration to the foods containing the agents provided by Nature to neutralize the acid formed during the process of their metabolism. It is readily seen in the table just given that meat and eggs show a marked excess of acid-forming elements, whereas vegetables and fruits yield an excess of base-forming elements. With these data, it becomes more simple to balance the diet and to avoid the acidosis which may arise from impairment of the fat metabolism of the body.
The enormous increase in the number of cases of pellagra in America during the last twenty years makes it necessary for something to be done to arrest its progress. The cause of this disease is still under discussion, but much has been done to find out definitely the reason for the tremendous increase in the number of cases, especially in the Southern States, where the increase has been most noticeable.
Cause.—This disease has been the subject of much study and discussion in this country in recent years. Voegtlin, in an article published in a Report of the United States Public Health Service (Reprint 597 of Public Health Report), summarizes the current findings on pellagra as follows:
“1. The hypothesis that there is a causal relation between pellagra and a restricted vegetable diet has been [Pg 456] substantiated by direct proof to this effect and has led to results of considerable practical and scientific value.
“2. The metabolism in pellagra shows certain definite changes from the normal, which point to decreased gastric secretion and increased intestinal putrefaction.
“3. In the treatment and prevention of pellagra, diet is the essential factor. The disease can be prevented by an appropriate change in the diet without changing other sanitary conditions.
“4. A diet of the composition used by the pellagrins prior to their attack by the disease leads to malnutrition and certain pathological changes in animals, resembling those found in pellagra. A typical pellagrous dermatitis has not been observed in animals. Pellagrous symptoms have been produced in man by the continued consumption of a restricted vegetable diet.
“5. The nature of the dietary effect has not been discovered, although certain observations point to a combined deficiency in some of the recognized dietary factors as the cause of the pellagrous syndrome.”
Dietetic Treatment.—The diet in pellagra is one which is well balanced in all its particulars, and one in which the proteins are carefully adjusted as to type. The best results have been observed on diets in which the complete proteins (milk, meat and eggs) have a prominent place. As a rule, in the diet of an adult suffering from pellagra, at least forty grams (about 60 per cent) of the necessary proteins should be in this form. The diet for pellagra must necessarily be such as to overcome as far as possible the progressive emaciation which is an important symptom. However, it must be kept in mind that gastro-intestinal disturbances are likewise prominent and that diarrhea is often most difficult to overcome. For these reasons it is essential to formulate a diet which will not interfere with the treatment for the disease, and which will be at the same time one on which the patient [Pg 457] can gradually be built up, and in this way benefit, as far as possible, under the circumstances. The diet used in the treatment of anemia seems to be the one best suited to meet the requirements of the patient suffering with pellagra; changes may be made in this diet, however, by the physician, who will be able to judge the need of the individual under his care. Whether pellagra can be cured by dietetic treatment is very uncertain, but the condition of the patient can undoubtedly be materially improved, provided the treatment is begun sufficiently early; that is, before the disease has progressed to such an extent that neither diet nor anything else can bring about a cure.
The above dietetic treatment is not claimed to be infallible. It is merely given as a suggestion to be used at the discretion of the physician.
In all probability the treatment of pellagra will undergo a definite change in the near future, but at present our best results accrue from the giving of an adequate, well-balanced diet. The extent of the relief of such dietetic measures depends, as has already been stated, upon taking the disease in its early stage.
Food Poisoning is more or less common, being induced by polluted water, milk, or other foods, bad sanitation, and imperfect canning, as well as by certain obscure substances known as ptomaines.
Shellfish have often been found to cause poisoning in certain individuals. Stale fish may cause the most violent type of poisoning in any individual.
Chicken Salad which has been kept overnight in tin receptacles has been known to cause violent attacks of poisoning.
Ice Cream which is melted and re-frozen is likewise a source of a number of the cases reported.
[Pg 458] Symptoms.—Very like those of auto-intoxication, and violent intestinal disturbances are manifested.
Prostration may be great, according to the violence and duration of the attack.
Anemia follows many cases of poisoning as a result not only of the impairment and lack of nutrition of the blood-making organs, but also on account of the other symptoms, especially diarrhea occurring in the disease.
This condition is more or less common, especially in the disturbances manifested by children.
Cause of acidosis is believed to be an impairment of metabolism, especially in regard to the fats.
Starvation or Malnutrition is believed to produce many cases of acidosis in childhood and adults suffering from diseases in which certain foods have been limited.
Dietetic Treatment like that used in acute gastro-intestinal disturbances begins with a starvation period and is followed by a simple fluid diet until violent symptoms subside. Examination of the stools and the material vomited will, at times, furnish an insight as to the source of the poison.
Convalescent Diet is begun after the violent symptoms have subsided, but care must be taken not to increase the diet too rapidly, owing to the danger from relapse.
Method of Administering Diet.—First: a period of total abstinence from food.
Second: fluid diet consisting of broth, buttermilk, or some of the predigested liquid beef preparations which furnish both food and stimulation necessary in such cases.
Rectal Feeding may be found necessary when the prostration is great.
Personal Idiosyncrasies should be taken into account and effort made to find whether or not the attack is caused by any one food material or by bad sanitation or unclean [Pg 459] food. The patient should be warned against the danger of taking a food which has caused a previous attack of poisoning, especially in cases where a personal idiosyncrasy against a food has been manifested.
The cause and cure for this disease are still a matter of discussion. Whether it is due to the presence or absence of certain substances in the food materials, is as yet to be determined.
Diet in Pellagra is most important. It is impossible to say that pellagra is a nutritional disease, but it is certain that in balancing the diet much has been done toward relieving the condition.
Diarrhea is one of the chief symptoms of the disease and great care is needed in formulating the dietary in order not to increase this condition.
Conclusion.—The diet is thus shown to be directed toward overcoming the emaciation and anemia and relieving or preventing the gastro-intestinal disturbances which are so apt to occur. It must be remembered that even a well-balanced diet will not materially relieve the condition unless it is instituted sufficiently early.
(a) Formulate a diet for an adult in which the base-forming elements predominate.
(b) Formulate a diet for child suffering from acidosis.
(c) Arrange a well balanced diet for pellagra in which forty grams of protein shall come from milk, meat or eggs.
[164] “Chemistry of Food and Nutrition” (revised), by Henry Sherman.
E.P. signifies edible portion; A.P. signifies as purchased.
| Key: | |
| A | Protein (N × 6.25) Per Cent |
| B | Fat Per Cent |
| C | Carbohydrate Per Cent |
| D | Fuel Value per Pound Calories |
| E | 100 Calorie Portion Grams |
| Food | A | B | C | D | E | |
| Almonds | E.P. | 21.0 | 54.9 | 17.3 | 2940 | 15 |
| A.P. | 11.5 | 30.2 | 9.5 | 1615 | 28 | |
| Apples | E.P. | .4 | .5 | 14.2 | 285 | 159 |
| A.P. | .3 | .3 | 10.8 | 214 | 212 | |
| Apricots | E.P. | 1.1 | — | 13.4 | 263 | 174 |
| A.P. | 1.0 | — | 12.6 | 247 | 184 | |
| Artichoke, French | E.P. | 3.4 | .5 | 12.0 | 300 | 151 |
| A.P. | 1.7 | .3 | 6.0 | 150 | 302 | |
| Asparagus, fresh | E.P. | 1.8 | .2 | 3.3 | 100 | 450 |
| cooked | A.P. | 2.1 | 3.3 | 2.2 | 213 | 213 |
| Avocado | E.P. | 2.1 | 20.1 | 7.4 | 993 | 46 |
| A.P. | 1.4 | 13.2 | 4.8 | 652 | 70 | |
| Bacon, smoked | E.P. | 10.5 | 64.8 | — | 2840 | 16 |
| A.P. | 9.5 | 59.4 | — | 2372 | 19 | |
| Bananas | E.P. | 1.3 | .6 | 22.0 | 447 | 101 |
| A.P. | .8 | .4 | 14.3 | 290 | 156 | |
| Barley, pearled | 8.5 | 1.1 | 77.8 | 1615 | 28 | |
| Beans, dried | 22.5 | 1.8 | 59.6 | 1565 | 29 | |
| Lima, dried | 18.1 | 1.5 | 65.9 | 1586 | 29 | |
| Lima, fresh | E.P. | 7.1 | .7 | 22.0 | 557 | 82 |
| A.P. | 3.2 | .3 | 9.9 | 250 | 182 | |
| string, fresh | E.P. | 2.3 | 3.0 | 7.4 | 184 | 241 |
| A.P. | 2.1 | 3.0 | 6.9 | 176 | 259 | |
| baked, canned | A.P. | 6.9 | 2.5 | 19.6 | 583 | 78 |
| red kidney, canned | 7.0 | .2 | 18.5 | 471 | 96 | |
| [Pg 462]Beef, brisket, medium fat | E.P. | 15.8 | 28.5 | — | 1449 | 31 |
| A.P. | 12.0 | 22.3 | — | 1130 | 40 | |
| chuck, average | E.P. | 19.2 | 15.4 | — | 978 | 46 |
| A.P. | 15.8 | 12.5 | — | 797 | 58 | |
| corned, average | E.P. | 15.6 | 26.2 | — | 1353 | 34 |
| A.P. | 14.3 | 23.8 | — | 1230 | 37 | |
| cross ribs, average | E.P. | 15.9 | 28.2 | — | 1440 | 32 |
| A.P. | 13.8 | 24.8 | — | 1262 | 36 | |
| dried, salted, and smoked | E.P. | 30.0 | 6.5 | .4 | 817 | 56 |
| A.P. | 26.4 | 6.9 | — | 760 | 60 | |
| flank, lean | E.P. | 20.8 | 11.3 | — | 838 | 54 |
| A.P. | 20.5 | 11.0 | — | 821 | 55 | |
| fore quarter, lean | E.P. | 18.9 | 12.2 | — | 842 | 54 |
| A.P. | 14.7 | 9.5 | — | 655 | 69 | |
| fore shank, lean | E.P. | 22.0 | 6.1 | — | 647 | 70 |
| A.P. | 14.0 | 3.9 | — | 414 | 110 | |
| heart | E.P. | 16.0 | 20.4 | 1.0 | 1140 | 40 |
| A.P. | 14.8 | 24.7 | .9 | 1292 | 35 | |
| hind quarter, lean | E.P. | 20.0 | 13.4 | — | 907 | 50 |
| A.P. | 16.7 | 11.2 | — | 757 | 60 | |
| hind shank, lean | E.P. | 21.9 | 5.4 | — | 617 | 75 |
| A.P. | 9.1 | 2.2 | — | 255 | 179 | |
| hind shank, fat | E.P. | 20.4 | 18.8 | — | 1171 | 40 |
| A.P. | 9.9 | 9.1 | — | 552 | 83 | |
| liver | E.P. | 20.4 | 4.5 | 1.7 | 584 | 78 |
| A.P. | 20.2 | 3.1 | 2.5 | 537 | 85 | |
| loin | E.P. | 19.7 | 12.7 | — | 877 | 52 |
| A.P. | 17.1 | 11.1 | — | 764 | 60 | |
| neck, lean | E.P. | 21.4 | 8.4 | — | 732 | 62 |
| A.P. | 15.1 | 5.9 | — | 493 | 93 | |
| neck, medium fat | E.P. | 20.1 | 16.5 | — | 1040 | 44 |
| A.P. | 14.5 | 11.9 | — | 749 | 61 | |
| plate, lean | E.P. | 15.6 | 18.8 | — | 1051 | 43 |
| A.P. | 13.0 | 15.5 | — | 867 | 52 | |
| [Pg 463]Porterhouse steak | E.P. | 21.9 | 20.4 | — | 1230 | 37 |
| A.P. | 19.1 | 17.9 | — | 1077 | 42 | |
| rib rolls, lean | A.P. | 20.2 | 10.5 | — | 795 | 57 |
| ribs, lean | E.P. | 19.6 | 12.0 | — | 845 | 54 |
| A.P. | 15.2 | 9.3 | — | 654 | 69 | |
| ribs, fat | E.P. | 15.0 | 35.6 | — | 1721 | 26 |
| A.P. | 12.7 | 30.6 | — | 1480 | 31 | |
| round, lean | E.P. | 21.3 | 7.9 | — | 709 | 64 |
| A.P. | 19.5 | 7.3 | — | 649 | 70 | |
| round, free from visible fat | 23.2 | 2.5 | — | 512 | 87 | |
| rump, lean | E.P. | 20.9 | 13.7 | — | 940 | 49 |
| A.P. | 19.1 | 11.0 | — | 796 | 57 | |
| rump, fat | E.P. | 16.8 | 35.7 | — | 1763 | 26 |
| A.P. | 12.9 | 27.6 | — | 1361 | 33 | |
| sides, lean | E.P. | 19.3 | 13.2 | — | 890 | 51 |
| A.P. | 15.5 | 10.6 | — | 715 | 64 | |
| sirloin steak | E.P. | 18.9 | 18.5 | — | 1099 | 41 |
| A.P. | 16.5 | 16.1 | — | 960 | 48 | |
| sweetbreads | A.P. | 16.8 | 12.1 | — | 799 | 57 |
| tenderloin | A.P. | 16.2 | 24.4 | — | 1290 | 35 |
| tongue | E.P. | 18.9 | 9.2 | — | 717 | 63 |
| A.P. | 14.1 | 6.7 | — | 529 | 86 | |
| Beets, cooked | E.P. | 2.3 | .1 | 7.4 | 180 | 252 |
| fresh | E.P. | 1.6 | .1 | 9.7 | 209 | 217 |
| A.P. | 1.3 | .1 | 7.7 | 167 | 271 | |
| Blackberries | A.P. | 1.3 | 1.0 | 10.9 | 262 | 173 |
| Blackfish | E.P. | 18.7 | 1.3 | — | 393 | 116 |
| A.P. | 7.4 | .7 | — | 163 | 279 | |
| Bluefish | E.P. | 19.4 | 1.2 | — | 402 | 113 |
| A.P. | 10.0 | .6 | — | 206 | 220 | |
| Boston crackers | 11.0 | 8.5 | 71.1 | 1835 | 25 | |
| Brazil nuts | E.P. | 17.0 | 66.8 | 7.0 | 3162 | 14 |
| A.P. | 8.6 | 33.7 | 3.5 | 1591 | 28 | |
| Bread, Boston brown | 6.0 | 6.3 | 54.0 | 1345 | 34 | |
| graham | 8.9 | 1.8 | 52.1 | 1189 | 38 | |
| rolls, water | 9.0 | 3.0 | 54.2 | 1268 | 36 | |
| toasted | 11.5 | 1.6 | 61.2 | 1385 | 33 | |
| [Pg 464]white, home made | 9.1 | 1.6 | 53.3 | 1199 | 38 | |
| milk | 9.6 | 1.4 | 51.1 | 1158 | 39 | |
| Vienna | 9.4 | 1.2 | 54.1 | 1199 | 38 | |
| average white | 9.2 | 1.3 | 53.1 | 1182 | 38 | |
| whole wheat | 9.7 | .9 | 49.7 | 1113 | 41 | |
| Buckwheat flour | 6.4 | 1.2 | 77.9 | 1580 | 29 | |
| Butter | 1.0 | 85.0 | — | 3491 | 13 | |
| Buttermilk | 3.0 | .5 | 4.8 | 162 | 280 | |
| Butternuts | E.P. | 27.9 | 61.2 | 3.5 | 3065 | 15 |
| A.P. | 3.8 | 8.3 | .5 | 417 | 109 | |
| Cabbage | E.P. | 1.6 | .3 | 5.6 | 143 | 317 |
| A.P. | 1.4 | .2 | 4.8 | 121 | 376 | |
| Calf’s-foot jelly | 4.3 | — | 17.4 | 394 | 115 | |
| Carrots, fresh | E.P. | 1.1 | .4 | 9.3 | 204 | 221 |
| A.P. | .9 | .2 | 7.4 | 158 | 286 | |
| Cauliflower | A.P. | 1.8 | .5 | 4.7 | 139 | 328 |
| Celery | E.P. | 1.1 | .1 | 3.3 | 84 | 542 |
| A.P. | .9 | .1 | 2.6 | 68 | 672 | |
| Celery soup, canned | 2.1 | 2.8 | 5.0 | 243 | 187 | |
| Cerealine | 9.6 | 1.1 | 78.3 | 1640 | 28 | |
| Chard | E.P. | 3.2 | .6 | 5.0 | 173 | 262 |
| Cheese, American pale | 28.8 | 35.9 | .3 | 1990 | 23 | |
| American red | 29.6 | 38.3 | — | 2102 | 22 | |
| Cheddar | 27.7 | 36.8 | 4.1 | 2080 | 22 | |
| cottage | 20.9 | 1.0 | 4.3 | 499 | 91 | |
| full cream | 25.9 | 33.7 | 2.4 | 1890 | 24 | |
| Fromage de Brie | 15.9 | 21.0 | 1.4 | 1170 | 39 | |
| Neufchâtel | 18.7 | 27.4 | 1.5 | 1484 | 31 | |
| pineapple | 29.9 | 38.9 | 2.6 | 2180 | 21 | |
| Roquefort | 22.6 | 29.5 | 1.8 | 1645 | 28 | |
| Swiss | 27.6 | 34.9 | 1.3 | 1945 | 23 | |
| Cherries, fresh | E.P. | 1.0 | .8 | 16.7 | 354 | 128 |
| A.P. | .9 | .8 | 15.9 | 337 | 134 | |
| canned | A.P. | 1.1 | .1 | 21.1 | 407 | 112 |
| Chestnuts, fresh | E.P. | 6.2 | 5.4 | 42.1 | 1098 | 41 |
| A.P. | 5.2 | 4.5 | 35.4 | 920 | 49 | |
| [Pg 465]Chicken, broilers | E.P. | 21.5 | 2.5 | — | 493 | 92 |
| A.P. | 12.8 | 1.4 | — | 289 | 157 | |
| Chocolate | 12.9 | 48.7 | 30.3 | 2768 | 16 | |
| Cocoa | 21.6 | 28.9 | 37.7 | 2258 | 20 | |
| Cod, dressed | A.P. | 11.1 | .2 | — | 209 | 217 |
| salt | E.P. | 25.4 | .3 | — | 473 | 96 |
| A.P. | 19.0 | .4 | — | 361 | 126 | |
| Consommé, canned | A.P. | 2.5 | — | .4 | 53 | 862 |
| Corn, green, canned | 2.8 | 1.2 | 19.0 | 455 | 102 | |
| sweet, fresh | E.P. | 3.1 | 1.1 | 19.7 | 459 | 99 |
| A.P. | 1.2 | .4 | 7.7 | 178 | 255 | |
| Corn meal | 9.2 | 1.9 | 75.4 | 1620 | 28 | |
| Cowpeas, dried | 21.4 | 1.4 | 60.8 | 1550 | 29 | |
| green | E.P. | 9.4 | .6 | 22.7 | 603 | 76 |
| Crackers, butter | A.P. | 9.6 | 10.1 | 71.6 | 1887 | 23 |
| cream | A.P. | 9.7 | 12.1 | 69.7 | 1938 | 23 |
| graham | A.P. | 10.0 | 9.4 | 73.8 | 1905 | 24 |
| soda | A.P. | 9.8 | 9.1 | 73.1 | 1875 | 24 |
| water | A.P. | 10.7 | 8.8 | 71.9 | 1855 | 24 |
| Cranberries | A.P. | .4 | .6 | 9.9 | 212 | 212 |
| Cream | 2.5 | 18.5 | 4.5 | 883 | 50 | |
| Cucumbers | E.P. | .8 | .2 | 3.1 | 79 | 575 |
| A.P. | .7 | .2 | 2.6 | 68 | 666 | |
| Currants, fresh | 1.5 | — | 12.8 | 259 | 175 | |
| dried Zante | 2.4 | 1.7 | 74.2 | 1455 | 31 | |
| Dandelion greens | 2.4 | 1.0 | 10.6 | 277 | 164 | |
| Dates, dried | E.P. | 2.1 | 2.8 | 78.4 | 1575 | 29 |
| A.P. | 1.9 | 2.5 | 70.6 | 1416 | 32 | |
| Doughnuts | 6.7 | 21.0 | 53.1 | 1941 | 23 | |
| Eggplant | E.P. | 1.2 | .3 | 5.1 | 126 | 349 |
| Eggs, uncooked | E.P. | 13.4 | 10.5 | — | 672 | 68 |
| A.P. | 11.9 | 9.3 | — | 594 | 76 | |
| Farina | 11.0 | 1.4 | 76.3 | 1640 | 28 | |
| Figs, dried | 4.3 | .3 | 74.2 | 1437 | 32 | |
| Flounder | A.P. | 5.4 | .3 | — | 110 | 412 |
| E.P. | 14.2 | .6 | — | 282 | 161 | |
| Flour, rye | 6.8 | .9 | 78.7 | 1590 | 29 | |
| [Pg 466]wheat, California fine | 7.9 | 1.4 | 76.4 | 1585 | 29 | |
| wheat, entire | 13.8 | 1.9 | 71.9 | 1630 | 28 | |
| wheat, graham | 13.3 | 2.2 | 71.4 | 1628 | 28 | |
| wheat, patent baker’s grade | 13.3 | 1.5 | 72.7 | 1623 | 28 | |
| wheat, straight grade | 10.8 | 1.1 | 74.8 | 1608 | 28 | |
| wheat, average high and medium | 11.4 | 1.0 | 75.1 | 1610 | 28 | |
| wheat, average low grade | 14.0 | 1.9 | 71.2 | 1625 | 28 | |
| Fowls | E.P. | 19.3 | 16.3 | — | 1017 | 45 |
| A.P. | 13.7 | 12.3 | — | 752 | 60 | |
| Gelatin | 91.4 | .1 | — | 1660 | 27 | |
| Grape butter | 1.2 | .1 | 58.5 | 1088 | 42 | |
| Grapes | E.P. | 1.3 | 1.6 | 19.2 | 437 | 104 |
| A.P. | 1.0 | 1.2 | 14.4 | 328 | 138 | |
| Grapefruit | E.P. | .6 | .1 | 12.2 | 235 | 193 |
| A.P. | .4 | .1 | 8.9 | 172 | 264 | |
| Haddock | E.P. | 17.2 | .3 | — | 324 | 140 |
| A.P. | 8.4 | .2 | — | 160 | 283 | |
| Halibut steaks | E.P. | 18.6 | 5.2 | — | 550 | 83 |
| A.P. | 15.3 | 4.4 | — | 457 | 100 | |
| Ham, fresh lean | E.P. | 25.0 | 14.4 | — | 1042 | 44 |
| A.P. | 24.8 | 14.2 | — | 1030 | 44 | |
| fresh, medium | E.P. | 15.3 | 28.9 | — | 1458 | 31 |
| A.P. | 13.5 | 25.9 | — | 1303 | 35 | |
| smoked, lean | E.P. | 19.8 | 20.8 | — | 1209 | 38 |
| A.P. | 17.5 | 18.5 | — | 1073 | 42 | |
| Herring, whole | E.P. | 19.5 | 7.1 | — | 644 | 70 |
| A.P. | 11.2 | 3.9 | — | 362 | 125 | |
| smoked | E.P. | 36.9 | 15.8 | — | 1315 | 35 |
| A.P. | 20.5 | 8.8 | — | 731 | 62 | |
| Hominy | 8.3 | .6 | 79.0 | 1609 | 28 | |
| Honey | .4 | — | 81.2 | 1481 | 31 | |
| Huckleberries | .6 | .6 | 16.6 | 336 | 135 | |
| Kohl-rabi | E.P. | 2.0 | .1 | 5.5 | 140 | 324 |
| Koumiss | 2.8 | 2.1 | 5.4 | 234 | 194 | |
| [Pg 467]Lamb, breast | E.P. | 19.1 | 23.6 | — | 1311 | 35 |
| A.P. | 15.4 | 19.1 | — | 1058 | 43 | |
| chops, broiled | E.P. | 21.7 | 29.9 | — | 1614 | 28 |
| fore quarter | E.P. | 18.3 | 25.8 | — | 1385 | 33 |
| A.P. | 14.9 | 21.0 | — | 1127 | 40 | |
| hind quarter | E.P. | 19.6 | 19.1 | — | 1149 | 40 |
| A.P. | 16.5 | 16.1 | — | 953 | 48 | |
| leg roast | 19.7 | 12.7 | — | 876 | 52 | |
| side | E.P. | 17.6 | 23.1 | — | 1263 | 36 |
| A.P. | 14.1 | 18.7 | — | 1015 | 45 | |
| Lard, refined | — | 100.0 | — | 4080 | 11 | |
| Lemon juice | — | — | 9.8 | 178 | 255 | |
| Lemons | E.P. | 1.0 | .7 | 8.5 | 201 | 226 |
| A.P. | .7 | .5 | 5.9 | 140 | 323 | |
| Lettuce | E.P. | 1.2 | .3 | 2.9 | 87 | 525 |
| A.P. | 1.0 | .2 | 2.5 | 72 | 633 | |
| Liver, beef | E.P. | 20.4 | 4.5 | 1.7 | 583 | 78 |
| A.P. | 20.2 | 3.1 | 2.5 | 538 | 84 | |
| veal | E.P. | 19.0 | 5.3 | — | 562 | 81 |
| Lobster, whole | E.P. | 16.4 | 1.8 | .4 | 379 | 120 |
| A.P. | 5.9 | .7 | .2 | 139 | 326 | |
| canned | A.P. | 18.1 | 1.1 | .5 | 382 | 119 |
| Macaroni | 13.4 | .9 | 74.1 | 1625 | 28 | |
| Macaroons | 6.5 | 15.2 | 65.2 | 1922 | 24 | |
| Mackerel | E.P. | 18.7 | 7.1 | — | 629 | 72 |
| A.P. | 10.2 | 4.2 | — | 356 | 127 | |
| salt | E.P. | 21.1 | 22.6 | — | 1305 | 35 |
| A.P. | 16.3 | 17.4 | — | 1005 | 45 | |
| Marmalade, orange | .6 | .1 | 84.5 | 1548 | 29 | |
| Milk, condensed, sweetened | 8.8 | 8.3 | 54.1 | 1480 | 31 | |
| skimmed | 3.4 | .3 | 5.1 | 167 | 273 | |
| whole | 3.3 | 4.0 | 5.0 | 314 | 145 | |
| Mince meat, commercial | 6.7 | 1.4 | 60.2 | 1280 | 36 | |
| home made | 4.8 | 6.7 | 32.1 | 942 | 48 | |
| Molasses, cane | 2.4 | — | 69.3 | 1302 | 35 | |
| Mushrooms | A.P. | 3.5 | .4 | 6.8 | 204 | 223 |
| Muskmelons | E.P. | .6 | — | 9.3 | 180 | 252 |
| A.P. | .3 | — | 4.6 | 89 | 510 | |
| [Pg 468]Mutton, fore quarter | E.P. | 15.6 | 30.9 | — | 1543 | 29 |
| A.P. | 12.3 | 24.5 | — | 1223 | 37 | |
| hind quarter | E.P. | 16.7 | 28.1 | — | 1450 | 31 |
| A.P. | 13.8 | 23.2 | — | 1197 | 38 | |
| leg | E.P. | 19.8 | 12.4 | — | 863 | 52 |
| A.P. | 16.5 | 10.3 | — | 718 | 63 | |
| side | A.P. | 13.0 | 24.0 | — | 1215 | 37 |
| E.P. | 16.2 | 29.8 | — | 1512 | 30 | |
| Nectarines | E.P. | .6 | — | 15.9 | 299 | 152 |
| A.P. | .6 | — | 14.8 | 280 | 162 | |
| Oatmeal | 16.1 | 7.2 | 67.5 | 1811 | 25 | |
| Okra | E.P. | 1.6 | .2 | 7.4 | 172 | 264 |
| A.P. | 1.4 | .2 | 6.5 | 152 | 300 | |
| Olives, green | E.P. | 1.1 | 27.6 | 11.6 | 1357 | 33 |
| A.P. | .8 | 20.2 | 8.5 | 995 | 46 | |
| ripe | E.P. | 1.7 | 25.0 | 4.3 | 1130 | 40 |
| A.P. | 1.4 | 21.0 | 3.5 | 947 | 48 | |
| Onions, fresh | E.P. | 1.6 | .3 | 9.9 | 220 | 206 |
| A.P. | 1.4 | .3 | 8.9 | 199 | 228 | |
| Oranges | E.P. | .8 | .2 | 11.6 | 233 | 195 |
| A.P. | .6 | .1 | 8.5 | 169 | 268 | |
| Oxtail soup, canned | A.P. | 3.8 | .5 | 4.2 | 166 | 274 |
| Oysters | E.P. | 6.2 | 1.2 | 3.7 | 228 | 199 |
| in shell | A.P. | 1.2 | .2 | .7 | 43 | 1065 |
| canned | A.P. | 8.8 | 2.4 | 3.9 | 328 | 138 |
| Parsnips | E.P. | 1.6 | .5 | 13.5 | 294 | 154 |
| A.P. | 1.3 | .4 | 10.8 | 236 | 192 | |
| Pea soup, canned | A.P. | 3.6 | .7 | 7.6 | 232 | 196 |
| Peaches, canned | A.P. | .7 | .1 | 10.8 | 213 | 213 |
| fresh | E.P. | .7 | .1 | 9.4 | 188 | 242 |
| A.P. | .5 | .1 | 7.7 | 153 | 297 | |
| Peanuts | E.P. | 25.8 | 38.6 | 24.4 | 2490 | 18 |
| A.P. | 19.5 | 29.1 | 18.5 | 1877 | 24 | |
| Pears, fresh | E.P. | .6 | .5 | 14.1 | 288 | 158 |
| A.P. | .5 | .4 | 12.7 | 256 | 177 | |
| Peas, canned | A.P. | 3.6 | .2 | 9.8 | 252 | 180 |
| dried | 24.6 | 1.0 | 62.0 | 1611 | 28 | |
| green | E.P. | 7.0 | .5 | 16.9 | 454 | 100 |
| A.P. | 3.6 | .2 | 9.8 | 252 | 180 | |
| [Pg 469]Peppers, green | E.P. | 1.1 | .1 | 4.6 | 109 | 417 |
| Persimmons | E.P. | .8 | .7 | 31.5 | 615 | 74 |
| Pies, apple | 3.1 | 0.8 | 42.8 | 1233 | 37 | |
| custard | 4.2 | 6.3 | 26.1 | 806 | 56 | |
| lemon | 3.6 | 10.1 | 37.4 | 1156 | 39 | |
| mince | 5.8 | 12.3 | 38.1 | 1300 | 35 | |
| squash | 4.4 | 8.4 | 21.7 | 817 | 56 | |
| Pineapples, fresh | E.P. | .4 | .3 | 9.7 | 196 | 232 |
| canned | A.P. | .4 | .7 | 36.4 | 695 | 65 |
| Pine nuts (pignolias) | 33.9 | 49.4 | 6.9 | 2757 | 16 | |
| Pistachios, shelled | 22.3 | 54.0 | 16.3 | 2900 | 16 | |
| Plums | E.P. | 1.0 | — | 20.1 | 383 | 118 |
| A.P. | .9 | — | 19.1 | 363 | 125 | |
| Pomegranates | E.P. | 1.5 | 1.6 | 19.5 | 447 | 102 |
| Pork chops, medium | E.P. | 16.6 | 30.1 | — | 1530 | 30 |
| A.P. | 13.4 | 24.2 | — | 1230 | 37 | |
| chuck ribs and shoulder | E.P. | 17.3 | 31.1 | — | 1585 | 29 |
| A.P. | 14.1 | 25.5 | — | 1298 | 35 | |
| fat, salt | A.P. | 1.9 | 86.2 | — | 3555 | 13 |
| sausage | A.P. | 13.0 | 44.2 | 1.1 | 2030 | 22 |
| side | E.P. | 9.1 | 55.3 | — | 2423 | 19 |
| A.P. | 8.0 | 49.0 | — | 2145 | 21 | |
| tenderloin | A.P. | 18.9 | 13.0 | — | 875 | 52 |
| Potato chips | A.P. | 6.8 | 39.8 | 46.7 | 2598 | 17 |
| Potatoes, white, raw | E.P. | 2.2 | .1 | 18.4 | 378 | 120 |
| A.P. | 1.8 | .1 | 14.7 | 302 | 149 | |
| sweet, raw | E.P. | 1.8 | .7 | 27.4 | 558 | 81 |
| A.P. | 1.4 | .6 | 21.9 | 447 | 102 | |
| Prunes, dried | E.P. | 2.1 | — | 73.3 | 1368 | 33 |
| A.P. | 1.8 | — | 62.2 | 1160 | 39 | |
| Pumpkins | E.P. | 1.0 | .1 | 5.2 | 117 | 389 |
| A.P. | .5 | .1 | 2.6 | 60 | 753 | |
| Radishes | E.P. | 1.3 | .1 | 5.8 | 133 | 341 |
| A.P. | .9 | .1 | 4.0 | 91 | 488 | |
| Raisins | E.P. | 2.6 | 3.3 | 76.1 | 1562 | 29 |
| A.P. | 2.3 | 3.0 | 68.5 | 1407 | 32 | |
| [Pg 470]Raspberries, red | 1.0 | — | 12.6 | 247 | 184 | |
| black | 1.7 | 1.0 | 12.6 | 300 | 151 | |
| Rhubarb | E.P. | .6 | .7 | 3.6 | 105 | 433 |
| A.P. | .4 | .4 | 2.2 | 63 | 714 | |
| Rice | 8.0 | .3 | 79.0 | 1591 | 29 | |
| Salmon, dressed | A.P. | 13.8 | 8.1 | — | 582 | 78 |
| whole | E.P. | 22.0 | 12.8 | — | 923 | 49 |
| A.P. | 15.3 | 8.9 | — | 642 | 71 | |
| Sausage, Bologna | E.P. | 18.7 | 17.6 | .3 | 1061 | 43 |
| A.P. | 18.2 | 19.7 | — | 1135 | 40 | |
| farmer | E.P. | 29.0 | 42.0 | — | 2240 | 20 |
| A.P. | 27.9 | 40.4 | — | 2156 | 21 | |
| Shad, whole | E.P. | 18.8 | 9.5 | — | 727 | 61 |
| A.P. | 9.4 | 4.8 | — | 367 | 124 | |
| roe | 20.9 | 3.8 | 2.6 | 582 | 78 | |
| Shredded wheat | 10.5 | 1.4 | 77.9 | 1660 | 27 | |
| Spinach, fresh | A.P. | 2.1 | .3 | 3.2 | 109 | 417 |
| Squash | E.P. | 1.4 | .5 | 9.0 | 209 | 217 |
| A.P. | .7 | .2 | 4.5 | 103 | 443 | |
| Strawberries | 1.0 | .6 | 7.4 | 169 | 269 | |
| Succotash, canned | 3.6 | 1.0 | 18.6 | 444 | 102 | |
| Sugar | — | — | 100.0 | 1815 | 25 | |
| Tomatoes, fresh | A.P. | .9 | .4 | 3.9 | 104 | 438 |
| canned | A.P. | 1.2 | .2 | 4.0 | 103 | 443 |
| Tuna (tunny fish) | E.P. | 26.6 | 11.4 | — | 946 | 48 |
| Turkey | E.P. | 21.1 | 22.9 | — | 1320 | 34 |
| A.P. | 16.1 | 18.4 | — | 1042 | 43 | |
| sandwich, canned | 20.7 | 29.2 | — | 1568 | 29 | |
| Turnips | E.P. | 1.3 | .2 | 8.1 | 178 | 256 |
| A.P. | .9 | .1 | 5.7 | 124 | 367 | |
| Veal, breast | E.P. | 20.3 | 11.0 | — | 817 | 56 |
| A.P. | 15.3 | 8.6 | — | 629 | 72 | |
| cutlet | E.P. | 20.3 | 7.7 | — | 683 | 66 |
| A.P. | 20.1 | 7.5 | — | 670 | 68 | |
| fore quarter | E.P. | 20.0 | 8.0 | — | 690 | 66 |
| A.P. | 15.1 | 6.0 | — | 517 | 88 | |
| hind quarter | E.P. | 20.7 | 8.3 | — | 715 | 64 |
| A.P. | 16.2 | 6.6 | — | 534 | 85 | |
| side | E.P. | 20.2 | 8.1 | — | 697 | 65 |
| A.P. | 15.6 | 6.3 | — | 539 | 84 | |
| [Pg 471]Vegetable soup, canned | 2.9 | — | .5 | 62 | 735 | |
| Walnuts, California or English | E.P. | 18.4 | 64.4 | 13.0 | 3199 | 14 |
| A.P. | 4.9 | 17.3 | 3.5 | 859 | 53 | |
| black | E.P. | 27.6 | 56.3 | 11.7 | 3011 | 15 |
| A.P. | 7.2 | 14.6 | 3.0 | 780 | 59 | |
| Watermelons | E.P. | .4 | .2 | 6.7 | 136 | 332 |
| A.P. | .2 | .1 | 2.7 | 57 | 800 | |
| Wheat, cracked | 11.1 | 1.7 | 75.5 | 1635 | 28 | |
| Whitefish | E.P. | 22.9 | 6.5 | — | 680 | 67 |
| A.P. | 10.6 | 3.0 | — | 315 | 144 | |
| Zwieback | 9.8 | 9.9 | 73.5 | 1915 | 24 | |
[165] Courtesy of Dr. Henry Sherman.
[166] The percentages of nutrients are taken from Bull. 28, Office of Experiment Stations, U. S. Department of Agriculture. The fuel values are calculated from these percentages by the use of the factors explained in Chapter II, viz.—protein, 4 calories; fat, 9 calories; carbohydrate, 4 calories per gram.
(Compiled from various sources)
| Key: | |
| A | Calcium (Ca) |
| B | Magnesium (Mg) |
| C | Potassium (K) |
| D | Sodium (Na) |
| E | Phosphorus (P) |
| F | Chlorine (Cl) |
| G | Sulphur (S) |
| H | Iron (Fe) |
| Food | A | B | C | D | E | F | G | H |
| Almonds | .239 | .251 | .741 | .019 | .465 | .037 | .160 | .00390 |
| Apples | .007 | .008 | .127 | .011 | .012 | .005 | .006 | .00030 |
| dried | .032 | .037 | (.623) | (.050) | .048 | (.025) | ? | (.0015) |
| Apricots | .014 | .010 | .248 | .038 | .025 | .002 | .010 | (.0003) |
| dried | (.066) | (.047) | (1.157) | (.177) | (.117) | (.009) | ? | (.0014) |
| Asparagus | .025 | .011 | .196 | .007 | .039 | .039 | .041 | .00100 |
| Bacon (See Meat) | ||||||||
| Bananas | .009 | .028 | .401 | .034 | .031 | .125 | .010 | .00060 |
| Barley, entire | .043 | .141 | .477 | .076 | .400 | .016 | .153 | .00410 |
| pearled | .020 | (.070) | (.241) | (.037) | .181 | (.016) | (.120) | (.0020) |
| Beans, dried | .160 | .156 | 1.229 | .097 | .471 | .032 | .215 | .00700 |
| kidney, dry | .132 | .139 | 1.144 | .041 | .475 | .041 | .227 | .00720 |
| Lima, dry | .071 | .188 | 1.741 | .249 | .338 | .026 | .161 | .00700 |
| Lima, fresh | .028 | (.070) | (.613) | (.088) | .133 | (.009) | (.057) | .00200 |
| string, fresh | .046 | .025 | .240 | .019 | .052 | .024 | .030 | .00110 |
| Beef (See Meat) | ||||||||
| Beer | .004 | .008 | .058 | .013 | .028 | .006 | .015 | .00010 |
| Beets | .029 | .021 | .353 | .093 | .039 | .058 | .016 | .00060 |
| Blackberries | .017 | .021 | .169 | (.007) | .034 | (.010) | .020 | .00060 |
| Blood (avg.) | .008 | .004 | .075 | .261 | .031 | .280 | .137 | .05260 |
| Blueberries | .020 | .007 | .051 | .016 | .008 | .008 | .011 | .00090 |
| Bluefish (See Fish) | ||||||||
| Bread, Boston brown | .129 | .078 | (.232) | (.394) | .185 | (.607) | .201 | (.0030) |
| entire wheat | (.05) | (.05) | (.208) | (.394) | (.175) | (.607) | (.120) | (.0016) |
| graham | (.05) | (.05) | (.291) | (.394) | (.218) | (.607) | .150 | (.0025) |
| rye | .024 | .039 | .151 | .701 | .148 | 1.025 | .104 | (.0016) |
| white | .027 | .023 | .108 | (.394) | .093 | (.607) | .105 | .00090 |
| Breadfruit | .084 | .007 | .235 | .027 | .068 | .100 | .049 | |
| Brussels sprouts | .027 | .040 | .375 | .004 | .120 | .040 | .194 | (.0011) |
| Buckwheat flour | .039 | .048 | .130 | .027 | .226 | .012 | .071 | .00120 |
| Butter | .015 | .001 | .014 | (.788) | .017 | (1.212) | (.010) | .00020 |
| Buttermilk | .105 | .016 | .151 | .064 | .097 | .099 | .026 | .00025 |
| Cabbage | .045 | .015 | .247 | .027 | .029 | .024 | .066 | .00110 |
| Cabbage greens | .106 | .030 | .512 | .025 | .099 | .068 | .173 | .00180 |
| Cantaloupe | .017 | .012 | .235 | .061 | .015 | .041 | .014 | .00030 |
| Capers | .122 | .022 | .209 | .051 | .062 | — | — | — |
| Carp (See Fish) | ||||||||
| Carrots | .056 | .021 | .287 | .101 | .046 | .036 | .022 | .00060 |
| Cauliflower | .123 | .014 | .222 | .068 | .061 | .050 | .086 | .00060 |
| Caviar | .137 | .022 | .422 | .874 | .176 | 1.819 | — | — |
| [Pg 473]Celery | .078 | .014 | .316 | .084 | .037 | .156 | .022 | .00050 |
| Chard | .150 | .071 | .318 | .086 | .040 | .039 | .124 | (.0025) |
| Cheese | .931 | .037 | .089 | .606 | .683 | .880 | .263 | .00130 |
| Cherries | .019 | .016 | .213 | .023 | .031 | .014 | .011 | .00040 |
| Cherry juice | .017 | .011 | .200 | .013 | .018 | .003 | .006 | (.0003) |
| Chestnuts | .034 | .051 | .560 | .065 | .093 | .006 | .068 | .00070 |
| Chicken (See Meat) | ||||||||
| Chocolate | .092 | (.293) | (.563) | .012 | .455 | (.051) | .085 | (.0027) |
| Cider | .008 | .011 | .095 | .020 | .009 | .006 | .006 | (.0002) |
| Citron | .121 | .018 | .210 | .011 | .033 | .003 | .020 | — |
| Clams, round | .106 | .098 | .131 | .705 | .046 | 1.220 | .224 | — |
| soft, long | .124 | .079 | .212 | .500 | .122 | .910 | .213 | — |
| Cocoa | .112 | .420 | .900 | .059 | .709 | .051 | .203 | .00270 |
| Coconut, dried | .059 | .059 | .597 | .073 | .155 | .239 | (.056) | — |
| fresh | .024 | .020 | .300 | .036 | .074 | .120 | .028 | — |
| Coconut milk | .020 | .009 | .144 | — | .010 | — | .008 | — |
| Cod (See Fish) | ||||||||
| Corn (maize), mature | .020 | .121 | .339 | .036 | .283 | .045 | .151 | .00290 |
| meal | .018 | .084 | .213 | .039 | .190 | .146 | .111 | .00090 |
| sweet | .006 | .033 | .113 | .040 | .103 | .014 | .046 | .00080 |
| sweet, dried | .021 | .121 | .414 | .146 | .376 | .050 | .167 | .00290 |
| Cotton seed meal | .265 | .462 | 1.390 | .234 | 1.193 | .037 | .485 | — |
| Cowpeas | .100 | .208 | 1.402 | .161 | .456 | .040 | .240 | — |
| Crackers | .022 | .011 | .100 | (.594) | .102 | (.910) | .125 | .00150 |
| Cranberries | .018 | .007 | .077 | .010 | .013 | .009 | .007 | .00060 |
| Cream | .086 | .010 | .126 | .035 | .067 | .080 | .030 | .00022 |
| Cucumbers | .016 | .009 | .140 | .010 | .033 | .030 | .020 | .00020 |
| Currants, dried | .082 | .044 | .873 | .081 | .195 | .060 | .044 | (.0025) |
| fresh | .026 | .017 | .211 | .007 | .038 | .006 | .014 | .00050 |
| Currant juice | .021 | .010 | .185 | (.006) | .018 | .004 | .005 | — |
| Dandelion | .105 | .036 | .461 | .168 | .072 | .099 | .017 | .00270 |
| Dates | .065 | .069 | .611 | .055 | .056 | .228 | .070 | .00300 |
| Duck (See Meat) | ||||||||
| Eggplant | .011 | .015 | (.140) | (.010) | .034 | .024 | .016 | .00050 |
| Eggs | .067 | .011 | .140 | .143 | .180 | .106 | .195 | .00300 |
| Egg white | .015 | .010 | .160 | .156 | .014 | .155 | .216 | .00010 |
| Egg yolk | .137 | .016 | .115 | .075 | .524 | .094 | .166 | .00860 |
| Endive | .104 | .013 | .380 | .109 | .038 | .167 | .035 | — |
| Farina | .021 | .025 | .120 | .065 | .125 | .076 | .155 | .00080 |
| Figs, dried | .162 | .071 | .964 | .046 | .116 | .043 | .056 | .00300 |
| fresh | .053 | .022 | .303 | .012 | .036 | .014 | .010 | — |
| Fish[168] | ||||||||
| [Pg 474]Flaxseed | .204 | .252 | .901 | .050 | .627 | .022 | .170 | — |
| Flour, buckwheat | .010 | .048 | .130 | .027 | .176 | .012 | .071 | .00120 |
| entire wheat | .031 | (.090) | (.274) | (.037) | .238 | (.070) | (.180) | .00250 |
| graham | .039 | (.133) | (.457) | (.037) | .364 | (.070) | .183 | .00370 |
| white | .020 | .018 | .115 | .060 | .092 | .074 | .177 | .00100 |
| rye | .018 | .081 | .463 | .019 | .289 | .055 | .123 | .00130 |
| Fowl (See Meat) | ||||||||
| Gluten feed | .247 | .221 | .250 | .420 | .542 | .090 | .558 | — |
| Goose (See Meat) | ||||||||
| Gooseberries | .035 | .014 | .197 | .038 | .031 | — | .011 | .00050 |
| Grapefruit | .021 | .009 | .161 | .004 | .020 | .005 | .010 | .00030 |
| Grape juice | .011 | .009 | .106 | .005 | .011 | .002 | .009 | .00030 |
| Grapes | .019 | .010 | .197 | .015 | .031 | .005 | .024 | .00030 |
| Guava | .014 | .008 | .384 | — | .030 | .045 | — | — |
| Haddock (See Fish) | ||||||||
| Halibut (See Fish) | ||||||||
| Ham (See Meat) | ||||||||
| Hazelnuts | .287 | .140 | .618 | .019 | .354 | .067 | .198 | .00410 |
| Herring (See Fish) | ||||||||
| Hominy | .011 | .058 | .174 | .020 | .144 | .046 | (.136) | (.0009) |
| Honey | .004 | .018 | .386 | .001 | .019 | .029 | .001 | .00070 |
| Horseradish | .096 | .039 | .468 | .062 | .076 | .016 | .190 | — |
| Huckleberries | .020 | .007 | .051 | .016 | .008 | .008 | .011 | .00090 |
| Huckleberry wine | .009 | .004 | .042 | .006 | .004 | .001 | .006 | — |
| Jam[169] | ||||||||
| Jelly | .014 | (.010) | (.100) | (.013) | .008 | (.004) | (.007) | (.0003) |
| Kohl-rabi | .077 | .033 | .370 | .050 | .071 | .053 | .057 | .00060 |
| Lamb (See Meat) | ||||||||
| Leeks | .058 | .014 | .199 | .081 | .006 | .024 | .072 | — |
| Lemons | .036 | .007 | .175 | .004 | .022 | .002 | .011 | .00060 |
| Lemon juice | .024 | .010 | .127 | .009 | .010 | .003 | .006 | — |
| Lemon, sweet | .030 | .006 | .442 | — | .042 | .013 | .016 | — |
| Lentils, dry | .107 | .101 | .877 | .062 | .438 | .050 | .277 | .00860 |
| Lettuce | .043 | .017 | .339 | .027 | .042 | .074 | .014 | .00070 |
| Limes | .055 | .014 | .350 | .062 | .036 | .039 | .011 | — |
| Lime juice | — | — | — | — | — | — | .003 | — |
| Linseed meal | .413 | .432 | 1.083 | .251 | .741 | .085 | .396 | — |
| Lupins, dry | .191 | .191 | .840 | .073 | .520 | .034 | — | — |
| fresh | .053 | .022 | .303 | .012 | .036 | .014 | .010 | — |
| [Pg 475]Macaroni | .022 | .037 | .130 | .008 | .144 | .073 | .172 | .00120 |
| Mackerel (See Fish) | ||||||||
| Mamey | .009 | .012 | .345 | — | .028 | .140 | — | — |
| Mango | .021 | .007 | .235 | — | .017 | .019 | .013 | — |
| Mangolds | .026 | .030 | .334 | .071 | .038 | .082 | .026 | — |
| Maple syrup | .107 | .034 | .208 | .010 | .013 | (.010) | (.005) | (.003) |
| Meat[170] | ||||||||
| Meat extract, solid | .085 | .363 | 7.347 | 2.394 | 2.800 | 3.117 | — | — |
| Meat peptone | .025 | .124 | 2.440 | .641 | 1.130 | .561 | .222 | — |
| Milk (cow’s), whole | .120 | .012 | .143 | .051 | .093 | .106 | .034 | .00024 |
| skimmed | (.122) | (.012) | (.149) | (.052) | (.096) | (.110) | (.035) | .00025 |
| condensed | (.300) | (.032) | (.374) | (.134) | .235 | (.280) | (.090) | .00060 |
| buffalo | .203 | .016 | .099 | .038 | .125 | .062 | — | — |
| camel’s | .143 | .021 | .114 | .019 | .098 | .105 | — | — |
| goat’s | .128 | .013 | .145 | .079 | .103 | .014 | .037 | — |
| human | .034 | .005 | .047 | .010 | .015 | .035 | — | — |
| mare’s | .083 | .007 | .081 | .010 | .054 | .029 | — | — |
| sheep’s | .207 | .008 | .187 | .030 | .123 | .071 | — | — |
| Millet | .014 | .167 | .290 | .085 | .327 | .019 | — | — |
| Molasses | .211 | .068 | 1.349 | .019 | .044 | .317 | .129 | .00730 |
| Mushrooms | .017 | .016 | .384 | .027 | .108 | .021 | .051 | — |
| Muskmelon | .017 | .012 | .235 | .061 | .015 | .041 | .014 | .00030 |
| Mustard | .492 | .260 | .761 | .056 | .755 | .016 | 1.230 | — |
| Mutton (See Meat) | ||||||||
| Oatmeal | .069 | .110 | .344 | .062 | .392 | .069 | .202 | .00380 |
| Okra | .071 | .010 | .035 | .043 | .019 | — | — | — |
| Olives | .122 | .002 | 1.526 | .128 | .014 | .004 | .027 | .00290 |
| Onions | .034 | .016 | .178 | .016 | .045 | .021 | .070 | .00060 |
| Oranges | .045 | .012 | .177 | .012 | .021 | .006 | .011 | .00020 |
| Orange juice | .029 | .011 | .182 | .008 | .016 | .003 | .009 | .00020 |
| Oysters | .052 | .037 | .091 | .459 | .155 | .590 | .187 | .00450 |
| Paprika | .229 | .164 | 2.075 | .178 | .341 | .155 | — | — |
| Parsnips | .059 | .034 | .518 | .004 | .076 | .030 | .036 | .00060 |
| Peaches | .016 | .010 | .214 | .022 | .024 | .004 | .009 | .00030 |
| dried | .034 | .056 | (.830) | .082 | .146 | — | .212 | (.0012) |
| Peanuts | .071 | .180 | .654 | .050 | .399 | .056 | .224 | .00200 |
| Pears | .015 | .011 | .132 | .016 | .026 | .011 | .010 | .00030 |
| Pear juice | .009 | .008 | 1.400 | — | .011 | — | .009 | — |
| Peas, dried | .084 | .149 | .903 | .104 | .400 | .035 | .219 | .00570 |
| fresh | .028 | .038 | .285 | .013 | .127 | .024 | .063 | .00170 |
| Pecan nuts | .089 | .152 | (.332) | — | .335 | .050 | .113 | .00260 |
| [Pg 476]Pepper, green, fresh | .006 | .010 | (.139) | — | .026 | .013 | .014 | .00040 |
| Pepper, black, dry | .440 | .156 | 1.140 | .131 | .188 | .312 | — | — |
| Pepper, white, dry | .425 | .113 | — | — | .233 | .029 | — | — |
| Perch (See Fish) | ||||||||
| Persimmons | .022 | .009 | .292 | .011 | .021 | .002 | .005 | — |
| Pineapple | .018 | .011 | .321 | .016 | .028 | .051 | .009 | .00050 |
| Plums | .020 | .011 | .203 | .019 | .032 | .002 | .009 | .00050 |
| Pomegranate | .011 | .005 | .063 | .085 | .105 | .003 | — | .00040 |
| Pork (See Meat) | ||||||||
| Potatoes | .014 | .028 | .429 | .021 | .058 | .038 | .030 | .00130 |
| sweet | .019 | .028 | .397 | .039 | .045 | .094 | .024 | .00050 |
| Prunes, dried | .054 | .055 | 1.030 | .069 | .105 | .017 | .037 | .00300 |
| Pumpkin | .023 | .008 | (.320) | .065 | .059 | — | .021 | (.0008) |
| Radishes | .021 | .012 | .218 | .069 | .029 | .054 | .041 | .00060 |
| Raisins | .064 | .083 | .820 | .133 | .132 | .082 | .051 | .00210 |
| Raspberries | .049 | .024 | .173 | — | .052 | — | .017 | .00060 |
| Raspberry juice | .021 | .016 | .134 | .005 | .012 | — | .009 | — |
| Rhubarb | .044 | .017 | .325 | .025 | .031 | .036 | .013 | .00100 |
| Rice, brown | — | — | — | — | .207 | — | — | .00200 |
| white | .009 | .033 | .070 | .025 | .096 | .054 | .117 | .00090 |
| Romaine (salad) | .045 | .032 | .306 | .016 | .053 | .073 | .019 | — |
| Rutabagas | .074 | .018 | .399 | .083 | .056 | .058 | .083 | — |
| Rye, entire (See also Bread and Flour) | .055 | .130 | .453 | .035 | .385 | .025 | .170 | .00390 |
| Salmon (See Fish) | ||||||||
| Sapota | .026 | .008 | .179 | — | .006 | .087 | — | — |
| Shredded wheat | .041 | .144 | — | — | .324 | — | — | .00450 |
| Shrimp | .096 | — | — | — | — | — | — | — |
| Soup, canned | .036 | — | .033 | — | .030 | — | — | — |
| canned vegetable | .025 | .013 | .101 | — | .038 | — | .025 | — |
| Spinach | .067 | .037 | .774 | .125 | .068 | .074 | .038 | .00360 |
| Squash, summer, seeds removed | .018 | .008 | .150 | .002 | — | — | — | (.0006) |
| with seeds | .024 | .012 | .180 | .004 | — | — | — | (.0006) |
| Squash, winter | .019 | .011 | .320 | .004 | — | — | — | (.0006) |
| Strawberries | .041 | .019 | .147 | .050 | .028 | .006 | .014 | .00080 |
| Tamarind | .007 | .021 | — | — | .072 | .007 | .009 | — |
| [Pg 477]Tapioca | .023 | — | — | — | .090 | .018 | .029 | .00160 |
| Tomatoes | .011 | .010 | .275 | .010 | .026 | .034 | .014 | .00040 |
| Tomato juice | .006 | .010 | .310 | .015 | .015 | .055 | — | — |
| Truffles | .024 | .018 | .404 | .077 | .062 | .039 | — | — |
| Turnips | .064 | .017 | .338 | .056 | .046 | .041 | .065 | .00050 |
| Turnip tops | .347 | .028 | .307 | .082 | .049 | .168 | .069 | — |
| Veal (See Meat) | ||||||||
| Vinegar (cider) | .016 | .008 | .165 | — | .013 | — | .017 | (.0003) |
| Walnuts | .089 | .134 | (.332) | — | .358 | .040 | .172 | .00210 |
| Water cress | .187? | .034 | .287 | .099 | .005 | .061 | .167 | .00190 |
| Watermelon | .011 | .003 | .073 | .008 | .003 | .008 | .007 | — |
| Wheat, entire (See also Bread and Flour) | .045 | .133 | .473 | .039 | .423 | .068 | .181 | .00500 |
| Wheat bran | .120 | .511 | 1.217 | .154 | 1.215 | .090 | .247 | .00780 |
| Wheat germ | .071 | .342 | .296 | .722 | 1.050 | .070 | .325 | — |
| Wheat gluten | .078 | .045 | .007 | .028 | 2.000 | .050 | .920 | — |
| Whey | .044 | .008 | .157 | .038 | .035 | .119 | .009 | ? |
| Whortleberries, entire | .031 | .021 | .261 | .021 | .042 | — | — | — |
| flesh only | .020 | .011 | .087 | — | .018 | — | — | — |
| Wine (avg.) | .009 | .010 | .104 | .008 | .015 | .011 | .015 | (.0003) |
[167] From Sherman’s “Chemistry of Food and Nutrition,” by courtesy of the author.
[168] Average fish is estimated to contain per 100 grams of protein as follows: 0.109 gram Ca; 0.133 gram Mg; 1.671 grams K; 0.373 gram Na; 1.148 grams P; 0.528 gram Cl; 1.119 grams S; 0.0055 gram Fe.
[169] The percentages of the ash constituents in jams are believed to average about two thirds those of the corresponding fruits.
[170] Average meat is estimated to contain per 100 grams protein as follows: 0.058 gram Ca; 0.118 gram Mg; 1.694 grams K; 0.421 gram Na; 1.078 grams P; 0.378 gram Cl; 1.146 grams S; 0.0150 gram Fe.
| Key: | |
| A | Protein Calories |
| B | Protein Grams |
| C | Nitrogen Grams |
| D | Calcium Grams |
| E | Phosphorus Grams |
| F | Iron Grams |
| Material | Measure Portion | A | B | C | D | E | F |
| Almonds | 12-15 nuts | 12.90 | 3.20 | .051 | .037 | .072 | .00060 |
| Apples, dried | ½ cup, 1.2 oz. | 2.50 | .60 | 0.100 | .108 | .163 | .00050 |
| Apples, fresh | 1 large apple, 7.5 oz. | 2.40 | 0.60 | .096 | .012 | .020 | .00050 |
| Apricots, dried | 9 halves, 1.3 oz. | 7.60 | 1.90 | 0.300 | .123 | .044 | .00050 |
| Asparagus, fresh | 20 stalks, 8 in. long, 15.9 oz. | 32.40 | 8.10 | 1.290 | .122 | .177 | .00450 |
| Bacon, fried | 4-5 small slices, 5 oz. | 6.80 | 1.70 | .270 | .001 | .018 | .00030 |
| Bananas | 1 large, 5.5 oz. | 5.30 | 1.30 | .020 | .009 | .031 | .00060 |
| Beans, Lima, dried | 2 tbs., 1 oz. | 23.20 | 5.80 | .920 | .020 | .096 | .00200 |
| Beans, Lima, fresh | ½ cup, 2.9 oz. | 23.00 | 5.70 | .920 | .001 | .007 | .00011 |
| Beans, string | 2½ cups, cut in pieces, 8.5 oz. | 22.40 | 5.60 | .890 | .110 | .126 | .00270 |
| Beans, white, dried | 2 tbs., 1 oz. | 26.00 | 6.50 | 1.400 | .047 | .137 | .00200 |
| Beets | 4 beets, 2 in. diam., 7 oz. | 14.00 | 3.50 | 0.560 | .064 | .084 | .00130 |
| Beef, round, lean | 1 slice, 3 × 3 × 1½ in., 2 oz. | 48.00 | 12.00 | 1.920 | .007 | .129 | .00180 |
| Beef feet | slice, 5 × 2½ × ¼ in., 1.6 oz. | 30.00 | 7.50 | 1.600 | .004 | .081 | .00110 |
| Butter | 1 (scant) tbs., 0.5 oz. | 1.60 | 0.40 | .064 | .002 | .002 | .00003 |
| [Pg 479]Cabbage | 5 cups, sliced, 11.2 oz. | 20.40 | 5.10 | 0.890 | .143 | .092 | .00350 |
| Carrots | 4-5 young car., 10.5 oz. | 9.60 | 2.40 | 0.384 | .124 | .101 | .00130 |
| Cauliflower | 1 small head, 11.5 oz. | 23.60 | 5.90 | 0.944 | .403 | .200 | .00200 |
| Celery | 4 cups, in 1-in. pieces | 5.20 | 1.30 | 0.200 | .421 | .201 | .00270 |
| Clams | 6 clams, ½ cup, 7.6 oz. | 79.20 | 19.80 | 3.160 | .285 | .282 | .00970 |
| Cheese, American | 1⅛ in. cube (0.8 oz.) | 24.40 | 6.10 | 0.970 | .211 | .156 | .00030 |
| Cherries (stoned) | 1 cup, 4.5 oz. | 4.80 | 1.20 | 0.190 | .025 | .039 | .00050 |
| Chicken, lean meat, roasted | 2½ oz. | 79.60 | 19.90 | 3.190 | .006 | .075 | .00290 |
| Crackers, soda | 4 crackers | 9.60 | 2.40 | 0.380 | .006 | .025 | .00040 |
| Cornmeal | 3 tbs., 1 oz. | 10.40 | 2.60 | 0.410 | .005 | .053 | .00030 |
| Corn | ⅓ cup, 3.6 oz. | 12.40 | 3.10 | 0.490 | .006 | .102 | .00080 |
| Chocolate, unsweetened | ¾ × ¼ × ⅞ in. piece | 8.40 | 2.10 | 0.330 | .015 | .075 | .00040 |
| Cocoa | 3½ tbs., 0.7 oz. | 17.60 | 4.40 | 0.490 | .023 | .143 | .00050 |
| Cream, 18% (thin) | ¼ cup, 1.8 oz. | 5.20 | 1.30 | 9.200 | .050 | .044 | .00010 |
| Cream, 40% (thick) | 1⅓ tbs., 0.9 oz. | 2.40 | 0.60 | 0.096 | .020 | .020 | .00005 |
| Dates | 4½ dates, 1.1 oz. | 2.40 | 0.60 | 0.096 | .019 | .016 | .00090 |
| Eggs | 1⅓ eggs | 36.40 | 9.10 | 1.450 | .045 | .122 | .00210 |
| Egg whites | 7 whites, 6.9 oz. | 96.48 | 24.12 | 3.850 | .020 | .022 | .00020 |
| Egg yolks | 2 yolks, 1 oz. | 17.28 | 4.32 | .691 | .036 | .118 | .00230 |
| [Pg 480]Farina | 3 tbs., 1 oz. | 12.40 | 3.10 | .496 | .006 | .035 | .00020 |
| Fish, lean | piece, 3 × 3 × ½ in., 2.4 oz. | 90.40 | 22.60 | 3.610 | .025 | .259 | .00120 |
| Fish, oily | 53.20 | 13.30 | 2.120 | .015 | .153 | .00070 | |
| Figs | 1½ large figs, 1.1 oz. | 5.60 | 1.40 | .224 | .051 | .037 | .00100 |
| Flour, entire wheat | 3 tbs., 1 oz. | 15.60 | 3.90 | .624 | .009 | .066 | .00070 |
| graham | 3 tbs., 1 oz. | 14.80 | 3.70 | .592 | .011 | .101 | .00100 |
| rye | 3 tbs., 1 oz. | 8.00 | 2.00 | .320 | .005 | .082 | .00040 |
| white | 4 tbs., 1 oz. | 12.80 | 3.20 | .572 | .006 | .026 | .00020 |
| Gelatin | 27 grams | 98.80 | 24.90 | 3.980 | |||
| Grapefruit | 2¾ tbs. | 5.00 | 1.25 | .040 | .036 | .00058 | |
| Grapes (Concord) | 1 large bunch, 5 oz. | 5.60 | 1.40 | 0.200 | .019 | .032 | .00030 |
| Grape juice | ½ cup, 3.6 oz. | 1.40 | 0.35 | .050 | .011 | .011 | .00030 |
| Hominy | 3½ tbs., 1 oz. | 9.60 | 2.40 | 0.350 | .002 | .027 | .00030 |
| Honey | 1 tbs., 1.1 oz. | .40 | 0.10 | .002 | .006 | .00030 | |
| Lamb | 1 slice, 3½ × 4½ × ⅓ in., 1.8 oz. | 25.60 | 6.40 | 1.020 | .004 | .069 | .00100 |
| Lemons | 3 large, 11.4 oz. | 9.20 | 2.30 | 0.360 | .081 | .049 | .00140 |
| [Pg 481]Lettuce | 2 large heads, 18.5 oz. | 25.20 | 6.30 | 1.000 | .224 | .224 | .00790 |
| Lentils (dried) | 2½ tbs., 1 oz. | 29.60 | 7.40 | 1.180 | .031 | 1.260 | .00250 |
| Macaroni | 1 cup | 14.80 | 3.70 | 0.590 | .006 | .040 | .00030 |
| Milk, whole | ⅜ cup, 5.1 oz. | 19.20 | 4.80 | 0.760 | .174 | .134 | .00090 |
| skimmed | ⅜ cup | 37.20 | 9.30 | 1.480 | .331 | .262 | .00070 |
| unsweetened, canned | 3¾ tbs., 2.1 oz. | 23.20 | 5.80 | 0.920 | .188 | .146 | .00040 |
| sweet, canned | 1½ tbs., 1.1 oz. | 10.40 | 2.60 | 0.410 | .096 | .072 | .00020 |
| buttermilk | 1⅛ cup, 10.0 oz. | 33.60 | 8.40 | 1.340 | .294 | .271 | .00070 |
| Milk powder[172] | 1 oz. | ||||||
| malted (Horlick’s)[173] | 1½ tbs., 1.2 oz. | ||||||
| Molasses | |||||||
| Mutton | 1 slice, 3 × 3¼ × ⅛ inch | 24.80 | 6.20 | 0.990 | .004 | .067 | .00090 |
| Oatmeal | ⅓ cup, 1 oz. | 16.80 | 4.20 | 0.670 | .017 | .099 | .00100 |
| Onions | 3-4 med., 7.2 oz. | 13.20 | 3.30 | 0.520 | .069 | .093 | .00100 |
| Orange | 1 large, 9.5 oz. | 6.40 | 1.60 | 0.250 | .088 | .040 | .00040 |
| Oysters (raw) | 6-12 oys., ⅔ cup, 7.2 oz. | 49.20 | 12.30 | 1.060 | .106 | .306 | .00890 |
| Parsnip | 2 medium, 7.0 oz. | 10.00 | 2.50 | 0.400 | .091 | .117 | .00090 |
| Peas, fresh | ¾ cup, 3.5 oz. | 26.00 | 6.50 | 1.040 | .026 | .120 | .00170 |
| Peaches, fresh | 3 medium, 60.5 oz. | 3.80 | 1.70 | 0.270 | .038 | .057 | .00070 |
| [Pg 482]Pears | 1 large, 6.3 oz. | 4.00 | 1.00 | 0.160 | .024 | .041 | .00050 |
| Peanuts | 20-24 single, 0.6 oz. | 18.80 | 4.70 | 0.750 | .013 | .073 | .00049 |
| Pecans | 12 single, 0.51 oz. | 5.20 | 1.30 | 0.200 | .012 | .045 | .00040 |
| Pepper (green) | 18.00 | 4.50 | 0.720 | .034 | .145 | .00220 | |
| Pineapple | 2 slices 1 in. thick, 8.2 oz. | 3.60 | 0.90 | .041 | .064 | .00120 | |
| Plums | 3-4 large, 4.4 oz. | 4.80 | 1.20 | 0.190 | .024 | .038 | .00060 |
| Potatoes (sweet) | ½ medium, 3.6 oz. | 6.00 | 1.50 | 0.240 | .016 | .037 | .00040 |
| Potatoes (white) | 1 medium, 5.3 oz. | 10.80 | 2.70 | 0.430 | .016 | .069 | .00160 |
| Prunes | 4 medium, 1.4 oz. | 2.80 | 0.70 | .110 | .018 | .035 | .00100 |
| Radishes | 36 small, 12 oz. | 17.60 | 4.40 | 0.700 | .073 | .098 | .00210 |
| Rhubarb | 4 cups, cut in small pieces, 15.3 oz. | 10.40 | 2.60 | 0.410 | .189 | .134 | .00430 |
| Rice | 3 tbs., 1 oz. | 9.20 | 2.30 | 0.360 | .004 | .027 | .00030 |
| Shredded wheat | 1 biscuit, 0.9 oz. | 14.00 | 3.50 | 0.550 | .011 | .089 | .00120 |
| Spinach | 3 cups, 14.7 oz. | 35.20 | 8.80 | 1.400 | .281 | .285 | .01500 |
| Squash, summer | 12.40 | 3.10 | 0.490 | .039 | .035 | .00130 | |
| winter | 12.40 | 3.10 | .038 | .069 | .00130 | ||
| Strawberries | 1⅓ cups, 9.0 oz. | 10.24 | 2.56 | 0.400 | .104 | .072 | .00210 |
| [Pg 483]Tapioca | 3 tbs., 1.0 oz. | 0.44 | 0.11 | 0.017 | .004 | .025 | .00050 |
| Tomatoes, fresh | 2-3 medium, 15.5 oz. | 16.00 | 4.00 | 0.640 | .050 | .113 | .00180 |
| canned | 1¾ cup, 15.6 oz. | ||||||
| Turnips | 2 cups, cut in cubes, 13.0 oz. | 13.20 | 3.30 | 0.520 | .161 | .117 | .00130 |
| Veal | slice, 2 × 2¾ inches, 2.3 oz. | 58.00 | 14.50 | 2.320 | .008 | .156 | .00220 |
| Walnuts, English | 16-18 nuts, 0.5 oz. | 10.40 | 2.60 | 0.410 | .013 | .015 | .00030 |
| Watermelon (edible portion) | 11.7 oz. | 5.20 | 1.30 | 0.200 | .038 | .010 | .00100 |
[171] Table compiled from “Chemistry of Food and Nutrition,” Sherman.—“A Laboratory Handbook for Dietetics,” and “Feeding the Family,” Rose—and other sources.
[172] Milk powders now on market are made from skimmed or partially skimmed milk.
[173] Horlick’s malted milk. Analysis made in Horlick’s Laboratories.
All determinations allow 28.35 grams to the ounce.
All calculations are made using the factor 4 calories for protein, 4 calories for carbohydrates, and 9 calories for fats.
The materials are measured in standard 8-ounce measuring cups, or tablespoons. The measures are exactly level unless otherwise stated. In calculating beverages containing alcohol, it is necessary to know the percentage of alcohol contained therein. Alcohol has a fuel value of 7 calories per gram. (Whether this heat is available for the needs of the body is still a question.)
| Key: | |
| A | Nitrogen Gm. |
| B1 | Proteins Per Cent |
| B2 | Proteins Gm. |
| C1 | Fats Per cent |
| C2 | Fats Gm. |
| D1 | Carbohydrates Per Cent |
| D2 | Carbohydrates Gm. |
| E | Fuel Value |
| Material | Weight | Measure | A | B1 | B2 | C1 | C2 | D1 | D2 | E |
| Almonds | ½ oz. | 6 | .48 | 21.0 | 2.970 | 54.90 | 7.780 | 17.3 | 2.450 | 92.00 |
| Apples | 5.5 oz. | 1 medium | .09 | 0.4 | .600 | 0.50 | .780 | 14.2 | 22.000 | 97.40 |
| Apricots | 9 halves | — | 5.1 | 1.900 | 0.10 | .400 | 61.0 | 22.500 | 100.00 | |
| Arrowroot | 1 oz. | 8 tablespoonfuls | — | — | — | — | — | 69.2 | 19.600 | 78.00 |
| Artichoke, French | 1 oz. | .15 | 3.4 | .960 | 0.50 | .140 | 12.0 | 3.400 | 18.70 | |
| Asparagus, fresh | 4 oz. | 6 stalks | .33 | 1.8 | 2.040 | 0.20 | .230 | 3.3 | 3.740 | 25.00 |
| Asparagus, canned | 4 oz. | ½ cup | .28 | 1.5 | 1.700 | 0.10 | .110 | 2.8 | 3.170 | 21.00 |
| Bacon | 1 oz. | 2 slices | .35 | 9.0 | 2.500 | 58.00 | 16.000 | — | — | 144.00 |
| Bananas, E.P.[174] | 3½ oz. | 1 medium | .20 | 1.3 | 1.290 | 0.60 | .600 | 22.0 | 21.830 | 98.00 |
| Barley, pearled | 1 oz. | 3 tablespoonfuls | .39 | 8.5 | 2.410 | 1.10 | .310 | 77.0 | 22.000 | 100.00 |
| Barley flour | ½ oz. | 1 tablespoonful | .16 | 10.4 | .980 | 2.20 | .210 | 72.6 | 7.000 | 33.00 |
| Bass | 3 oz. | 1 serving | 2.53 | 18.6 | 15.800 | 2.80 | 2.370 | — | — | 84.00 |
| Beans, string | 3 oz. | 1 serving | .31 | 2.3 | 1.950 | .26 | .220 | 5.1 | 4.350 | 27.00 |
| Beans, butter | 3 oz. | 1 serving | 1.26 | 9.3 | 7.900 | 0.60 | .510 | 29.2 | 24.800 | 135.00 |
| Beans, Lima, dried | 1 oz. | .81 | 18.0 | 5.100 | 1.50 | .420 | 65.9 | 18.700 | 99.00 | |
| Beans, baked, canned | 1 oz. | .31 | 6.9 | 1.960 | 2.50 | .710 | 19.6 | 5.500 | 36.00 | |
| Beef broth | 1 oz. | 2 tablespoonfuls | 0.10 | 1.8 | .500 | 0.10 | .300 | — | — | 4.70 |
| Beef broth | 6 oz. | 1 cup | 0.30 | 1.8 | 3.000 | 0.10 | 1.800 | — | — | 28.00 |
| Beef soup[175] | 6 oz. | 1 cup | 1.18 | 4.3 | 7.400 | 3.60 | 6.100 | 1.1 | 1.800 | 92.00 |
| Beef juice | 1 oz. | 2 tablespoonfuls | .22 | 4.9 | 1.390 | .60 | .170 | — | — | 6.00 |
| Beef marrow | ½ oz. | 1 tablespoonful | .05 | 2.2 | .310 | 92.00 | 13.000 | — | — | 118.00 |
| Beefsteak, porterhouse | 3 oz. | 1 serving | 2.99 | 22.0 | 18.690 | 20.40 | 17.350 | — | — | 240.00 |
| Beefsteak, sirloin | 3 oz. | 1 serving | 2.57 | 19.0 | 16.080 | 18.50 | 15.720 | — | — | 205.80 |
| Top of round | 3 oz. | 1 serving | 2.65 | 19.5 | 16.580 | 7.30 | 6.210 | — | — | 106.20 |
| Roast beef, second cut | 2 oz. | 1 slice | 1.84 | 20.2 | 11.500 | 8.40 | 4.800 | — | — | 89.00 |
| Roast beef, second cut | 1 oz. | 1 thin slice | .91 | 20.1 | 5.700 | 8.50 | 2.400 | — | — | 44.00 |
| Beets, cooked | 1 oz. | .10 | 2.3 | .650 | .10 | .030 | 7.4 | 2.100 | 11.30 | |
| Bluefish | 3 oz. | 1 serving | 2.65 | 19.6 | 16.600 | 1.20 | 1.000 | — | — | 75.00 |
| Brandy | ½ oz. | 1 tablespoonful | — | — | — | — | — | — | — | 42.00 |
| Bran | 2½ oz. | 1 cup | 1.25 | 11.0 | 7.800 | 2.10 | 1.500 | 61.0 | 43.000 | 217.00 |
| Bread | 1 oz. | 1 slice, ¾ in. thick | .42 | 9.2 | 2.600 | 1.30 | .370 | 53.0 | 15.000 | 73.70 |
| Boston brown | 1 oz. | 1 slice | .27 | 6.0 | 1.700 | 6.30 | 1.790 | 54.0 | 15.300 | 84.10 |
| Rolls | 1 oz. | .41 | 9.0 | 2.550 | 3.00 | .850 | 54.2 | 15.400 | 79.50 | |
| Whole wheat | 1 oz. | .44 | 9.7 | 2.750 | .90 | .260 | 49.7 | 14.100 | 69.70 | |
| [Pg 486 & 487]Bread crumbs | 5 oz. | 1 cup | 2.08 | 9.3 | 13.000 | 1.20 | 1.700 | 53.0 | 75.000 | 367.00 |
| Bread, graham | 1 oz. | 1 slice | .40 | 8.8 | 2.500 | 1.80 | .510 | 52.0 | 14.700 | 73.50 |
| Bread, gluten[176] | 1 oz. | 1 slice, ½ in. thick | 1.34 | 29.5 | 8.400 | 1.10 | .300 | 30.0 | 8.500 | 70.00 |
| Maryland biscuit (Southern beaten biscuit) | 1 oz. | 2 small biscuits | .38 | 8.4 | 2.380 | 5.60 | 1.500 | 60.0 | 17.000 | 91.70 |
| Butter | 1 oz. | 2 tablespoonfuls | .04 | 1.0 | .280 | 85.00 | 24.090 | — | — | 218.00 |
| Butter | 1 lb. | 2 cups | .72 | 1.0 | 4.530 | 85.00 | 385.500 | — | — | 3488.00 |
| Cabbage | 1 oz. | .07 | 1.6 | .450 | 00.30 | .090 | 5.6 | 1.590 | 9.00 | |
| Carrots | 3 oz. | 1 medium | .15 | 1.1 | .930 | 00.40 | .340 | 9.3 | 7.910 | 37.50 |
| Carrots | 1 oz. | .05 | 1.1 | .310 | 00.40 | .110 | 9.3 | 2.630 | 12.50 | |
| Cauliflower | 3 oz. | 1 serving | .24 | 1.8 | 1.530 | 00.50 | .420 | 4.7 | 3.990 | 25.80 |
| Cauliflower | 1 oz. | .08 | 1.8 | .510 | 00.50 | .140 | 4.7 | 1.330 | 8.60 | |
| Celery | 1 oz. | 1 stalk, medium sized | .05 | 1.1 | .310 | 00.10 | .030 | 3.3 | .930 | 5.20 |
| Chard | 1 oz. | .15 | 3.2 | .910 | 00.60 | .170 | 5.0 | 1.410 | 10.80 | |
| Cherries, fresh | 1 oz. | .04 | 1.0 | .280 | 00.80 | .230 | 16.7 | 4.730 | 22.00 | |
| Chestnuts | 1 oz. | .28 | 6.2 | 1.760 | 5.40 | 1.530 | 42.1 | 11.940 | 68.60 | |
| Clam bouillon | 1 oz. | 2 tablespoonfuls | .01 | 0.2 | .057 | — | — | 0.2 | .057 | .45 |
| Clam bouillon | 6 oz. | ⅔ cup | .01 | 0.2 | .342 | — | — | 0.2 | .342 | 3.00 |
| Cheese, American | 1 oz. | 2 tablespoonfuls, grated | 1.31 | 28.8 | 8.160 | 35.90 | 10.180 | 0.3 | .090 | 124.60 |
| Cottage cheese (curds) | 1 oz. | 2 tablespoonfuls | .95 | 20.9 | 5.920 | 1.00 | .280 | 4.3 | 1.220 | 31.00 |
| Cream cheese (Neufchâtel) | 1 oz. | ½ block | .85 | 18.7 | 5.240 | 27.40 | 7.770 | 1.5 | .420 | 93.00 |
| Chicken, broiler, E.P. | 1 oz. | .97 | 20.7 | 5.800 | 8.30 | 2.350 | — | — | 44.35 | |
| Chicken, broiler, E.P. | 3 oz. | 1 serving | 2.92 | 20.7 | 17.400 | 8.30 | 7.050 | — | — | 133.00 |
| Chocolate, unsweetened | 1 oz. | 1 square | .58 | 12.9 | 3.650 | 48.70 | 13.800 | 30.3 | 8.590 | 173.00 |
| Cocoa | 1 oz. | 4 tablespoonfuls | .98 | 21.6 | 6.120 | 28.90 | 8.190 | 37.7 | 10.690 | 141.00 |
| Cocoa | ⅛ oz. | 2 teaspoonfuls (1 serving) | .12 | 21.6 | .760 | 28.90 | 1.020 | 37.7 | 1.330 | 17.60 |
| Cod, dressed | 1 oz. | .50 | 11.0 | 3.120 | 0.20 | .060 | — | — | 13.00 | |
| Condensed milk, sweetened (Eagle Brand) | 1 oz. | 2 tablespoonfuls | .40 | 8.8 | 2.490 | 8.30 | 2.350 | 53.9 | 15.300 | 92.00 |
| Condensed milk, or evaporated, unsweetened | ⅛ oz. | 1 teaspoonful | .07 | 7.5 | .270 | 8.30 | .290 | 9.7 | .340 | 5.00 |
| Consommé | 6 oz. | ⅔ cup | 1.06 | 2.5 | 4.250 | — | — | 0.4 | .680 | 19.70 |
| Corn, canned | 1 oz. | 2 tablespoonfuls | .13 | 2.8 | .790 | 1.20 | .340 | 19.0 | 5.390 | 28.00 |
| Corn, green, E.P. | 1 oz. | 2 tablespoonfuls | .14 | 3.1 | .880 | 1.10 | .310 | 19.7 | 5.580 | 28.60 |
| Cornmeal, granular | 1 oz. | 2 tablespoonfuls | .42 | 9.3 | 2.630 | 1.90 | .540 | 75.5 | 21.400 | 101.00 |
| Cornflakes, toasted | 1 oz. | .25 | 5.5 | 1.560 | 1.50 | .430 | 81.2 | 23.000 | 102.10 | |
| Cornstarch | 1 oz. | 3 tablespoonfuls | — | — | — | — | — | 89.1 | 25.250 | 101.00 |
| Crackers, graham | ⅓ oz. | 1 cracker | .15 | 10.0 | .940 | 9.30 | .880 | 73.8 | 6.970 | 39.50 |
| Crackers, water | ⅓ oz. | 1 cracker | .19 | 11.7 | .770 | 5.00 | .470 | 75.7 | 7.000 | 35.30 |
| Crackers, oyster | 1 oz. | .51 | 11.3 | 3.200 | 10.50 | 2.980 | 70.5 | 19.980 | 119.50 | |
| Cracker crumbs | 2½ oz. | ½ cup | 1.32 | 11.6 | 7.800 | 6.00 | 4.300 | 72.9 | 51.700 | 276.70 |
| [Pg 488 & 489]Cranberries | 1 oz. | 2 tablespoonfuls | .02 | 0.4 | .110 | 0.60 | .170 | 10.0 | 2.800 | 13.00 |
| Cream, 18% (single X) | 1 oz. | 2 tablespoonfuls | .13 | 3.0 | .800 | 19.70 | 5.600 | 4.9 | 1.400 | 59.00 |
| Cream, 40% (double X) | 1 oz. | 2 tablespoonfuls | .10 | 2.2 | .620 | 40.00 | 11.340 | 3.0 | .850 | 108.00 |
| Cucumber, E.P. | 1 oz. | .04 | 0.8 | .230 | 0.20 | .060 | 3.1 | .880 | 5.00 | |
| Currants, dried | 1 oz. | 2 tablespoonfuls | .11 | 2.4 | .680 | 1.70 | .480 | 74.2 | 21.040 | 91.00 |
| Dates, dried | 1.1 oz. | 4½ | .09 | 2.0 | .570 | 2.80 | .790 | 78.4 | 22.200 | 7.50 |
| Dry peptonoids | 1 oz. | 2 tablespoonfuls | .96 | 21.1 | 6.000 | — | — | 28.2 | 8.000 | 56.00 |
| Eggs, whole, without shell | 1.8 oz. | or | ||||||||
| 5 gms. | 1 medium sized | 1.00 | 13.4 | 6.800 | 10.50 | 5.360 | — | — | 75.00 | |
| Egg white | 1.2 oz. | 1 white (34 gm. wt.) | .67 | 12.3 | 4.180 | .20 | 0.070 | — | — | 17.00 |
| Egg yolk | .6 oz. | 1 yolk (17 gm. wt.) | .43 | 15.7 | 2.670 | 31.00 | 5.270 | — | — | 58.00 |
| Eggplant | 1 oz. | .05 | 1.2 | .340 | .30 | .090 | 5.1 | 1.450 | 8.00 | |
| Farina | 1 oz. | 3 tablespoonfuls | .50 | 11.0 | 3.110 | 1.40 | .390 | 76.4 | 21.650 | 103.00 |
| Figs, dried | 1 oz. | 1 fig | .19 | 4.3 | 1.210 | 0.30 | .090 | 74.1 | 21.000 | 89.60 |
| Fish | 1 oz. | .84 | 18.0 | 5.240 | 1.40 | .400 | — | — | 24.60 | |
| Flour, barley | 1 oz. | 2 tablespoonfuls | .46 | 10.2 | 2.900 | 2.20 | .620 | 72.7 | 20.600 | 99.70 |
| Flour, gum gluten | 1 oz. | 3 tablespoonfuls | 1.65 | 36.3 | 10.300 | 1.30 | .360 | 36.9 | 10.440 | 86.20 |
| Flour, graham | 1 oz. | 3 tablespoonfuls | .60 | 13.3 | 3.770 | 2.20 | .620 | 71.4 | 20.240 | 101.60 |
| Flour, wheat | 1 oz. | 3 tablespoonfuls | .51 | 11.2 | 3.180 | 1.00 | .280 | 75.2 | 21.310 | 100.50 |
| Flour, wheat | ⅓ oz. | 1 tablespoonful | .17 | 11.2 | 1.060 | 1.00 | .090 | 75.2 | 7.100 | 33.50 |
| Flour, entire wheat | 1 oz. | 3 tablespoonfuls | .63 | 13.8 | 3.910 | 1.90 | .530 | 71.9 | 20.380 | 102.00 |
| Fowl, E.P. | 1 oz. | .88 | 19.3 | 5.470 | 16.30 | 4.650 | — | — | 63.50 | |
| Fowl, E.P. | 3½ oz. | 1 serving | 3.09 | 19.3 | 19.000 | 16.30 | 16.300 | — | — | 222.00 |
| Gelatin, granulated | 1 oz. | 4.15 | 91.4 | 25.910 | 0.10 | .028 | — | — | 103.80 | |
| Gelatin, granulated | ¼ oz. | 1 tablespoonful | 1.04 | 91.4 | 6.470 | 0.10 | .007 | — | — | 25.90 |
| Gum gluten bread | 1 oz. | 1 slice | 1.34 | 29.7 | 8.400 | 1.10 | .300 | 30.0 | 8.500 | 70.30 |
| Gum gluten biscuit | ¼ oz. | 1 biscuit | .47 | 41.9 | 2.900 | 1.80 | .1300 | 44.4 | 3.150 | 25.40 |
| Greens (A.P.), beet tops | 4 oz. | .38 | 2.1 | 2.400 | 3.30 | 3.700 | 3.2 | 3.600 | 57.00 | |
| Greens, cooked | 4 oz. | 1 serving | .37 | 2.0 | 2.300 | 0.30 | .300 | 3.2 | 3.600 | 26.30 |
| Grapes, malaga | 2 oz. | about 12 grapes | .12 | 1.3 | .740 | 1.60 | .900 | 19.2 | 10.880 | 54.50 |
| Grapes, malaga | 1 lb. | .95 | 1.3 | 5.900 | 1.60 | 7.200 | 19.2 | 87.040 | 436.00 | |
| Grapefruit | 1 oz. | — | .6 | .170 | .10 | .030 | 12.2 | 3.460 | 14.80 | |
| Grape juice | 1 oz. | 2 tablespoonfuls | — | — | — | — | — | 25.0 | 7.090 | 28.30 |
| Grape juice | 4 oz. | ½ cupful | — | — | — | — | — | 25.0 | 28.360 | 113.40 |
| Halibut (E.P.) steak | 3 oz. | 1 serving | 2.53 | 18.6 | 15.810 | 5.20 | 4.420 | — | — | 103.00 |
| Ham, lean, smoked, E.P. | 1½ oz. | 1 serving (1 slice) | 1.35 | 19.8 | 8.410 | 21.00 | 8.930 | — | — | 114.00 |
| Ham, medium fat, smoked | 1 oz. | 1 slice | .74 | 16.3 | 4.620 | 38.80 | 11.000 | — | — | 117.50 |
| Hominy | 1 oz. | 2 tablespoonfuls | .38 | 8.3 | 2.350 | 0.60 | .170 | 79.0 | 22.390 | 100.50 |
| Hickory nuts, shelled | 1 oz. | 2 tablespoonfuls | .70 | 15.4 | 4.360 | 67.10 | 19.000 | 11.4 | 3.230 | 201.30 |
| Honey | 1 oz. | 2 tablespoonfuls | .02 | 0.4 | .110 | — | — | 81.3 | 23.040 | 92.60 |
| [Pg 490 & 491] | ||||||||||
| Jell-O | 3.5 oz. | 1 box | 1.79 | 11.2 | 11.000 | — | — | 86.4 | 86.000 | 388.00 |
| Jell-O | .6 oz. | 1 serving | .30 | 11.2 | 1.900 | — | — | 86.4 | 14.700 | 66.00 |
| Kohl-rabi | 1 oz. | .09 | 2.0 | .560 | .10 | .030 | 5.5 | 1.560 | 8.80 | |
| Koumiss | 1 litre | 1000 c.c. | 4.01 | 2.8 | 25.400 | 2.10 | 19.500 | 5.4 | 48.900 | 473.00 |
| Koumiss | 4 oz. | ½ glassful | .51 | 2.8 | 3.170 | 2.10 | 2.380 | 5.4 | 6.120 | 58.50 |
| Lactose (sugar of milk) 100% carbohydrates | 1 oz. | 2 tablespoonfuls | — | — | — | — | — | 100.0 | 28.350 | 113.40 |
| Lady fingers | ½ oz. | 3 lady fingers | .20 | 8.7 | 1.230 | 5.00 | .700 | 70.5 | 10.000 | 51.20 |
| Lamb chops, broiled | 3 oz. | 2 chops, medium size | 2.95 | 21.8 | 18.540 | 30.00 | 25.510 | — | — | 303.70 |
| Lamb, leg, roasted | 1 oz. | 1 serving (small) | — | 19.7 | 5.580 | 12.70 | 3.600 | — | — | 54.70 |
| Lard | 1 oz. | 2 tablespoonfuls | — | — | — | 100.00 | 28.350 | — | — | 255.10 |
| Lemon juice (1 lemon) | 1½ oz. | 3 tablespoonfuls | — | — | — | — | — | 9.7 | 4.120 | 16.40 |
| Lemon juice | 1 oz. | 2 tablespoonfuls | — | — | — | — | — | 9.8 | 2.770 | 11.00 |
| Lettuce | 8 oz. | 1 head | .44 | 1.2 | 2.720 | 0.30 | .680 | 2.9 | 4.520 | 35.00 |
| Lettuce | 2 oz. | 1 serving (¼ head) | .11 | 1.2 | .680 | 0.30 | .170 | 2.0 | 1.130 | 8.77 |
| Liver | 1 oz. | — | 20.4 | 5.780 | 4.50 | 1.280 | 1.7 | .480 | 36.50 | |
| Liquid peptonoids | 1 oz. | 2 tablespoonfuls | .26 | 5.6 | 1.600 | — | — | 14.8 | 4.200 | 23.00 |
| Lentils | 1 oz. | 2 tablespoonfuls | 1.17 | 25.7 | 7.290 | 1.00 | .280 | 59.2 | 16.780 | 98.80 |
| Lobster | 2 oz. | 1 serving | 1.75 | 18.1 | 10.260 | 1.10 | .620 | 0.5 | .280 | 48.00 |
| Macaroni | 4 oz. | ½ cupful | 2.43 | 13.4 | 15.200 | 0.90 | 1.000 | 74.1 | 84.000 | 406.00 |
| Mackerel, fresh, E.P. | 3 oz. | 1 serving | 2.54 | 18.7 | 15.900 | 7.10 | 6.030 | — | — | 117.80 |
| Mackerel, salt dressed, E.P. | 2 oz. | 1 serving (small) | 1.57 | 17.3 | 9.800 | 26.30 | 14.850 | — | — | 173.00 |
| Malted milk (Horlick’s) | ½ oz. | 1 tablespoonful | .37 | 16.2 | 2.300 | 8.50 | 1.200 | 67.0 | 9.500 | 58.00 |
| Milk (whole) | 1 oz. | 2 tablespoonfuls | .15 | 3.3 | .940 | 4.00 | 1.130 | 5.0 | 1.410 | 19.60 |
| Milk (whole) | 8 oz. | 1 glassful | 1.20 | 3.3 | 7.520 | 4.00 | 9.040 | 5.0 | 11.280 | 156.80 |
| Milk (skimmed) | 1 oz. | 2 tablespoonfuls | .15 | 3.4 | .960 | 0.30 | .090 | 5.1 | 1.450 | 10.40 |
| Milk, dried (whole) | 1 oz. | 2 tablespoonfuls | 1.10 | 24.3 | 6.890 | 28.50 | 8.080 | 36.8 | 10.430 | 142.00 |
| Milk, dried (skim) | 1 oz. | 2 tablespoonfuls | 1.50 | 33.9 | 9.600 | 1.00 | .280 | 55.0 | 15.600 | 103.30 |
| Molasses, cane | 1 oz. | 2 tablespoonfuls | .11 | 2.4 | .680 | — | — | 69.3 | 19.650 | 81.30 |
| Mushrooms | 1 oz. | — | 3.5 | .990 | .40 | .110 | 6.8 | 1.930 | 12.70 | |
| Muskmelons | 8 oz. | ½ small melon | .22 | 0.6 | 1.360 | — | — | 9.3 | 21.000 | 89.44 |
| Noodles (gluten) | 2 oz. | ¾ cupful | 2.05 | 45.0 | 25.500 | 4.10 | 2.300 | 32.5 | 18.400 | 196.40 |
| Oatmeal | ½ oz. | 1 tablespoonful | .38 | 16.1 | 2.300 | 7.20 | 1.000 | 67.5 | 9.500 | 56.40 |
| Oatmeal gruel | 4 oz. | ½ cupful | .21 | 1.1 | 1.300 | 0.40 | .450 | 0.6 | 7.300 | 38.40 |
| Oats, rolled | 1 oz. | .76 | 16.7 | 4.730 | 7.30 | 2.070 | 66.2 | 18.770 | 112.60 | |
| Okra | 1 oz. | .07 | 1.6 | .450 | .20 | .060 | 7.4 | 2.100 | 10.74 | |
| Olives | ½ oz. | 3 medium sized | .02 | 1.1 | .150 | 27.60 | 3.910 | 11.6 | 1.640 | 42.40 |
| Olive oil | 1 oz. | 2 tablespoonfuls | — | — | — | 100.00 | 28.350 | — | — | 255.10 |
| [Pg 492 & 493]Onion | 2 oz. | 1 medium sized | .07 | 1.6 | .900 | 0.30 | .170 | 9.9 | 5.600 | 27.50 |
| Orange | 5 oz. | 1 medium sized | .17 | 0.6 | .850 | 0.10 | .140 | 8.5 | 12.050 | 53.00 |
| Orange (juice) | 1 oz. | 2 tablespoonfuls | — | — | — | — | — | 11.3 | 3.200 | 12.80 |
| Oysters | 1 oz. | 3 small | .28 | 6.2 | 1.750 | 1.20 | .340 | 3.7 | 1.040 | 14.20 |
| Panopepton | 1 oz. | 2 tablespoonfuls | .32 | 7.1 | 2.000 | — | — | 17.3 | 5.000 | 28.00 |
| Parsnips | 1 oz. | 1 medium size | — | 0.1 | .030 | .50 | .140 | 13.5 | 3.830 | 16.70 |
| Peaches, E.P. (fresh) | 3 oz. | 1 medium size | .10 | 0.7 | .600 | 0.10 | .090 | 9.4 | 7.990 | 35.10 |
| Peaches, canned | 3 oz. | 1 serving | .10 | 0.7 | .600 | 0.10 | .090 | 10.8 | 9.180 | 39.90 |
| Peanut butter | 1 oz. | 2 tablespoonfuls | 1.33 | 29.3 | 8.310 | 46.60 | 13.200 | 17.1 | 4.850 | 151.40 |
| Peanuts, shelled | 2½ oz. | ½ cupful | 3.32 | 29.3 | 20.770 | 46.50 | 33.000 | 5.8 | 4.120 | 396.50 |
| Pears, fresh | 3 oz. | 1 medium size | .08 | 0.6 | .510 | 0.50 | .420 | 14.1 | 12.000 | 53.80 |
| Pears, canned | 3 oz. | 1 serving | .04 | 0.3 | .260 | 0.30 | .260 | 18.1 | 12.400 | 53.00 |
| Peas, green, fresh, E.P. | 3 oz. | 1 serving, about ½ cup | .95 | 7.0 | 5.950 | .50 | .420 | 16.9 | 14.370 | 85.00 |
| Peas, canned | 4 oz. | ½ cup | .65 | 3.6 | 4.080 | 0.20 | .230 | 9.8 | 11.110 | 62.80 |
| Peas (dried, split peas) | 1 oz. | 3 tablespoonfuls | 1.12 | 24.6 | 6.970 | 1.00 | .280 | 62.0 | 17.570 | 100.70 |
| Peppers, green | 1 oz. | .05 | 1.1 | .310 | 0.10 | .030 | 4.6 | 1.300 | 6.71 | |
| Pineapple (canned) | 3 oz. | 1 thick slice | .07 | 0.5 | .400 | 0.70 | .600 | 36.4 | 31.000 | 131.00 |
| Pineapple (fresh, E.P.) | 3 oz. | 1 serving | .05 | 0.4 | .340 | 0.30 | .260 | 9.7 | 8.250 | 36.70 |
| Pecans, shelled | 2½ oz. | ½ cup | .58 | 9.6 | 6.800 | 70.50 | 50.000 | 15.0 | 10.600 | 519.60 |
| Plums | 1 oz. | .04 | 1.0 | .280 | — | — | 20.1 | 5.700 | 23.90 | |
| Port wine (10% alcohol) | ½ oz. | 1 tablespoonful | — | — | — | — | — | — | — | 10.00 |
| Potatoes, white, raw | 3 oz. | 1 medium size | .30 | 2.2 | 1.870 | 0.10 | .090 | 18.4 | 15.650 | 70.90 |
| Potatoes, sweet, raw | 4 oz. | 1 medium size | .30 | 1.8 | 2.040 | 0.70 | .790 | 27.4 | 31.070 | 139.60 |
| Prunes, A.P. | 1 oz. | 3 prunes | .08 | 1.8 | .510 | — | — | 62.2 | 17.630 | 72.60 |
| Prunes, E.P. | 4 oz. | 1 cupful | .38 | 2.1 | 2.380 | — | — | 73.3 | 83.120 | 342.00 |
| Quail | 3½ oz. | ½ quail, 1 serving | 1.00 | 21.0 | 20.300 | 8.00 | 7.900 | — | — | 152.30 |
| Raisins | 1 oz. | 3 dozen | .12 | 2.6 | .740 | 3.30 | .940 | 76.1 | 21.570 | 97.70 |
| Raspberries, black, fresh | 1 oz. | 3 tablespoonfuls | .08 | 1.7 | .480 | 1.00 | .280 | 12.6 | 3.570 | 18.70 |
| Raspberry juice, fresh | 4 oz. | ½ cup | — | — | — | — | — | 10.0 | 11.300 | 45.20 |
| Rhubarb, fresh, E.P. | 1 oz. | .03 | 0.6 | .170 | 0.70 | .200 | 3.6 | 1.020 | 6.60 | |
| Rice | 1 oz. | 2 tablespoonfuls, 1 serving | .36 | 7.9 | 2.260 | 0.30 | .090 | 79.0 | 22.390 | 99.35 |
| Rum | 1 oz. | 2 tablespoonfuls | — | — | — | — | — | — | — | 76.00 |
| Salmon, canned | 1 oz. | .99 | 22.0 | 6.240 | 12.80 | 3.630 | — | — | 57.60 | |
| Salmon, canned | 1 lb. | 1 can | 15.82 | 22.0 | 99.800 | 12.80 | 57.600 | — | — | 922.00 |
| Saltines (crackers) | 1 oz. | .48 | 10.6 | 3.000 | 12.70 | 3.600 | 68.5 | 19.420 | 123.00 | |
| Saltines (crackers) | 1 lb. | 1 box | 7.68 | 10.6 | 48.000 | 12.70 | 57.600 | 68.5 | 310.700 | 1968.00 |
| Sardines, canned | 1 oz. | 1 small serving | 1.08 | 23.0 | 6.720 | 19.70 | 5.580 | — | — | 77.00 |
| [Pg 494 & 495]Shad | 3 oz. | 1 serving | 1.96 | 18.8 | 11.000 | 9.50 | 8.070 | — | — | 116.60 |
| Shad roe | 1 oz. | 1 small serving | .95 | 20.9 | 5.920 | 3.80 | 1.080 | 2.6 | .730 | 36.30 |
| Sherry wine | 1 oz. | 2 tablespoonfuls | — | — | — | — | — | — | — | 28.00 |
| Spinach | 4 oz. | ½ cup | .38 | 2.1 | 2.380 | .30 | .340 | 3.2 | 3.630 | 27.00 |
| Squab | 2½ oz. | ½ squab | 1.86 | 16.3 | 11.500 | 36.20 | 25.650 | — | — | 277.00 |
| Squash | 3 oz. | 1 serving | .10 | 0.7 | .600 | 0.20 | .170 | 4.5 | 3.830 | 18.30 |
| Strawberries | 3 oz. | 1 serving, about ½ cup | .13 | 1.0 | .850 | 0.60 | .510 | 7.4 | 6.290 | 33.00 |
| Strawberry juice | 4 oz. | ½ cup | — | — | — | — | — | 4.8 | 5.400 | 22.00 |
| Suet | 1 oz. | 2 tablespoonfuls | .21 | 4.7 | 1.330 | 82.00 | 23.190 | — | — | 215.00 |
| Sugar (granulated) | 1 oz. | 2 tablespoonfuls | — | — | — | — | — | 100.0 | 28.350 | 113.40 |
| Sugar (loaf) | ½ oz. | 1 lump | — | — | — | — | — | 100.0 | 7.100 | 28.40 |
| Sugar (powdered) | ⅓ oz. | 1 tablespoonful | — | — | — | — | — | 100.0 | 9.450 | 37.80 |
| Sweetbreads | 3½ oz. | 1 serving | 2.28 | 16.7 | 16.450 | 12.10 | 12.000 | — | — | 173.80 |
| Sweetbreads | 8 oz. | 1 set | 6.08 | 16.7 | 38.000 | 12.10 | 27.400 | — | — | 398.60 |
| Tapioca | 1 oz. | 2 tablespoonfuls | .02 | 0.4 | .110 | 0.10 | .030 | 88.0 | 24.950 | 100.50 |
| Tapioca (minute) | 1 oz. | 2 tablespoonfuls | .02 | 0.4 | .110 | 0.10 | .030 | 88.0 | 24.950 | 100.50 |
| Toast | 1 oz. | 1 thick slice | .52 | 11.5 | 3.260 | 1.60 | .450 | 61.2 | 17.350 | 86.50 |
| Tomatoes (fresh) | 5 oz. | 1 whole tomato | .07 | 0.9 | 1.270 | 0.40 | .570 | 3.9 | 5.500 | 32.00 |
| Tomatoes (canned) | 1 oz. | 2 tablespoonfuls | .05 | 1.2 | .340 | 0.20 | .060 | 4.0 | 1.130 | 6.40 |
| Trout | 3 oz. | 1 serving | 2.46 | 18.0 | 15.300 | 10.30 | 8.760 | — | — | 140.00 |
| Trout | 1 oz. | .82 | 18.0 | 5.100 | 10.30 | 2.920 | — | — | 46.70 | |
| Turnips (fresh) | 3 oz. | 1 serving | .18 | 1.3 | 1.110 | 0.20 | .170 | 8.1 | 6.900 | 33.60 |
| Turkey | 2½ oz. | 1 serving (2 slices) | 2.39 | 21.1 | 14.940 | 22.90 | 16.220 | — | — | 206.00 |
| Turkey | 1 oz. | .96 | 21.1 | 5.980 | 22.90 | 6.490 | — | — | 82.40 | |
| Veal cutlet | 1 oz. | — | 20.3 | 5.750 | 7.70 | 2.180 | — | — | 42.60 | |
| Walnuts | 1 oz. | .84 | 18.4 | 5.220 | 64.40 | 18.260 | 13.0 | 3.790 | 200.00 | |
| Walnuts | 5½ oz. | 1 cupful | 4.59 | 18.4 | 28.710 | 64.40 | 100.430 | 13.0 | 20.840 | 1100.00 |
| Watermelon, E.P. | 1 oz. | .02 | .4 | .110 | .20 | .060 | 6.7 | 1.900 | 8.58 | |
| Wheat (shredded) | 1 oz. | 1 biscuit | .55 | 10.5 | 2.980 | 1.40 | .400 | 78.0 | 22.000 | 103.50 |
| Wheat flakes | 1 oz. | 1 cupful (about) | .61 | 13.4 | 3.800 | 1.40 | .390 | 74.3 | 21.060 | 103.00 |
| Whey | 6 oz. | 1 cup (scant) | .27 | 1.0 | 1.700 | 0.30 | .510 | 5.0 | 8.500 | 45.40 |
| Whitefish, E.P. | 1 oz. | ⅓ serving | 1.04 | 22.9 | 6.500 | 6.50 | 1.840 | — | — | 42.56 |
| Zwieback | 1 oz. | 3 small slices | .44 | 9.8 | 2.770 | 1.00 | 2.800 | 73.5 | 20.830 | 119.60 |
[174] Edible portion.
[175] Beef soup is not so thoroughly strained or so well skimmed as broth.
[176] Gum gluten has a smaller percentage of starch than ordinary gluten flour.
| Foodstuff | “A” | “B” | “C” |
| Meats: | |||
| Beef heart | + | + | ? |
| Brains | + + | + + + | + ? |
| Codfish | + | + | ? |
| Cod testes | + | ||
| Fish roe | + | + + | ? |
| Herring | + + | + + | ? |
| Horse meat | + | + | |
| Kidney | + + | + + | |
| Lean muscle | 0 | 0 | + ? |
| Liver | + | + | + ? |
| Pancreas | 0 | + + + | |
| Pig heart | + | + | ? |
| Placenta | + | ||
| Thymus (sweetbreads) | 0 | 0 | 0 |
| Vegetables: | |||
| Beetroot | + | + | + + |
| Beet root juice | ? | Little | + + + |
| Cabbage, dried | + + + | + + + | + |
| Cabbage, fresh | + + + | + + + | + + + + |
| Carrots | + + + | + + + | + + |
| Cauliflower | + + | + + + | + + |
| Celery | ? | + + + | ? |
| Chard | + + + | + + | ? |
| Dasheens | + | + + | ? |
| Lettuce | + + | + + | + + + + |
| Mangels | + + | + + | ? |
| Onions | ? | + + + | + + + |
| Parsnips | + + | + + + | |
| Peas (fresh) | + | + + | + + + |
| Potatoes | 0 | + + + | + + |
| Potatoes (sweet) | + + + | + + | ? |
| Rutabaga | + + + | ||
| Spinach | + + + | + + + | + + + |
| Cereals: | |||
| Barley | + | + + + | ? |
| Bread (white) | + ? | ||
| Bread (whole meal) | + | + + + | ? |
| Maize | + In yellow | + + + | ? |
| 0 In white | |||
| Oats | + | + + + | 0 |
| Rice (polished) | 0 | 0 | 0 |
| Rice (whole grain) | + | + + + | 0 |
| [Pg 497]Rye | + | + + + | 0 |
| Corn embryo | + + + | ||
| Corn (kaffir) | + + + | ||
| Corn (see maize) | |||
| Corn pollen | + + | ||
| Malt extract | 0 | 0 | 0 |
| Wheat bran | 0 | + | 0 |
| Wheat embryo | + + | + + + | 0 |
| Wheat endosperm | 0 | 0 | 0 |
| Wheat kernel | + | + + + | 0 |
| Other seeds: | |||
| Beans, kidney | + + + | ||
| Beans, navy | + + + | 0 | |
| Beans, soy | + | + + + | 0 |
| Cotton seed | + + | + + + | |
| Flaxseed | + + | + + + | |
| Hemp seed | + + | + + + | |
| Millet seed | + + | + + + | |
| Peanuts | + | + + | |
| Peas (dry) | + ? | + + | 0 |
| Sunflower seeds | + | ||
| Fruits: | |||
| Apples | + + | + + | |
| Bananas | ? | + | + + |
| Grapefruit | + + + | + + + | |
| Grape juice | + | + | |
| Grapes | 0 | + | + |
| Lemons | + + + | + + + + | |
| Limes | + + | + + | |
| Oranges | + + + | + + + + | |
| Pears | + + | + + | |
| Raisins | + | + | |
| Tomatoes | + + | + + + | + + + + |
| Oils and fats: | |||
| Almond oil | 0 | 0 | |
| Beef fat | + | 0 | 0 |
| Butter | + + + + | 0 | 0 |
| Cocoanut oil | 0 | 0 | 0 |
| Cod liver oil | + + + + | 0 | 0 |
| Corn oil | 0 | 0 | 0 |
| Cotton seed oil | 0 ? | 0 | 0 |
| Egg yolk fat | + + + + | 0 | 0 |
| Fish oils | + + | 0 | 0 |
| Lard | 0 ? | 0 | 0 |
| Oleo, animal | + | 0 | 0 |
| [Pg 498]Oleo, vegetable | 0 | 0 | 0 |
| Olive oil | 0 | 0 | 0 |
| Pork fat | 0 ? | 0 | |
| Tallow | 0 | 0 | 0 |
| Vegetable oils | 0 ? | 0 | 0 |
| Nuts: | |||
| Almonds | + | + + + | |
| Brazil nut | + + + | ||
| Chestnut | + + + | ||
| Cocoanut | + + | + + + | |
| English walnuts | + + + | ||
| Filbert | + + + | ||
| Hickory | + | + | + |
| Pine | + | + | + |
| Dairy products: | |||
| Butter | + + + + | 0 | 0 |
| Cheese | + + | + | ? |
| Condensed milk | + + | + | 0 |
| Cream | + + + | + | ? |
| Eggs | + + + + | + + | 0 |
| Milk powder (skim) | + | + + + | + ? |
| Milk powder (whole) | + + + | + + + | + ? |
| Milk whole | + + + | + + + | + + |
| Whey | + | + + + | + |
| Miscellaneous: | |||
| Alfalfa | + + + | + + + | ? |
| Blood | Varies with source | ||
| Clover | + + + | + + + + | ? |
| Honey | + + | 0 | |
| Malt extract | 0 | 0 | 0 |
| Nectar | 0 | 0 | 0 |
| Timothy | + + | + + + | |
| Yeast, brewers’ | 0 | + + + + | 0 |
| Yeast cakes | 0 | + + | 0 |
| Yeast extract | 0 | + + + | 0 |
Table V taken from “The Vitamine Manual,” by Walter S. Eddy, published by Williams & Wilkins Co., Baltimore, Md.
[177] Courtesy of Dr. Walter S. Eddy.
(Based on Data Published by the Children’s Bureau, U. S. Department of Labor)
| Age | BOYS | GIRLS | ||
| Height | Weight | Height | Weight | |
| Inches | Pounds | Inches | Pounds | |
| Birth | 20.6 | 7.6 | 20.5 | 7.2 |
| 3 mo. | 23.5 | 13.0 | — | — |
| 6 mo. | 26.5 | 18.0 | 25.9 | 16.8 |
| 9 mo. | 28.1 | 20.4 | 26.6 | 19.1 |
| 12 mo. | 29.4 | 21.9 | 28.9 | 20.8 |
| 15 mo. | 30.8 | 23.6 | 30.1 | 21.9 |
| 18 mo. | 31.8 | 24.6 | 31.1 | 23.4 |
| 21 mo. | 32.9 | 25.8 | 32.3 | 24.8 |
| 24 mo. | 33.8 | 27.1 | 33.4 | 26.4 |
| 27 mo. | 34.8 | 29.0 | 33.9 | 27.3 |
| 30 mo. | 35.4 | 29.5 | 34.9 | 28.3 |
| 33 mo. | 36.1 | 30.6 | 35.6 | 29.1 |
| 36 mo. | 37.1 | 32.3 | 36.8 | 30.5 |
| 39 mo. | 37.9 | 33.1 | 37.3 | 31.6 |
| 42 mo. | 38.6 | 33.8 | 38.0 | 32.5 |
| 45 mo. | 39.0 | 34.5 | 38.5 | 33.3 |
| 48 mo. | 39.5 | 35.9 | 39.0 | 33.8 |
| 5 years | 41.6 | 41.4 | 41.3 | 39.7 |
| Height Inches | 5 Yrs. | 6 Yrs. | 7 Yrs. | 8 Yrs. | 9 Yrs. | 10 Yrs. | 11 Yrs. | 12 Yrs. | 13 Yrs. | 14 Yrs. | 15 Yrs. | 16 Yrs. | 17 Yrs. | 18 Yrs. |
| 39 | 35 | 36 | 37 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 40 | 37 | 38 | 39 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 41 | 39 | 40 | 41 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 42 | 41 | 42 | 43 | 44 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 43 | 43 | 44 | 45 | 46 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 44 | 45 | 46 | 46 | 47 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 45 | 47 | 47 | 48 | 48 | 49 | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 46 | 48 | 49 | 50 | 50 | 51 | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 47 | ... | 51 | 52 | 52 | 53 | 54 | ... | ... | ... | ... | ... | ... | ... | ... |
| 48 | ... | 53 | 54 | 55 | 55 | 56 | 57 | ... | ... | ... | ... | ... | ... | ... |
| 49 | ... | 55 | 56 | 57 | 58 | 58 | 59 | ... | ... | ... | ... | ... | ... | ... |
| 50 | ... | ... | 58 | 59 | 60 | 60 | 61 | 62 | ... | ... | ... | ... | ... | ... |
| 51 | ... | ... | 60 | 61 | 62 | 63 | 64 | 65 | ... | ... | ... | ... | ... | ... |
| 52 | ... | ... | 62 | 63 | 64 | 65 | 67 | 68 | ... | ... | ... | ... | ... | ... |
| 53 | ... | ... | ... | 66 | 67 | 68 | 69 | 70 | 71 | ... | ... | ... | ... | ... |
| 54 | ... | ... | ... | 69 | 70 | 71 | 72 | 73 | 74 | ... | ... | ... | ... | ... |
| 55 | ... | ... | ... | ... | 73 | 74 | 75 | 76 | 77 | 78 | ... | ... | ... | ... |
| 56 | ... | ... | ... | ... | 77 | 78 | 79 | 80 | 81 | 82 | ... | ... | ... | ... |
| 57 | ... | ... | ... | ... | ... | 81 | 82 | 83 | 84 | 85 | 86 | ... | ... | ... |
| 58 | ... | ... | ... | ... | ... | 84 | 85 | 86 | 87 | 88 | 90 | 91 | ... | ... |
| 59 | ... | ... | ... | ... | ... | 87 | 88 | 89 | 90 | 92 | 94 | 96 | 97 | ... |
| 60 | ... | ... | ... | ... | ... | 91 | 92 | 93 | 94 | 97 | 99 | 101 | 102 | ... |
| 61 | ... | ... | ... | ... | ... | ... | 95 | 97 | 99 | 102 | 104 | 106 | 108 | 110 |
| 62 | ... | ... | ... | ... | ... | ... | 100 | 102 | 104 | 106 | 109 | 111 | 113 | 116 |
| 63 | ... | ... | ... | ... | ... | ... | 105 | 107 | 109 | 111 | 114 | 115 | 117 | 119 |
| 64 | ... | ... | ... | ... | ... | ... | ... | 113 | 115 | 117 | 118 | 119 | 120 | 122 |
| 65 | ... | ... | ... | ... | ... | ... | ... | ... | 120 | 122 | 123 | 124 | 125 | 126 |
| 66 | ... | ... | ... | ... | ... | ... | ... | ... | 125 | 126 | 127 | 128 | 129 | 130 |
| 67 | ... | ... | ... | ... | ... | ... | ... | ... | 130 | 130 | 132 | 133 | 134 | 135 |
| 68 | ... | ... | ... | ... | ... | ... | ... | ... | 134 | 135 | 136 | 137 | 138 | 139 |
| 69 | ... | ... | ... | ... | ... | ... | ... | ... | 138 | 139 | 140 | 141 | 142 | 143 |
| 70 | ... | ... | ... | ... | ... | ... | ... | ... | ... | 142 | 144 | 145 | 146 | 147 |
| 71 | ... | ... | ... | ... | ... | ... | ... | ... | ... | 147 | 149 | 150 | 151 | 152 |
| 72 | ... | ... | ... | ... | ... | ... | ... | ... | ... | 152 | 154 | 155 | 156 | 157 |
| 73 | ... | ... | ... | ... | ... | ... | ... | ... | ... | 157 | 159 | 160 | 161 | 162 |
| 74 | ... | ... | ... | ... | ... | ... | ... | ... | ... | 162 | 164 | 165 | 166 | 167 |
| 75 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | 169 | 170 | 171 | 172 |
| 76 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | 174 | 175 | 176 | 177 |
Prepared by Dr. Thomas D. Wood
| Age | |
| 5 to 8 | 6 oz. |
| 8 to 12 | 8 oz. |
| 12 to 16 | 16 oz. |
| 16 to 18 | 8 oz. |
Weight and measures should be taken without shoes, and in only the usual indoor clothes.
Courtesy of Child Health Organization of America
| Height Inches | 5 Yrs. | 6 Yrs. | 7 Yrs. | 8 Yrs. | 9 Yrs. | 10 Yrs. | 11 Yrs. | 12 Yrs. | 13 Yrs. | 14 Yrs. | 15 Yrs. | 16 Yrs. | 17 Yrs. | 18 Yrs. |
| 39 | 34 | 35 | 36 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 40 | 36 | 37 | 38 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 41 | 38 | 39 | 40 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 42 | 40 | 41 | 42 | 43 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 43 | 42 | 42 | 43 | 44 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 44 | 44 | 45 | 45 | 46 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 45 | 46 | 47 | 47 | 48 | 49 | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 46 | 48 | 48 | 49 | 50 | 51 | ... | ... | ... | ... | ... | ... | ... | ... | ... |
| 47 | ... | 49 | 50 | 51 | 52 | 53 | ... | ... | ... | ... | ... | ... | ... | ... |
| 48 | ... | 51 | 52 | 53 | 54 | 55 | 56 | ... | ... | ... | ... | ... | ... | ... |
| 49 | ... | 53 | 54 | 55 | 56 | 57 | 58 | ... | ... | ... | ... | ... | ... | ... |
| 50 | ... | ... | 56 | 57 | 58 | 59 | 60 | 61 | ... | ... | ... | ... | ... | ... |
| 51 | ... | ... | 59 | 60 | 61 | 62 | 63 | 64 | ... | ... | ... | ... | ... | ... |
| 52 | ... | ... | 62 | 63 | 64 | 65 | 66 | 67 | ... | ... | ... | ... | ... | ... |
| 53 | ... | ... | ... | 66 | 67 | 68 | 68 | 69 | 70 | ... | ... | ... | ... | ... |
| 54 | ... | ... | ... | 68 | 69 | 70 | 71 | 72 | 73 | ... | ... | ... | ... | ... |
| 55 | ... | ... | ... | ... | 72 | 73 | 74 | 75 | 76 | 77 | ... | ... | ... | ... |
| 56 | ... | ... | ... | ... | 76 | 77 | 78 | 79 | 80 | 81 | ... | ... | ... | ... |
| 57 | ... | ... | ... | ... | ... | 81 | 82 | 83 | 84 | 85 | 86 | ... | ... | ... |
| 58 | ... | ... | ... | ... | ... | 85 | 86 | 87 | 88 | 89 | 90 | 91 | ... | ... |
| 59 | ... | ... | ... | ... | ... | 89 | 90 | 91 | 93 | 94 | 95 | 96 | 98 | ... |
| 60 | ... | ... | ... | ... | ... | ... | 94 | 95 | 97 | 99 | 100 | 102 | 104 | 106 |
| 61 | ... | ... | ... | ... | ... | ... | 99 | 101 | 102 | 104 | 106 | 108 | 109 | 111 |
| 62 | ... | ... | ... | ... | ... | ... | 104 | 106 | 107 | 109 | 111 | 113 | 114 | 115 |
| 63 | ... | ... | ... | ... | ... | ... | 109 | 111 | 112 | 113 | 115 | 117 | 118 | 119 |
| 64 | ... | ... | ... | ... | ... | ... | ... | 115 | 117 | 118 | 119 | 120 | 121 | 122 |
| 65 | ... | ... | ... | ... | ... | ... | ... | 117 | 119 | 120 | 122 | 123 | 124 | 125 |
| 66 | ... | ... | ... | ... | ... | ... | ... | 119 | 121 | 122 | 124 | 126 | 127 | 128 |
| 67 | ... | ... | ... | ... | ... | ... | ... | ... | 124 | 126 | 127 | 128 | 129 | 130 |
| 68 | ... | ... | ... | ... | ... | ... | ... | ... | 126 | 128 | 130 | 132 | 133 | 134 |
| 69 | ... | ... | ... | ... | ... | ... | ... | ... | 129 | 131 | 133 | 135 | 136 | 137 |
| 70 | ... | ... | ... | ... | ... | ... | ... | ... | ... | 134 | 136 | 138 | 139 | 140 |
| 71 | ... | ... | ... | ... | ... | ... | ... | ... | ... | 138 | 140 | 142 | 143 | 144 |
| 72 | ... | ... | ... | ... | ... | ... | ... | ... | ... | ... | 145 | 147 | 148 | 149 |
Prepared by Dr. Thomas D. Wood
| Age | |
| 5 to 8 | 6 oz. |
| 8 to 11 | 8 oz. |
| 11 to 14 | 12 oz. |
| 14 to 16 | 8 oz. |
| 16 to 18 | 4 oz. |
Courtesy of Child Health Organization of America
Pelidisi Chart (For School Children)
| Sitting Height | Percentage (Pelidisi) | |||||||||||
| in Cm. | 85 | 86 | 87 | 88 | 89 | 90 | 91 | 92 | 93 | 94 | 95 | 96 |
| 55 | 10.0 | 10.4 | 10.7 | 11.1 | 11.5 | 11.9 | 12.3 | 12.7 | 13.1 | 13.6 | 14.0 | 14.4 |
| 56 | 10.6 | 10.9 | 11.4 | 11.7 | 12.2 | 12.6 | 13.0 | 13.4 | 13.9 | 14.3 | 14.8 | 15.3 |
| 57 | 11.1 | 11.5 | 11.9 | 12.4 | 12.8 | 13.2 | 13.7 | 14.2 | 13.6 | 15.1 | 15.6 | 16.1 |
| 58 | 11.7 | 12.1 | 12.6 | 13.0 | 13.5 | 13.9 | 14.4 | 14.9 | 15.4 | 15.9 | 16.4 | 16.9 |
| 59 | 12.4 | 12.8 | 13.2 | 13.7 | 14.2 | 14.7 | 15.2 | 15.7 | 16.2 | 16.7 | 17.3 | 17.8 |
| 60 | 13.0 | 13.4 | 13.9 | 14.4 | 14.9 | 15.4 | 15.9 | 16.5 | 17.1 | 17.6 | 18.2 | 18.8 |
| 61 | 13.7 | 14.1 | 14.6 | 15.2 | 15.7 | 16.2 | 16.8 | 17.3 | 17.9 | 18.5 | 19.1 | 19.7 |
| 62 | 14.3 | 14.8 | 15.4 | 15.9 | 16.5 | 17.1 | 17.6 | 18.2 | 18.8 | 19.4 | 20.0 | 20.7 |
| 63 | 15.0 | 15.6 | 16.1 | 16.7 | 17.3 | 17.9 | 18.5 | 19.1 | 19.7 | 20.4 | 21.0 | 21.7 |
| 64 | 15.8 | 16.3 | 16.9 | 17.5 | 18.1 | 18.8 | 19.4 | 20.0 | 20.7 | 21.4 | 22.1 | 22.8 |
| 65 | 16.5 | 17.1 | 17.7 | 18.3 | 19.0 | 19.7 | 20.3 | 21.0 | 21.7 | 22.4 | 23.1 | 23.9 |
| 66 | 17.3 | 17.9 | 18.5 | 19.2 | 19.9 | 20.6 | 21.2 | 21.9 | 22.7 | 23.4 | 24.2 | 25.0 |
| 67 | 18.7 | 18.7 | 19.4 | 20.1 | 20.8 | 21.5 | 22.2 | 23.0 | 23.7 | 24.5 | 25.3 | 26.1 |
| 68 | 18.9 | 19.6 | 20.3 | 21.0 | 21.7 | 22.5 | 23.2 | 24.0 | 24.8 | 25.6 | 26.4 | 27.3 |
| 69 | 19.8 | 20.5 | 21.2 | 22.0 | 22.7 | 23.5 | 24.2 | 25.0 | 25.9 | 26.7 | 27.6 | 28.5 |
| 70 | 20.6 | 21.4 | 22.1 | 22.9 | 23.7 | 24.5 | 25.3 | 26.2 | 27.0 | 27.9 | 28.8 | 29.8 |
| 71 | 21.5 | 22.3 | 23.1 | 23.9 | 24.7 | 25.6 | 26.4 | 27.3 | 28.2 | 29.1 | 30.1 | 31.3 |
| 72 | 22.4 | 23.2 | 24.1 | 25.0 | 25.8 | 26.6 | 27.6 | 28.5 | 29.4 | 30.4 | 31.4 | 32.4 |
| 73 | 23.4 | 24.3 | 25.1 | 26.0 | 26.9 | 27.8 | 28.8 | 29.8 | 30.7 | 31.7 | 32.8 | 33.8 |
| 74 | 24.4 | 25.3 | 26.2 | 27.1 | 28.0 | 29.0 | 30.0 | 31.0 | 32.0 | 33.0 | 34.0 | 35.2 |
| 75 | 25.4 | 26.3 | 27.2 | 28.2 | 29.2 | 30.2 | 31.2 | 32.3 | 33.2 | 34.3 | 35.5 | 36.6 |
| 76 | 26.4 | 27.4 | 28.4 | 29.4 | 30.3 | 31.3 | 32.7 | 33.5 | 34.6 | 35.7 | 36.9 | 38.2 |
| 77 | 27.5 | 28.4 | 29.5 | 30.6 | 31.6 | 32.6 | 33.8 | 34.8 | 36.0 | 37.2 | 38.4 | 39.6 |
| 78 | 28.6 | 29.6 | 30.7 | 31.8 | 32.8 | 33.9 | 35.0 | 36.2 | 37.4 | 38.6 | 40.0 | 41.1 |
| 79 | 29.7 | 30.8 | 31.8 | 33.0 | 34.0 | 35.2 | 36.4 | 37.7 | 38.8 | 40.1 | 41.5 | 42.8 |
| 80 | 30.8 | 31.9 | 33.1 | 34.2 | 35.4 | 36.6 | 37.9 | 39.0 | 40.4 | 41.7 | 43.0 | 44.5 |
| 81 | 32.0 | 33.2 | 34.3 | 35.5 | 36.7 | 38.0 | 39.3 | 40.5 | 41.9 | 43.3 | 44.7 | 46.1 |
| 82 | 33.2 | 34.4 | 35.6 | 36.8 | 38.1 | 39.4 | 40.8 | 42.0 | 43.5 | 45.0 | 46.4 | 47.9 |
| 83 | 34.4 | 35.7 | 36.9 | 38.2 | 39.6 | 40.8 | 42.3 | 43.7 | 45.1 | 46.6 | 48.0 | 49.6 |
| 84 | 35.7 | 37.0 | 38.2 | 39.6 | 41.0 | 42.3 | 43.8 | 45.3 | 46.8 | 48.3 | 49.9 | 51.5 |
| 85 | 37.0 | 38.2 | 39.6 | 41.0 | 42.4 | 43.9 | 46.4 | 46.9 | 48.5 | 50.0 | 51.6 | 53.4 |
| 86 | 38.3 | 39.6 | 41.0 | 42.5 | 44.0 | 45.5 | 47.0 | 48.7 | 50.2 | 51.9 | 53.7 | 55.4 |
| 87 | 39.6 | 41.0 | 42.5 | 44.0 | 45.5 | 47.1 | 48.7 | 50.3 | 52.0 | 53.8 | 55.5 | 57.2 |
| 88 | 41.0 | 42.5 | 44.0 | 45.5 | 47.2 | 48.7 | 50.4 | 52.0 | 58.8 | 55.5 | 57.5 | 59.3 |
| 89 | 42.5 | 44.0 | 45.5 | 47.1 | 48.8 | 50.5 | 52.2 | 53.9 | 55.7 | 57.5 | 59.6 | 61.2 |
| 90 | 44.0 | 45.4 | 47.0 | 48.7 | 50.4 | 52.2 | 54.0 | 55.8 | 57.5 | 59.5 | 61.5 | 63.4 |
| Sitting Height | Percentage (Pelidisi) | |||||||||||
| in Cm. | 97 | 98 | 99 | 100 | 101 | 102 | 103 | 104 | 105 | 106 | 107 | 108 |
| 55 | 14.9 | 15.4 | 15.8 | 16.4 | 16.9 | 17.4 | 17.9 | 18.4 | 19.0 | 19.6 | 20.1 | 20.7 |
| 56 | 15.7 | 16.2 | 16.8 | 17.3 | 17.9 | 18.4 | 18.9 | 19.5 | 20.1 | 20.6 | 21.2 | 21.8 |
| 57 | 16.6 | 17.1 | 17.7 | 18.2 | 18.8 | 19.4 | 20.0 | 20.6 | 21.2 | 21.8 | 22.4 | 23.0 |
| 58 | 17.5 | 18.0 | 18.6 | 19.2 | 19.8 | 20.4 | 21.0 | 21.6 | 22.3 | 22.9 | 23.6 | 24.2 |
| 59 | 18.4 | 19.0 | 19.6 | 20.2 | 20.9 | 21.5 | 22.2 | 22.8 | 23.5 | 24.1 | 24.8 | 25.6 |
| 60 | 19.3 | 20.0 | 20.6 | 21.2 | 22.0 | 22.6 | 23.3 | 24.0 | 24.6 | 25.4 | 26.1 | 26.8 |
| 61 | 20.3 | 21.0 | 21.7 | 22.4 | 23.1 | 23.7 | 24.4 | 25.2 | 25.9 | 26.6 | 27.4 | 28.2 |
| 62 | 21.4 | 22.1 | 22.8 | 23.4 | 24.2 | 24.9 | 25.7 | 26.4 | 27.2 | 28.0 | 28.8 | 29.6 |
| 63 | 22.4 | 23.2 | 23.8 | 24.6 | 25.4 | 26.2 | 27.0 | 27.8 | 28.6 | 29.4 | 30.2 | 31.1 |
| 64 | 23.5 | 24.3 | 25.0 | 25.8 | 26.8 | 27.4 | 28.2 | 29.1 | 30.0 | 30.8 | 31.6 | 32.6 |
| 65 | 24.6 | 25.5 | 26.2 | 27.0 | 27.9 | 28.8 | 29.6 | 30.5 | 31.4 | 32.2 | 33.2 | 34.2 |
| 66 | 25.7 | 26.6 | 27.4 | 28.2 | 29.2 | 30.0 | 31.0 | 31.9 | 32.8 | 33.8 | 34.8 | 35.8 |
| 67 | 26.9 | 27.8 | 28.6 | 29.5 | 30.6 | 31.4 | 32.4 | 33.4 | 34.3 | 35.4 | 36.3 | 37.4 |
| 68 | 28.2 | 29.1 | 30.0 | 30.9 | 32.0 | 32.9 | 33.8 | 34.9 | 35.9 | 36.9 | 38.0 | 39.1 |
| 69 | 29.7 | 30.4 | 31.3 | 32.3 | 33.4 | 34.4 | 35.4 | 36.4 | 37.5 | 38.6 | 39.7 | 40.9 |
| 70 | 30.7 | 31.6 | 32.7 | 33.8 | 34.8 | 35.8 | 37.0 | 38.1 | 39.1 | 40.3 | 41.5 | 42.6 |
| 71 | 32.1 | 33.1 | 34.1 | 35.2 | 36.4 | 37.4 | 38.6 | 39.7 | 40.9 | 42.0 | 43.2 | 44.5 |
| 72 | 33.5 | 34.5 | 35.6 | 36.7 | 38.0 | 39.0 | 40.3 | 41.5 | 42.6 | 43.9 | 45.1 | 46.8 |
| 73 | 34.9 | 36.0 | 37.0 | 38.2 | 39.5 | 40.7 | 42.0 | 43.2 | 44.5 | 45.7 | 47.1 | 48.4 |
| 74 | 36.3 | 37.4 | 38.6 | 39.8 | 41.1 | 42.4 | 43.7 | 45.0 | 46.4 | 47.6 | 49.0 | 50.4 |
| 75 | 37.8 | 39.0 | 40.1 | 41.4 | 42.8 | 44.1 | 45.4 | 46.9 | 48.3 | 49.5 | 50.9 | 52.5 |
| 76 | 39.3 | 40.5 | 41.7 | 43.1 | 44.5 | 45.9 | 47.3 | 48.7 | 50.3 | 51.5 | 53.0 | 54.5 |
| 77 | 40.9 | 42.7 | 43.5 | 44.8 | 46.4 | 47.7 | 49.2 | 50.7 | 52.3 | 53.6 | 55.2 | 56.8 |
| 78 | 42.5 | 43.9 | 45.2 | 46.6 | 48.2 | 49.6 | 51.0 | 52.6 | 54.3 | 55.7 | 57.3 | 58.9 |
| 79 | 44.1 | 45.5 | 46.9 | 48.4 | 50.0 | 51.5 | 53.1 | 54.7 | 56.5 | 58.0 | 59.6 | 61.3 |
| 80 | 45.9 | 47.3 | 48.7 | 50.2 | 52.0 | 53.6 | 55.1 | 56.9 | 58.6 | 60.1 | 61.8 | 63.7 |
| 81 | 47.6 | 49.1 | 50.6 | 52.1 | 54.0 | 55.5 | 57.3 | 59.0 | 60.8 | 62.5 | 64.3 | 66.0 |
| 82 | 49.9 | 51.0 | 52.5 | 54.1 | 56.0 | 57.6 | 59.5 | 61.3 | 63.0 | 67.9 | 66.7 | 68.5 |
| 83 | 51.2 | 52.9 | 54.5 | 56.1 | 58.1 | 59.7 | 61.7 | 63.5 | 65.3 | 67.2 | 69.1 | 71.0 |
| 84 | 53.0 | 54.8 | 56.5 | 58.2 | 60.2 | 62.0 | 64.0 | 65.8 | 67.7 | 69.7 | 71.6 | 73.6 |
| 85 | 55.0 | 56.8 | 58.5 | 60.4 | 62.4 | 64.3 | 66.3 | 68.2 | 70.0 | 72.1 | 74.2 | 76.3 |
| 86 | 57.1 | 58.9 | 60.7 | 62.6 | 64.6 | 66.5 | 68.5 | 70.5 | 72.7 | 74.8 | 76.9 | 79.0 |
| 87 | 59.1 | 60.9 | 62.9 | 64.7 | 66.9 | 69.0 | 71.0 | 73.0 | 75.2 | 77.5 | 79.6 | 81.8 |
| 88 | 61.2 | 63.0 | 65.0 | 67.0 | 69.3 | 71.4 | 73.5 | 75.5 | 77.8 | 80.0 | 82.4 | 84.7 |
| 89 | 63.3 | 65.3 | 67.3 | 69.4 | 71.6 | 73.6 | 76.0 | 78.1 | 80.5 | 82.9 | 85.2 | 87.5 |
| 90 | 65.4 | 67.5 | 69.5 | 71.5 | 74.0 | 76.4 | 78.6 | 80.9 | 83.4 | 85.7 | 88.1 | 90.5 |
Instructions for use: To determine the “pelidisi,” locate in the left-hand column the child’s sitting height in centimeters. With a ruler follow the weights in kilograms to the right until the proper figure is reached. Trace upward in that column to the heavy figure at the top, which indicates the pelidisi.
[178] This material was published in the American Medical Journal, Vol. 77, No. 20, Nov. 12, 1921, by Dr. William E. Carter, Dept. Pediatrics, University of California Medical School, San Francisco, Calif.
Pirquet believes that the sitting height is a basis for the more accurate estimation of the nutritional state than is the standing height. It was demonstrated that the cube of the sitting height in centimeters is approximately ten times the weight in grams of the normal person. With this formula in mind, it becomes easy to compute the nutritional state in percentages, when the sitting height and the weight are known. The formula would read:
or
Diet, in fevers, 244
in infectious diseases, 244,
244j
Diphtheria, 244d, 244k
complications of, 244d,
244k
convalescent diet in, 244e,
244k
dietetic treatment of, 244e,
244k
gavage in, 244k
rectal feeding in, 244e,
244k
Fevers, diet in, 244
Infant feeding, in infectious diseases, 244
Infectious diseases, diet in, 244, 244j
infant feeding in, 244
restricting diet in, 244a
Measles, 244h, 244l
complications of, 244h, 244l
dietetic treatment of, 244i, 244l
Nephritis in scarlet fever, 244c, 244j
Scarlet fever, 244b, 244j
convalescent treatment in, 244d
dietetic treatment of, 244c,
244j
nephritis in, 244c, 244j
Whooping cough, 244e, 244k
after-effects of, 244f
complications of, 244f,
244k
dietetic treatment of, 244f,
244k
hygiene and sanitation in, 244g
A B C D E F G H I J K L M N O P Q R S T U V W Y Z
Absorption, 166, 176
defined, 166
in large intestine, 178
of carbohydrate, 177
of fat, 177
of mineral salts, 178
of proteins, 177
of water, 177
Acetone bodies, in diabetes, 401
Acetone in urine, test for, 333
Acid, uric, see Uric acid
Acid content of stomach, determining of, 248
Acidosis, 453, 454, 458
dietetic treatment in, 453, 458
fat metabolism in, 453
in diabetes mellitus, 372, 382,
401, 454
in typhoid fever, 299
Added urea and salt test, 351
Adenase, 171
Adenin, 184
Adipose tissue, 15
Adult, factors influencing food requirement of, 43
Agar jelly, preparation of, 147
Age, influence of on food requirements, 43
Albumen, in urine, 333
tests for, 333
Albumen milk, preparation of, 142
Albumen water, with brandy, preparation of, 141
Albumenized grape juice, preparation of, 97
lemonade, preparation of, 97
milk, preparation of, 87
milk shake, preparation of, 87
orangeade, preparation of, 96
Albumins, 20
Albuminoids, 21
Albuminuria, 333
of pregnancy, diet in, 197
Alcohol in gout, 418
Alfalfa, vitamines in, 498
Alkalies, effect of on vitamine B, 32
in diabetes mellitus, 382
in infant feeding, 205, 206
Alkaline carbonates, effect of on gastric secretion, 175
Allen’s Paradoxical Law, 371
starvation treatment in diabetes, 63, 372
Almond biscuits, preparation of, 157
Almond flour, preparation of, 158
Almond ice cream, preparation of, 91
Almond meal, preparation of, 158
Almonds, ash constituent of, 472
composition of, 484
food content of, 478
fuel value of, 461, 484
nutrient value of, 461
standard portion of, 478
Amino acids, 19
Ammonium salts, 183
Anabolism, 181
Anemia, in gastric ulceration, 255
Angel food cake, preparation of, 110
Appendicitis, 268, 278
convalescent diet in, 269, 278
dietetic treatment in, 269, 278
after operation, 317, 321
food to be avoided in, 269
recurring, 278
relapse in, 278
Apples, ash constituent of, 472
composition of, 484
food content of, 478
fuel value of, 461, 484
nutrient value of, 461
standard portion of, 478
vitamines in, 497
Apple tapioca pudding, preparation of, 107
Apricot ice, preparation of, 137
Apricots, ash constituent of, 472
composition of, 484
[Pg 506]
food content of, 478
fuel value of, 461, 484
nutrient value of, 461
standard portion of, 478
Arrowroot, composition of, 484
fuel value of, 484
Artificial feeding of infants, 205
Artificially fed infants, digestive disturbances in, 231
Artichoke, composition of, 484
fuel value of, 461, 484
nutrient value of, 481
Ash, 25
Ash constituents of foods, 472, 473, 474, 475, 476, 477
Asparagus, ash constituent of, 484
composition of, 484
food content of, 478
fuel value of, 461, 484
nutrient value of, 461
standard portion of, 478
Auto-intoxication, 273
absorption of toxins in, 273
care of bowels in, 273
convalescent diet in, 275
dietetic treatment of, 273
Autolytic enzymes, 171
Avocado, fuel value of, 461
nutrient value of, 461
Bacon, ash constituent of, 472
composition of, 484
food content of, 478
fuel value of, 461, 484
nutrient value of, 461
standard portion of, 478
Bacteria, action of in alimentary canal, 178
types of, 180
Bacterial action, in body, 180
upon carbohydrates, 13
Bacterial activity, 181
Baked custard, preparation of, 102
Baked onion, preparation of, 151
Baked potato, preparation of, 130
Baked tapioca, preparation of, 106
Baking, 71
Bananas, ash constituent of, 472
composition of, 484
food content of, 478
fuel value of, 461, 484
nutrient value of, 461
standard portion of, 478
vitamines in, 497
Banting’s method for obesity, 426, 427
Barley, ash constituent of, 472
composition of, 484
fuel value of, 461, 484
nutrient value of, 461
vitamines in, 496
Barley water, 220
preparation of, 140
Basal metabolism, 42
Basal requirements, 42
Bass, composition of, 484
fuel value of, 484
Beans, ash constituent of, 472
composition of, 484
food content of, 478
fuel value of, 461, 484
nutrient value of, 461
standard portion of, 478
vitamines in, 497
Beef, and see Meats
ash constituents of, 472
cuts of, 117
food content of, 473
fuel value of, 462, 463,
484
composition of, 484
methods of preparing, 117
nutrient value of, 462, 463
standard portion of, 478
vitamines in, 496
Beef broth, preparation of, 118
Beef juice, preparation of, 119, 141
Beef steak, preparation of, 123
Beer, ash constituents of, 472
Beets, ash constituent of, 472
composition of, 484
food content of, 478
fuel value of, 463, 484
nutrient value of, 463
standard portion of, 478
vitamines in, 496
Benedict’s test for sugar in urine, 328, 329, 331, 332
Bile, 174
Birds à la bain marie, preparation of, 121
Blackberries, ash constituent of, 472
fuel value of, 463
nutrient value of, 463
Blackfish, fuel value of, 463
nutrient value of, 463
Blood, ash constituent of, 472
vitamines in, 498
Bluefish, ash constituent of, 472
composition of, 484
fuel value of, 463, 484
nutrient value of, 463
[Pg 507]
Body, 165
chemical composition of, 165
food requirements of, 42, 50,
165
metabolism of tissues of, 187
Boas’ enema, preparation of, 146
Boiled corn beef with cabbage and other vegetables, preparation of, 153
Boiling, 70
Bomb calorimeter, 36
Borax, test for, 68
Boric acid, test for, 68
Boston crackers, fuel value of, 463
nutrient value of, 463
Bowels, of nursing mother, 197
Boys, height and weight of, 500
Brains, vitamines in, 496
Bran, composition of, 484
fuel value of, 484
Bran agar wafers, preparation of, 146
Bran biscuits, preparation of, 149, 155,
156
for constipation, 156
Bran cookies, preparation of, 145
Bran gems, preparation of, 144
Bran muffins, preparation of, 155
Brandy, composition of, 484
fuel value of, 484
Brazil nuts, fuel value of, 463
nutrient value of, 463
Bread, ash constituent of, 472
composition of, 484, 486
fuel value of, 463, 464,
484, 486
nutrient value of, 463, 464
vitamines in, 496
Breadfruit, ash constituent of, 472
Breadstuffs, preparation of, 103
Bread substitutes, preparation of, 155
Breast feeding versus artificial feeding, 243
Breast milk, as a food, 228
versus cow’s milk, 203
Brick feeder, 225
Bright’s disease, see Nephritis
Broiled oysters, preparation of, 123
Broiled quail, preparation of, 121
Broiled squab, preparation of, 121
Broiled tomatoes, preparation of, 133
Broiling, 71
Broths, preparation of, 118
standard, 118
Brown betty, preparation of, 107
Brussels sprouts, ash constituent of, 472
Buckwheat flour, ash constituent of, 472
fuel value of, 464
nutrient value of, 464
Bulgarian buttermilk, preparation of, 89
Butter, ash constituent of, 472
composition of, 486
food content of, 478
fuel value of, 464, 486
nutrient value of, 464
standard portion of, 478
vitamines in, 497, 498
Buttermilk, ash constituent of, 472
fuel value of, 464
nutrient value of, 464
Buttermilk, Bulgarian, preparation of, 89
Buttermilk mixtures, 208
for infants, 142
Butternuts, fuel value of, 464
nutrient value of, 464
Cabbage, ash constituent of, 472
composition of, 486
food content of, 478
fuel value of, 464, 486
nutrient value of, 464
standard portion of, 478
vitamines in, 496
Cabbage soufflé, preparation of, 150
Calcium, 27, 186
requirements in pregnancy and lactation, 191
retention in rickets, 241
source of, in food, 6
Calculating formulas for infant feeding, 212
Calf’s-foot jelly, fuel value of, 464
nutrient value of, 464
preparation of, 120
Calorie, defined, 37
Calorie allowance for children, 48
Calories, in carbohydrates, 38
in fats, 38
in proteins, 38
Calorimeter, 36
Cancer, gastric, dietetic treatment of, 260
Canned goods, 68, 128
adulteration of, 68
Cane sugar, in infant feeding, 228
Cantaloupe, ash constituent of, 472
Capers, ash constituent of, 472
Caramel custard, preparation of, 103
[Pg 508]
Carbohydrates, 7
absorption of, 177
bacterial action upon, 13
calories in, 38
composition of, 7
effect of heat upon, 14
enzymes acting upon, 171
fate of, 182
function of, 372
metabolism of, 182
rate of digestion of, 173
regulation of, 235
source of, 5
tolerance of in diabetes, 380
Carbohydrate-free diet, 63
Carbohydrate-free meat and fish, calorie equivalent of, 386
Carbon dioxide, excretion of, 324
Carbonates, alkaline, effect of on digestion, 175
Carp, see Fish
Carrots, ash constituent of, 472
composition of, 486
food content of, 478
fuel value of, 464, 486
nutrient value of, 464
standard portion of, 478
vitamines in, 496
with cream sauce or butter, preparation of, 129
Casoid flour and bran muffins, preparation of, 156
Catabolism, 181
Cauliflower, ash constituent of, 472
composition of, 486
food content of, 478
fuel value of, 464, 486
nutrient value of, 464
standard portion of, 478
vitamines in, 496
Caviar, ash content of, 472
Celery, ash constituent of, 473
composition of, 486
food content of, 479
fuel value of, 464, 486
nutrient value of, 464
standard portion of, 479
vitamines in, 496
Celery ramekins, preparation of, 151
Celery soup, fuel value of, 464
nutrient value of, 464
Cellu bran crackers, preparation of, 148
Cellulose, 12
Centigrade scale, 80
Cereal pudding, preparation of, 110
Cerealine, fuel value of, 464
nutrient value of, 464
Cereals, preparation of, 103
vitamines in, 496, 497
Certified milk, 81
Chard, ash constituent of, 473
composition of, 486
fuel value of, 464, 486
nutrient value of, 464
vitamines in, 496
Cheese, ash constituent of, 473
composition of, 486
food content of, 479
fuel value of, 464, 486
nutrient value of, 464
standard portion of, 479
vitamines in, 498
Cheese salad, preparation of, 154
Cherries, ash constituent of, 473
composition of, 486
food content of, 479
fuel value of, 464, 486
nutrient value of, 464
standard portion of, 479
Cherry juice, ash constituent of, 473
Chestnuts, ash constituents of, 473
composition of, 486
fuel value of, 464, 486
nutrient value of, 464
vitamines in, 498
Chicken, and see Meat
composition of, 486
food content of, 479
fuel value of, 465, 486
nutrient value of, 465
preparation of, 122
selection of, 114
standard portion of, 479
Chicken à la bain marie, preparation of, 121
Chicken broth, preparation of, 118
Chicken jelly, preparation of, 120
Chicken salad, poisoning by, 451
Chicken supreme, preparation of, 149
Children, care of in abnormal conditions,
231
diarrhea in, 263, 276
energy requirements of, 47
errors in diet in, 232, 243
feeding of, in abnormal conditions, 231
food allowance for, 48
food requirements of, 44, 52
gain in weight in, 49
[Pg 509]
heights and weights for, 499
malnutrition in, 242
nutrition in, 502
over-feeding, 243
under-feeding, 243
Chlorine, source of in food, 6
Chocolate, ash constituent of, 473
composition of, 486
food content of, 479
fuel value of, 465, 486
nutrient value of, 465
standard portion of, 479
Cholesterol, 15
Cider, ash constituents of, 473
Citron, ash constituents of, 473
Clams, ash constituents of, 473
composition of, 486
food content of, 479
fuel value of, 486
standard portion of, 479
Clam broth, preparation of, 119
Clover, vitamines in, 498
Cocoa, ash constituents of, 473
composition of, 486
food content of, 479
fuel value of, 465, 486
nutrient value of, 465
preparation of, 89
standard portion of, 479
Cocoanut, ash constituents of, 473
vitamines in, 498
Cocoanut biscuits, preparation of, 158
Cocoanut flour, preparation of, 158
Coddled eggs, preparation of, 100
Codfish, and see Fish
composition of, 486
fuel value of, 465, 486
nutrient value of, 465
vitamines in, 496
Coffee, adulteration of, 69
preparation of, 98
Coffee eggnog, preparation of, 99
Coleman’s high calorie diet in typhoid fever, 289, 291, 294, 295, 298, 299
Condensed milk, composition of,
486
for infants, 226, 227
fuel value of, 486
vitamines in, 498
Conserve, preparation of, 143
Consommé, composition of, 486
fuel value of, 465, 486
nutrient value of, 465
Constipation, bran biscuits for, 156
dietetic treatment of, 271, 279
diet for, 143, 239,
271, 272, 279,
406
in nursing women, 197
Convalescent diet, 62
Cookies, protein-free, 340
Cooking, time-table for, 72
Copper, test for, 68
Corn, ash constituents of, 473
composition of, 486
food content of, 479
fuel value of, 465, 486
nutrient value of, 465
standard portion of, 479
vitamines in, 497
Cornflakes, composition of, 486
fuel value of, 486
Corn meal, composition of, 486
food content of, 479
fuel value of, 465, 486
nutrient value of, 465
standard portion of, 479
Cornstarch, composition of, 486
fuel value of, 486
Cotton seed, ash constituents of, 473
vitamines in, 497
Cowpeas, ash constituents of, 473
fuel value of, 465
nutrient value of, 465
Crab, preparation of, 126
Crackers, ash constituents of, 473
composition of, 486
food content of, 479
fuel value of, 465, 486
nutrient value of, 465
standard portion of, 479
Cranberries, ash constituents of, 473
composition of, 488
fuel value of, 465, 488
nutrient value of, 465
Cream, ash constituents of, 473
composition of, 488
food content of, 479
fuel value of, 465, 488
nutrient value of, 465
standard portion of, 479
vitamines in, 498
Cream egg and vichy, preparation of, 98
Cream of asparagus, preparation of, 93
of carrots, preparation of, 94
of cauliflower, preparation of, 152
of celery, preparation of, 94
of peas, preparation of, 94
of potato, preparation of, 94
of spinach, preparation of, 94
[Pg 510] Cream sauce for soups, preparation of, 93
Cream soups, preparation of, 93
Cream toast, preparation of, 105
Creamed egg on toast, preparation of, 101
Creamed potatoes, preparation of, 130
Creatinin, 185
Cucumber, ash constituents of, 473
composition of, 488
fuel value of, 465, 488
nutrient value of, 465
Cucumber salad, preparation of, 131
Currant ice, preparation of, 137
Currant juice, ash constituents of, 473
Currants, ash constituents of, 473
composition of, 488
fuel value of, 465, 488
nutrient value of, 465
Custard, preparation of, 102, 159
Dairy products, 81
vitamines in, 498
Dandelion greens, ash constituents of, 473
fuel value of, 465
nutrient value of, 465
Dasheens, vitamines in, 496
Dates, ash constituents of, 473
composition of, 488
food content of, 479
fuel values of, 465, 488
nutrient value of, 465
standard portion of, 479
Desserts, preparation of, 138
Dextri-maltose, 236
in infant feeding, 207
Dextrin, 12
Diabetes mellitus, 371
acetone bodies in, 401
acidosis in, 372, 382,
401, 454
alkalies in, 382
Allen’s starvation treatment in, 372
carbohydrate-free diets in, 387, 389
carbohydrate tolerance in, 380
determination of food tolerance in, 379
dietetic treatment in, 382
diets in, 374, 382
in mild cases, 373
fast days in, 381
fasting in, 379
Diabetes mellitus, fat tolerance in, 381
formulas used in, 146
Joslin’s diet in, 383
menus for, 376, 377,
383, 389, 397
protein tolerance in, 381
schedule of treatment for, 380
starvation treatment of, 372
test diets in, 374
urine in, 328, 329,
330, 371, 401,
402
Diabetic acidosis, 454
Diabetic cures, 372
Diabetic flours, 403
Diabetic foods, commercial, 403
Diabetic muffins, preparation of, 155
Diacetic acid in urine, Gerhardt’s test for, 332
Diarrhea, 263,
276, and see Enteritis
causes of, 263, 276
dietetic treatment of, 264
in children, 263
dietetic treatment of, 237
Diastase, 171
Diet, or Diets, and see under the various diseases
carbohydrate-free, 63
convalescent, 62
diabetic, 63
emaciation, 63
fluid, 63
house, 62
light, 62
liquid, 62
milk, 63
mixed, 63
nephritic, 63, and see Nephritis
obesity, 63, and see Obesity
protein-free, 340
purin-free, 63
salt-free, 63
semi-solid, 62
special, 62, 63
Dietary, for child, 221, 223
sample, 54
Dieto-therapy, 189
Digestion, 167
chemical, 169, 172
gastric, 172
intestinal, 173, 176
processes included in, 166
salivary, 172
Digestive disturbances in infants and children, 231
Diluents, in infant feeding, 208
preparation of, 210
[Pg 511] Dilution for premature infants, 225
Dish gravy, 141
Dishes, washing, 76
Doughnuts, fuel value of, 465
nutrient value of, 465
Dry peptonoids, composition of, 488
fuel value of, 488
Duck, see Meat
Dysentery, dietetic treatment of, 268, 278
Ebstein’s method for obesity, 429
Egg, or Eggs, 95
ash constituents of, 473
composition of, 488
coddled, 100
food content of, 479
fuel value of, 465, 488
nutrient value of, 465
standard portion of, 479
vitamines in, 497, 498
Egg nest, preparation of, 101
Eggnog, preparation of, 99
Eggplant, ash constituents of, 473
composition of, 488
fuel value of, 465, 488
nutrient value of, 465
Egg salad, preparation of, 154
Eggwhite and mint, preparation of, 98
Elimination, 167
Emaciation, 438
allowable foods in, 441
dietetic treatment in, 440
diet in, 63, 439
diet sheets, 442, 443
in children, 438
method of increasing diet in, 444
milk cure in, 441
need for building foods in, 439
regulating diet in, 439
selection of foods in, 440
Endive, ash constituents of, 473
Enema, or Enemas, malted milk, 146
milk and egg, 145
milk and starch, 146
nutrient, 145
temperature of, 61
Energy output compared with food intake, 425
production of, 182
Enteritis, acute, 264, and see Diarrhea
Enteritis, acute, dietetic treatment of, 264, 265,
266, 276, 277
foods to be avoided in, 266, 277
Enteritis, chronic, 267
dietetic treatment in, 267
Enterocolitis, 267, 277
dietetic treatment of, in infants, 237
Enzymes, 170, 171
acting, on carbohydrates, 171
on fats, 171
on proteins, 171
on purins, 171
action of, 170, 171
amylolytic, 172
autolytic, 171
classification of, 172
coagulating, 172
deaminizing, 172
glycolytic, 171
hydrolytic, 172
lipolytic, 172
oxidizing, 172
proteolytic, 172
reducing, 172
source of, 171
sugar-splitting, 172
table of, 171
Errors in diet, in infants and children, 232, 243
Fahrenheit scale, 80
Farina, ash constituents of, 473
composition of, 488
food content of, 479
fuel value of, 465, 488
nutrient value of, 465
preparation of, 104
standard portion of, 479
Fast days, in treatment of diabetes, 381
Fat, or Fats, 14, 15
absorption of, 177
calories in, 38
cause of gastro-intestinal disturbances in children, 233
effect of heat upon, 16
enzymes acting on, 171
excess of, in diet of infants and children, 233
fate of, 182
functions of, 17
metabolism of, in acidosis, 453
phosphorized, 15
rate of digestion of, 173
regulation of, in diet, 233
[Pg 512]
source of, 5, 448
tolerance of, in diabetes, 381
vitamines in, 497, 498
Fat soluble A, 15
effect of heat upon, 31
function of, 30
foods containing, 6, 496,
497, 498
Fatty foods, effect of, upon gastric secretion, 175
Feeding, by inunction, 62
by mouth, 59
correct, evidences of, 243
forced, 59
in diseases of gastro-intestinal tract, 245
infant, see Infant feeding
methods of, 59
post-operative, 316, 319,
320
pre-operative, 312, 318,
320
rectal, 60, 61
Fehling’s solution, 331
Fehling’s test for sugar in urine, 328
Fermentation, and see Enzymes
cause of infantile disorders, 236, 237
in stomach, 180
Fermentation test for sugar in urine, 330
Fever, or Fevers, 281
care of mouth in, 285
convalescent diet in, 283
dietetic treatment in, 281
energy expenditure in, 288
energy requirements in, 285
fluid diet in, 282
nitrogen equilibrium in, 286
sample menus for, 284
schedule of feeding in, 282
soft diet in, 283
thirst in, 285
tissue waste in, 281
typhoid, see Typhoid fever
Figs, ash constituents of, 473
composition of, 488
food content of, 479
fuel value of, 465, 488
nutrient value of, 465
standard portion of, 479
Fish, 115
ash constituents of, 473
composition of, 488
food content of, 479
fuel value of, 488
standard portion of, 479
Fish roe, vitamines in, 496
Fish steaks stuffed with oysters, preparation of, 125
Flaxseed, ash constituents of, 474
vitamines in, 497
Floating island, preparation of, 103
Flounder, fuel value of, 465
nutrient value of, 465
Flour, ash constituents of, 474
composition of, 488
food content of, 479
fuel value of, 465, 488
nutrient value of, 465
standard portion of, 479
Flours, diabetic, 403
Foamy omelet, preparation of, 100
Foamy sauce, preparation of, 111, 112
Food, or Foods, 1, and see Foodstuffs
acid-forming, 184, 454
adulteration of, 67
allowance for children, 48
arrangement of, in stomach, 167
as fuel, 24, 36, 39
ash constituents of, 472, 473,
474, 475, 476,
477
base-forming, 184, 454
care of, 76
chemical composition of, 3, and 484 to
495
contamination of, 66
defined, 2
diabetic, 403
effect of cold upon, 39
effect of heat upon, 39
fuel value of, 36, 39,
221, 461 to 471, and
484 to 495
functions of, 2
idiosyncrasies to, 452
incomplete, as source of danger, 227
intake of, compared with output of energy, 425
materials, 2
mineral matter in, 25
nutrient value of, 461 to 471
passage of, from stomach, 168
preparation of, 69, 70
purin content of, 421
relation of, to mother’s milk, 203
requirements of body, 42, 43,
51, 52
factors influencing, 43, 44
salt content of, 358, 359,
360
selection of, 52, 75
[Pg 513]
sources of, 2, 3, 4
transformation of into fuel, 37
uses of, 2, 425
vitamines in, 496, 497,
498
which produce fat, 448
Food materials, 2
Foodstuffs, heat produced by oxidation of, 38
Forced feeding, 59
Formaldehyde, test for, 67
Formulas, determining fuel value of, 221
for constipation, 143
for feeding infants, 140, 212
Fowls, and see Meat
composition of, 488
fuel value of, 466, 488
nutrient value of, 466
French dressing, preparation of, 134
Frozen custard, preparation of, 91
Fructose, 9
Fruit, preparation of, 126, 127,
128
vitamines in, 497
Fruit beverages, preparation of, 96
Fruit jellies, method for, 135
preparation of, 160
Fruit salads, preparation of, 131, 132
Fruit sauce, preparation of, 111
Frying, 71
Fuel value of food, 36
to compute, 39, 221
Galactose, 9
Gall bladder, diet after operations on, 318, 321
Gallstones, 408
available foods, 410
dietetic treatment for, 408, 409
diet sheets for, 411, 412,
413
Gastric, and see Stomach
Gastric cancer, 260
dietetic treatment in, 260
Gastric digestion, 172
factors influencing, 175
Gastric, disturbances, factors inducing, 261, 262
Gastric hemorrhage, 251
Gastric juice, composition of, 246
retardation of, 175
stimulation of, 175
Gastric secretion, effect of alkaline
carbonates on, 175
effect of fatty foods upon, 175
water as a stimulant, 253
Gastric ulcer, 251
bland diet in, 255
convalescent diet in, 254
dietetic treatment in, 252, 256
lavage in, 255
Lenhartz diet in, 257
starvation treatment of, 252
Gastritis, acute, 248
dietetic treatment in, 248, 249
Gastritis, chronic, 250
dietetic treatment of, 250
Gastro-enterostomy, diet after, 321
Gastro-intestinal disturbances, relapses in, 244
Gastro-intestinal tract, feeding in diseases of, 245
Gavage, 60
Gelatin, composition of, 488
food content of, 480
fuel value of, 466, 488
nutrient value of, 466
standard portion of, 480
Gelatin jellies, preparation of, 135
Gerhardt’s test for diacetic acid, 332
Girls, heights and weights for, 501
Globulins, 20
Glucose, 8
Gluten food, ash constituents of, 474
Glycogen, 12
Glycolytic enzymes, 171
Goose, see Meat
Gooseberries, ash constituents of, 474
Gout, 417
alcohol in, 412
allowable foods in, 420
avoidable foods in, 420, 421
dietaries in, 422
dietetic treatment in, 420, 445
foods to be condemned in, 420
glycosuria in, 419
obesity in, 419
purin-free diet in, 410
Grape butter, fuel value of, 466
nutrient value of, 466
Grapefruit, ash constituents of, 474
composition of, 488
food content of, 480
fuel value of, 466, 488
nutrient value of, 466
standard portion of, 480
vitamines in, 497
Grape juice, ash constituents of, 474
[Pg 514]
composition of, 488
food content of, 480
fuel value of, 488
standard portion of, 480
vitamines in, 497
Grape juice ice, preparation of, 136, 137
Grape juice jelly, preparation of, 135
Grapes, ash constituents of, 474
composition of, 488
food content of, 480
fuel value of, 466, 488
nutrient value of, 466
standard portion of, 480
vitamines in, 497
Greens, composition of, 488
fuel value of, 488
Guanase, 171
Guava, ash constituents of, 474
Gum gluten, composition of, 488
fuel value of, 488
Haddock, and see Fish
fuel value of, 466
nutrient value of, 466
Haines’ solution, 331
Haines’ test for sugar in urine, 329
Halibut, and see Fish
composition of, 488
fuel value of, 466, 488
nutrient value of, 466, 488
Halpin’s salt-free nephritic diet, 342
Ham, and see Meat
composition of, 488
fuel value of, 466, 488
nutrient value of, 466
Hard sauce, preparation of, 111
Hazel nuts, ash constituents of, 474
Heat, application of to milk, 84
effect of on carbohydrates, 14
effect of on fats, 16
effect of on proteins, 22
effect of on vitamine A, 31
effect of on vitamine B, 32
effect of on vitamine C, 33
produced by oxidation of foodstuffs, 38
Hedinger-Schlayer-Mosenthal diet, 348, 350
Heights and weights for children, 499, 500, 501
Heller’s test for albumen in urine, 333
Hemoglobin, 22
Hemorrhages, gastric, 251
Hempseed, vitamines in, 497
Herring, and see Fish
fuel value of, 466
nutrient value of, 466
vitamines in, 496
Hickory nuts, composition of, 488
fuel value of, 488
High calorie diet, in tuberculosis, 304
in typhoid fever, 289, 291,
294, 295, 298,
299
Hollandaise sauce, preparation of, 126
Hominy, ash constituents of, 474
composition of, 488
food content of, 480
fuel value of, 466, 488
nutrient value of, 466
standard portion of, 480
Homogenized milk, 209
Homogenizer, 209
Honey, ash constituents of, 474
composition of, 488
food content of, 480
fuel value of, 466, 488
nutrient value of, 466
standard portion of, 480
vitamines in, 498
Horse meat, vitamines in, 496
Horseradish, ash constituents of, 474
House diet, 62
Household weights and measures, 78
Huckleberries, ash constituents of, 474
fuel value of, 466
nutrient value of, 466
Huckleberry wine, ash constituents of, 474
Hydrochloric acid, in gastric juice, 246
Hyperchlorhydria, 247
Hypochlorhydria, 246
Ice-box, care of, 73
Ice cream, poisoning by, 451
preparation of, 161
to reënforce, 91
Ices, preparation of, 161
Idiosyncrasies, to milk, 296
to foods, 452
Ileocecal valve, 176
Indican, test for in urine, 334
Infancy, retention of nitrogen in, 201
[Pg 515]
Infant, or Infants, and see Children
bath for, 202
bowels of, 202
care of in abnormal conditions, 231
daily gain in weight, 200
danger of incomplete foods, 227
digestive disturbances in, 231
energy requirements of, 198
enterocolitis in, 237
errors of diet in, 232, 243
feeding, see Infant feeding
food for, 201
foods, see Infant foods
over-feeding, 243
premature, see Premature infants
proprietary foods for, 226
quantity of milk needed for, 198
under-feeding, 243
weight of, 201
Infant feeding, 199
alkalies used in, 205, 206
amount given at each meal, 211
artificial, 205
breast versus artificial, 243
cane sugar in, 228
diluents in, 208, 228
formulas for, 140, 212,
229
in abnormal conditions, 231
lime water in, 206, 221
malt sugar in, 228
method of calculating formulas for, 212
milk sugar in, 228
Morse and Talbot’s method in, 215
normal, 201
over-dilution in, 232
regularity in, 201, 228
rules and regulations for, 204
scheme for, 217, 219
sugar in, 207
under-dilution in, 232
water in, 229
Infant foods, 140
addition of alkali to, 228
dilution of, 208, 228
increasing, 229
percentage, computation of, 229
preparation of, 229
scheme for adding solids to, 221
Infected food materials, 451
Intestinal digestion, 173
Intestinal secretions, stimulation of, 174
Intestinal tract, diseases of, 263
Intestines, behavior of foods in, 168
movements of, 168, 169
muscular contractions in, 169
Inunction, feeding by, 62
Invertase, 171
Iodine, source of in food, 6
Irish moss pudding, preparation of, 160
Iron, 28
sources of in food, 5
Jam, ash constituents of, 474
Jellies, ash constituents of, 474
preparation of, 159
Jello, composition of, 490
fuel value of, 490
Joslin’s treatment in diabetes, 383
Junket, preparation of, 90
Junket ice cream, preparation of, 90
Kidneys, function of, 323
functional tests for, 347, 348,
349, 351
limiting work of, 337
operations on, diet after, 318, 321
resting of, in nephritis, 338
vitamines in, 496
Kohl-rabi, ash constituents of, 474
composition of, 490
fuel value of, 466, 490
nutrient value of, 466
Koumiss, composition of, 490
fuel value of, 466, 490
nutrient value of, 466
Lactase, 171
Lactation, diet in, 191, 194, 197
Lactone buttermilk, preparation of, 91
Lactose, 8, 11
composition of, 490
fuel value of, 490
in infant feeding, 207
Lady fingers, composition of, 490
fuel value of, 490
Lamb, 112, and see Meats
composition of, 480
cuts of, 117
food content of, 480
fuel value of, 467, 490
nutrient value of, 467
standard portion of, 480
Lamb chops, preparation of, 124
Lard, composition of, 490
fuel value of, 467, 490
[Pg 516]
nutrient value of, 467
vitamines in, 497, 498
Lavage, 248
in gastric ulceration, 255
Leeks, ash constituents of, 474
Lemon, ash constituents of, 474
food content of, 480
fuel value of, 467
nutrient value of, 467
standard portion of, 480
vitamines in, 497
Lemonade, albumenized, preparation of, 97
Lemon cream, preparation of, 138
Lemon ice, preparation of, 136, 137, 161
Lemon ice cream, preparation of, 91
Lemon jelly, preparation of, 135, 159
Lemon juice, ash constituents of, 474
composition of, 490
fuel value of, 467, 490
nutrient value of, 467
Lenhartz diet, in gastric ulceration, 257
Lentils, ash constituents of, 474
composition of, 490
food content of, 480
fuel value of, 490
standard portion of, 480
Lettuce, ash constituents of, 474
composition of, 490
food content of, 480
fuel value of, 467, 490
nutrient value of, 467
standard portion of, 480
vitamines in, 496
von Leube’s enema, preparation of, 146
Limes, ash constituents of, 474
vitamines in, 497
Lime juice, ash constituents of, 474
Lime water, in infant feeding, 206, 221
Linen, 64
Linseed meal, ash constituents of, 474
Lipase, 171
Liquid diet, 62
Liquid peptonoid eggnog, preparation of, 99
Liquid peptonoids, composition of, 490
fuel value of, 490
Lister cream puff, preparation of, 159
Lister flour and bran muffins or biscuits, preparation of, 156
Lister muffins, preparation of, 155
Liver, cirrhosis of, 407
avoidable foods for, 408
dietetic treatment in, 407
composition of, 490
diseases of, 404
convalescence, diet in, 405
dietetic treatment in, 405, 414
fuel value of, 467, 490
functions of, 413
nutrient value of, 467
operations on, diet after, 318, 321
vitamines in, 496
work of, 404
Lobster, composition of, 490
fuel value of, 467, 490
nutrient value of, 467
preparation of, 126
Lupins, ash constituents of, 474
Macaroni, ash constituents of, 480
composition of, 490
food content of, 480
fuel value of, 467, 490
nutrient value of, 467
standard portion of, 480
Macaroons, fuel value of, 467
nutrient value of, 467
Mackerel, and see Fish
composition of, 490
fuel value of, 467, 490
nutrient value of, 467
Magnesium, source of in foods, 6
Maize, vitamines in, 496
Malnutrition, 242
Maltase, 171
Malt extract, vitamines in, 497, 498
Malt soup, preparation of, 141
Malt sugar, in infant feeding, 207, 208
Malted foods, for infant feeding, 207, 226, 227
Malted milk, composition of, 490
fuel value of, 490
preparation of, 92
Malted milk chocolate, preparation of, 92
Malted milk cocoa, preparation of, 92
Malted milk eggnog, preparation of, 99
Malted milk enema, 146
Mamey, ash constituents of, 475
Mango, ash constituents of, 475
[Pg 517]
Mangolds, ash constituents of, 475
vitamines in, 496
Maple syrup, ash constituents of, 475
Marmalade, fuel value of, 467
nutrient value of, 467
Mayonnaise, preparation of, 475
Meals, serving suggestions for, 56, 66
Measures and weights, 77
household, 78
Meat extract, ash constituents of, 475
Meat peptone, ash constituents of, 475
Meats, 112
ash constituents of, 475
carbohydrate-free, calorie equivalent of, 386
cuts of, 117
quality of, 113
selection of, 116
vitamines in, 496
Metabolism, 166, 181
basal, 42
mineral, 185
of body tissues, 187
of carbohydrates, 182
of proteins, 183
Metric system, 77
Milk, 82
adulteration of, 86
application of heat to, 84
ash constituents of, 475
breast versus cows’, 203
care of, 86
certified, 81
composition of, 205, 490
condensed, see Condensed milk
diet, 63
fats in, measuring according to, 210
food content of, 480
formulas, 212, 214,
216, 217
fuel value of, 467, 490
homogenized, 209
idiosyncrasies against, 296
method of administering to premature infants, 225
modification of, technique of, 209, 228
nutrient value of, 467
pasteurization of, 85, 211
quantity of needed for infant, 198
relation of food to, 203
secretion of, factors retarding, 195, 197
factors stimulating, 195, 197
selection of, 86
standard portion of, 480
sterilization of, 84
substitutes for whole, 228
sugar-free, 162
use of in nephritis, 162
vitamines in, 498
Milk and egg enemas, preparation of, 145
Milk and starch enemas, preparation of, 146
Milk cure in nephritis, 338
Milk powder, food content of, 480
standard portion of, 480
vitamines in, 498
Milk punch, preparation of, 88
Milk sauce, preparation of, 93
Milk shake, preparation of, 87
Milk sherbet, preparation of, 138
Milk soups, preparation of, 93
Milk sugar, in infant feeding, 228
Milk toast, preparation of, 105
Millet, ash constituents of, 475
Millet seed, vitamines in, 497
Mince meat, fuel value of, 467
nutrient value of, 467
Mineral metabolism, 185
Mineral oils, use of in constipation, 279
Mineral requirements of body, 50
Mineral salts, 25, 26
absorption of, 178
sources of in foods, 5
Mixed diet, 63
Molasses, ash constituents of, 475
composition of, 490
food content of, 480
fuel value of, 467, 490
nutrient value of, 467
standard portion of, 480
Monosaccharides, 7
Morse and Talbot’s method of infant feeding, 215
Mother’s milk, fuel value of, 198
making of, 198
Mouth, care of in typhoid, 299
Muffins, diabetic, preparation of, 155
Mushrooms, ash constituents of, 475
composition of, 490
fuel value of, 467, 490
nutrient value of, 467
Muskmelon, ash constituents of, 475
[Pg 518]
composition of, 490
fuel value of, 467, 490
nutrient value of, 467
Mustard, ash constituents of, 475
Mutton, and see Meat
cuts of, 117
food content of, 480
fuel value of, 468
nutrient value of, 468
standard portion of, 480
Mutton broth, preparation of, 118
Mutton chops, preparation of, 124
Nectar, vitamines in, 498
Nectarines, fuel value of, 468
nutrient value of, 468
Nephritic diet, 63
Nephritis, 336
acute, 336
adjusting diet in, 338
adjusting fluids in, 338
advisable foods in, 344
causes of, 336
Chase and Rose’s diet in, 340
chronic, 336, 346
dietetic treatment in, 346
functional tests in, 347, 348,
351
protein diet in, 346
chronic interstitial, 352
dietetic treatment in, 352
limiting fluid in, 353
limiting nitrogen in, 353
selection and preparation of food in, 354
convalescent diet in, 344
diet in, 339, 345,
356
effects of, 336
elimination of salt in, 340
foods to be avoided in, 344
Halpin’s diet in, 342
Karell cure in, 342
limiting the amount of food in, 341
milk cure in, 338
preparation of food in, 343
problems to be considered in, 337
proteins in, 343
resting the kidneys in, 338
selection of foods in, 343
thirst in, 343
Widal’s diet in, 341
Neufchâtel cheese salad, preparation of, 154
Nitrogen, retention of in infancy, 201
source of in foods, 5
Nitrogenous substances, oxidation and excretion of, 324
Noodles, composition of, 490
fuel value of, 490
Noodle soup, preparation of, 149
Normal saline solution, preparation of, 146
Nucleoproteins, 21
Nursing infant, food requirements of, 194
Nursing mother, constipation in, 197
diet of, 195
habits of, 203
Nuts, vitamines in, 498
Nut charlotte, preparation of, 138, 162
Nutrient enemas, 145
Nutrition in children, 502
Nutritional index, 503
Oatmeal, ash constituents of, 475
composition of, 490
food content of, 481
fuel value of, 468, 490
nutrient value of, 468
standard portion of, 481
Oatmeal cookies, preparation of, 106
Oats, composition of, 490
fuel value of, 490
vitamines in, 496
Oat water, preparation of, 141
Obese women, Rose’s reducing diet for, 431, 432
Obesity, 424
allowable foods in, 429
amount of food to be taken in, 431
Banting’s method in, 426, 427
cures for, 425, 426
dietetic treatment of, 426, 429,
446
diets for, 63, 426
Ebstein’s method in, 429
exercise in, 426
in gout, 419
limiting fluids in, 426
massage in, 425
menus for, 430, 435,
436, 437
Oertel’s method for, 427
Proudfit’s menu for, 429, 433,
434
Rose’s diet for, 431, 432
Oertel’s method in obesity, 427
Okra, ash constituents of, 475
composition of, 490
[Pg 519]
fuel value of, 468, 490
nutrient value of, 468
Olives, ash constituents of, 475
composition of, 490
fuel value of, 468, 490
nutrient value of, 468
Olive oil, composition of, 490
fuel value of, 490
Olmstead bran cakes, preparation of, 148
Onion, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 468, 492
nutrient value of, 468
standard portion of, 481
vitamines in, 496
Operations, diet in relation to, 312
Orange, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 468, 492
nutrient value of, 468
standard portion of, 481
vitamines in, 497
Orangeade, preparation of, 96
Orange charlotte, preparation of, 138, 162
Orange ice, preparation of, 136, 137, 161
Orange jelly, preparation of, 135, 160
Orange rice custard, preparation of, 108
Orange tapioca, preparation of, 106
Organic acids, 13
Over-dilution of infant’s food, 232
Over-feeding of infants and children, 243
Oxidases, 171
Oxtail soup, fuel value of, 468
nutrient value of, 468
Oyster broth, preparation of, 119
Oyster soup, preparation of, 94
Oysters, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 468, 492
nutrient value of, 468
standard portion of, 481
Pancreas, vitamines in, 496
Panopepton, composition of, 492
fuel value of, 492
Panopepton eggnog, preparation of, 99
Paprika, ash constituents of, 475
Parsley butter, preparation of, 154
Parsnips, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 468, 492
nutrient value of, 468
standard portion of, 481
vitamines in, 496
Pea soup, fuel value of, 468
nutrient value of, 468
Peaches, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 468, 492
nutrient value of, 468
standard portion of, 481
Peanut butter, composition of, 492
fuel value of, 492
Peanuts, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 468, 492
nutrient value of, 468
standard portion of, 481
vitamines in, 497
Pears, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 468, 492
nutrient value of, 468
standard portion of, 481
vitamines in, 497
Pear juice, ash constituents of, 475
Peas, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 468, 492
nutrient value of, 468
standard portion of, 481
vitamines in, 496, 497
Pecans, ash constituents of, 475
composition of, 492
food content of, 481
fuel value of, 492
standard portion of, 481
“Pelidisi,” the, 503
Pelidisi chart, 502
Pellagra, dietetic treatment in, 455, 456, 459
Peppers, ash constituents of, 476
composition of, 492
food content of, 481
fuel value of, 469, 492
nutrient value of, 469
Pepsin, 171
[Pg 520] Peptonized milk, preparation of, 88
Peptonized milk punch, preparation of, 89
Peptonoids, dry, composition of, 488
fuel value of, 488
liquid, composition of, 490
fuel value of, 490
Percentage calculations, 79, 229
Perch, see Fish
Persimmons, ash constituents of, 476
fuel value of, 469
nutrient value of, 469
Phosphoproteins, 21
Phosphorized fats, 15
Phosphorus, 27, 186
requirements in pregnancy and lactation, 191
sources of in food, 5
Pies, fuel value of, 469
nutrient value of, 469
Pig heart, vitamines in, 496
Pineapple, ash constituents of, 476
composition of, 492
food content of, 481
fuel value of, 469, 492
nutrient value of, 469
standard portion of, 481
Pineappleade, preparation of, 97
Pine nuts, fuel value of, 469
nutrient value of, 469
Pistachios, fuel value of, 469
nutrient value of, 469
Placenta, vitamines in, 496
Plums, ash constituents of, 476
composition of, 492
food content of, 481
fuel value of, 469, 492
nutrient value of, 469
standard portion of, 481
Pneumonia, 306, 311
convalescent diet in, 307
diet schedules for, 307
dietetic treatment in, 306, 307,
311
Poached eggs, preparation of, 101
Poaching, 71
Pomegranates, ash constituents of, 476
fuel value of, 469
nutrient value of, 469
Pork, 116, and see Meat
fuel value of, 469
nutrient value of, 469
vitamines in, 498
Port wine, composition of, 492
fuel value of, 492
Postoperative feeding, 316, 319, 320
Potassium, sources of in food, 6
Potato chips, fuel value of, 469
nutrient value of, 469
Potatoes, ash constituents of, 476
composition of, 492
food content of, 481
fuel value of, 469, 492
nutrient value of, 469
standard portion of, 481
vitamines in, 496
Potatoes stuffed with meat, preparation of, 130
Pregnancy, 191
albuminuria in, 197
diet in, 192, 193,
194, 196, 197
nutritional disturbances in, 191
Premature infants, dilution of food for,
225
energy requirements of, 224
feeding of, 224, 225,
229
Pre-operative feeding, 312, 318, 320
Presbyterian Hospital diet list in typhoid fever, 292
Protein milk, preparation of, 142
Proteins, 17
alcohol-soluble, 21
calories in, 38
classification of, 19
composition of, 18
conjugated, 21
construction of, 19
effect of heat upon, 22,
enzymes acting upon, 171
excess of in infant’s and children’s food, 234
fate of, 183
function of in body, 23
metabolism, 183
in nephritis, 343
rate of digestion of, 173
requirements in body, 50
sources of, 4
tolerance of in diabetes, 381
Proudfit’s menu for obesity, 429
reducing diet for obesity, 433, 434
Prune fig whip, preparation of, 139
Prunes, ash constituents of, 476
composition of, 492
food content of, 481
fuel value of, 469, 492
nutrient value of, 469
standard portion of, 481
[Pg 521] Prunes and figs, preparation of, 143
Prune whip, preparation of, 139
Ptomaines, 66
poisoning by, 451
dietetic treatment for, 451, 452
Ptyalin, 171
Pumpkins, ash constituents of, 476
fuel value of, 469
nutrient value of, 469
Punch, milk, preparation of, 88
Purin bases, 184
content of food, 421
Purin-free diet, 63
in gout, 419
Purins, enzymes acting upon, 171
Quail, composition of, 492
fuel value of, 492
Radishes, ash constituents of, 476
food content of, 481
fuel value of, 469
nutrient value of, 469
standard portion of, 481
Raisins, ash constituents of, 476
composition of, 492
fuel value of, 469, 476
nutrient value of, 469
vitamines in, 497
Raspberries, ash constituents of, 476
composition of, 492
fuel value of, 470, 492
nutrient value of, 470
Respiratory tract, diseases of, 301
Requirements, basal, 42
Rhubarb, ash constituents of, 476
composition of, 492
food content of, 481
fuel value of, 470, 492
nutrient value of, 470
standard portion of, 481
Rice, ash constituents of, 476
composition of, 492
food content of, 481
fuel value of, 470, 492
nutrient value of, 470
preparation of, 104
standard portion of, 481
vitamines in, 496
Rice custard, preparation of, 108
Rickets, 241
calcium retention in, 241
dietetic treatment of, 241
Roast chicken, preparation of, 122
Roast duck, preparation of, 122
Roast turkey, preparation of, 122
Roasting, 71
Romaine, ash constituents of, 476
Rose’s reducing diet for obese women, 431, 432
Rum, composition of, 492
fuel value of, 492
Rutabaga, ash constituents of, 476
vitamines in, 496
Rye, and see Bread, and Flour
ash constituents of, 476
vitamines in, 497
Saccharine, test for, 69
Salad, egg, preparation of, 154
Salads, fruit, preparation of, 131
vegetable, preparation of, 131
Saline solution, normal, 146
Saliva, 172
Salivary digestion, 172
Salisbury steak, preparation of, 149
Salmon, and see Fish
composition of, 492
fuel value of, 470, 492
nutrient value of, 470
Salmon, molded, preparation of, 150
Salt, elimination of in nephritis, 340
Salt content of foods, 358, 359, 360
Salt-free diet, 63
Salt-poor diet for nephritis, 341
Saltines, composition of, 492
fuel value of, 492
Sapota, ash constituents of, 476
Sardines, composition of, 492
fuel value of, 492
Sauce for puddings, preparation of, 111, 112
Sausage, fuel value of, 470
nutrient value of, 470
Sautéing, 71
Scalloped potatoes, preparation of, 131
Secretin, 174
Secretory cells, distribution of, 169
Secretory processes disturbed in diseases of stomach, 246
Seeds, vitamines in, 497
Semi-solid diet, 62
Serving meals, suggestions for, 56, 66
Shad, composition of, 494
fuel value of, 470, 494
nutrient value of, 470
[Pg 522]
Sherry wine, composition of, 494
fuel value of, 494
Shredded wheat, ash constituents of, 476
food content of, 481
fuel value of, 470
nutrient value of, 470
standard portion of, 481
Shrimp, ash constituents of, 476
Silver, 64
Simmering, 70
Singer’s enema, preparation of, 146
Sippi diet, in gastric ulceration, 256
Snow-balls, preparation of, 108
Snow pudding, preparation of, 139, 159
Soap stools, 233
Sodium, sources of in food, 6
Soft-cooked eggs, 100
Soft custard, preparation of, 102
Soups, ash constituents of, 476
preparation of, 118
Soya manna muffins, preparation of, 148
Soya meal and bran muffins, preparation of, 157
Spanish cream, preparation of, 158
Spice cookies, preparation of, 152
Spinach, ash constituents of, 476
composition of, 494
fuel value of, 470, 494
nutrient value of, 470
vitamines in, 496
Spinach and egg salad, preparation of, 147
Spinach soup, preparation of, 152
Sponge pudding, preparation of, 109
Squab, composition of, 494
fuel value of, 494
Squab pie, preparation of, 151
Squash, ash constituents of, 476
composition of, 494
food content of, 481
fuel value of, 470, 494
nutrient value of, 470
standard portion of, 481
Standard broth, preparation of, 118
Standard portion of foods, 40, 478
Starch, excess of in food formulas, 236
Starchy desserts, preparation of, 108
Starvation, in treatment of diabetes, 372
Steaming, 70
Steapsin, 171
Sterilization, 84
Stewed tomatoes on toast, preparation of, 134
Stomach, and see Gastric
acid content of, determining, 248
arrangement of food in, 167
diseases of, predisposing factors in, 245
disturbance of motility and tone of, 246
disturbance of secretory processes in, 246
fermentation in, 180
passage of food from, 168
secretion of water in, 174
Strawberries, ash constituents of, 476
composition of, 494
food content of, 481
fuel value of, 470, 494
nutrient value of, 470
standard portion of, 481
Strawberry ice, preparation of, 137
Strawberry juice, composition of, 494
fuel value of, 494
String beans, and see Beans
preparation of, 129
Succotash, fuel value of, 470
nutrient value of, 470
Sucrase, 171
Suet, composition of, 494
fuel value of, 494
Sugar, adjusting of, in food formulas, 235
composition of, 494
fuel value of, 470, 494
in infant feeding, 207
in urine, in diabetes, 371
tests for, 328, 330,
331
nutrient value of, 470
Sugar-free milk, 162
Sugar-splitting enzymes, 171
Sulphur, sources of in food, 6
Sunflower seeds, vitamines in, 497
Sunshine cake, preparation of, 110
Sweetbreads, composition of, 494
fuel value of, 494
preparation of, 123
vitamines in, 496
Tallow, vitamines in, 498
Tamarind, ash constituents of, 476
Tapioca, ash constituents of, 477
composition of, 494
food content of, 482
[Pg 523]
fuel value of, 494
standard portion of, 482
Tapioca custard, preparation of, 109
Test meals, 250
Thermometry, 80
Thirst, in nephritis, 343
in typhoid fever, 299
Thymus, vitamines in, 496
Timothy, vitamines in, 498
Toast, composition of, 494
fuel value of, 494
preparation of, 105
Tomatoes, ash constituents of, 477
composition of, 494
food content of, 482
fuel value of, 470, 494
nutrient value of, 470
standard portion of, 482
vitamines in, 497
Tomato aspic, preparation of, 154
Tomato bisque, preparation of, 152
Tomato jelly, preparation of, 132
Tomato juice, ash constituents of, 477
Tomato salad, preparation of, 131, 132
Tomato stuffed with rice, preparation of, 133
Tonsillitis, dietetic treatment of, 309, 310
Toxins, elimination of, 323
Trout, composition of, 494
fuel value of, 494
Truffles, ash constituents of, 477
Tuberculosis, 301, 305
dietetic treatment in, 302
high calorie diet in, 304
reënforcing the diet in, 306
schedule of diets in, 307
Tuna, fuel value of, 470
nutrient value of, 470
Tuna fish salad, preparation of, 154
Turkey, composition of, 494
fuel value of, 470, 494
nutrient value of, 470
selection of, 114
Turnips, ash constituents of, 477
composition of, 494
food content of, 482
fuel value of, 470, 494
nutrient value of, 470
standard portion of, 482
Turnip tops, ash constituents of, 477
Typhoid fever, 288,
297
absorption of food in, 290, 297
acidosis in, 299
care of mouth in, 299
Coleman’s high calorie diet in, 289,
291, 294, 295,
298, 299
energy expenditures in, 288, 297
energy requirements in, 289, 297
essential points in dietary, 297
hemorrhage in, 296, 298
high calorie diet in, 289, 291,
294, 295, 298,
299
idiosyncrasies in, 300
increasing diet in, 290, 300
liquid diet in, 290, 293
milk diet in, 291, 298
Presbyterian Hospital diet list for, 292
rate of metabolism in, 297
reënforcing diet in, 300
semi-solid diet in, 293
soft diet in, 293
thirst in, 299
tympanites in, 290
varying diet in, 292
Under-dilution of infants’ foods, troubles due to, 232
Under-feeding in infants and children, 243
Urea and salt test, 351
Uremic poisoning, 361
Uric acid, 324
elimination of, 417
formation of, 184
source of, 417
Urinalysis, 323
Urine, acetone in, test for, 333
albumin in, tests for, 333
analysis of, 323, 324
collection of, 326, 334
diacetic acid in, test for, 332
diseases in which it is diminished, 326
effect of food upon, 326
examination of, 323, 324
in diabetes, 328, 329,
330, 371, 401,
402
indican in, test for, 334
preserving, 335
sugar in, tests for, 328, 329,
330, 331
Utensils, care of, 76
[Pg 524] Vanilla ice cream, preparation of, 91
Veal, 112, 114, and see
Meats
composition of, 494
cuts of, 117
food content of, 482
fuel value of, 470, 494
method of preparation, 117
nutrient value of, 470
standard portion of, 482
Veal bird, preparation of, 150
Veal broth, preparation of, 118
Veal cutlets, preparation of, 124
Vegetable oils, vitamines in, 498
Vegetable salads, preparation of, 131
Vegetable soups, fuel value of, 471
nutrient value of, 471
preparation of, 223
Vegetables, preparation of, 126, 128,
153
vitamines in, 496
Vinegar, ash constituents of, 477
Vitamines, 29
fat soluble A, 15
in foods, 496, 497,
498
functions of, 30, 31
in foods, 496, 497,
498
requirements of in body, 52
source of in foods, 6, 7
water soluble B, 31
in foods, 496, 497,
498
water soluble C, 33
in foods, 496, 497,
498
Walnuts, ash constituents of, 477
composition of, 494
food content of, 482
fuel value of, 471, 494
nutrient value of, 471
standard portion of, 482
vitamines in, 498
Water, 24
absorption of, 177
administration of to infants, 229
as a fat maker, 425
as a stimulant to gastric secretion, 253
excretion of, 324
factors determining amount needed, 25
function of, 24
sources of in foods, 5
Water soluble B, 31
effect of alkalies upon, 32
effect of heat upon, 32
functions of, 31
in foods, 6, 496,
497, 498
Water soluble C, 33
effect of heat upon, 33
in foods, 7, 496,
497, 498
Water-cress, ash constituents of, 477
Water ices, preparation of, 136
Watermelon, ash constituents of, 477
composition of, 494
food contents of, 482
fuel value of, 471, 494
nutrient value of, 471
standard portion of, 482
Weights and measures, 77
household, 78
metric, 77
Weights and heights of children, 49, 499, 500, 501
Wet nurses, 229
Wheat, ash constituents of, 477
composition of, 494
fuel value of, 471, 494
nutrient value of, 471
vitamines in, 497
Whey, 83
ash constituents of, 477
composition of, 494
fuel value of, 494
vitamines in, 498
Whey mixtures, 226
Whitefish, composition of, 494
fuel value of, 471, 494
nutrient value of, 471
Whortleberries, ash constituents of, 477
Widal’s diet in nephritis, 341
Wine, ash constituents of, 477
Wine jelly, preparation of, 136, 160, 161
Wine panada, preparation of, 105
Wine sauce, preparation of, 111
Work, influence of upon food requirements, 43
Yeast, vitamines in, 498
Zwieback, composition of, 494
fuel value of, 471, 494
nutrient value of, 471
Transcriber's Note
Minor punctuation errors have been repaired. Hyphenation and accent usage has been made consistent.
There are some errors in calculation in places; these have been preserved as printed. For example, addition errors in the table on pp. 377-8.
Variable spelling is preserved as printed (e.g. sirup and syrup).
12 M. has been used inconsistently, to indicate either 12 Midnight or 12 Midday. It has been preserved as printed in all cases.
Calorie count or separate ingredients lists are omitted from some recipes; these are left as printed.
The 'Eggs' section, starting on page 95, has no recipes included. However, the following 'Fruit Beverages' section has a large number of egg recipes included in it. Whether this was an error or intentional is unclear, so the sections and ordering of recipes have been preserved as they appeared in the original publication.
The recipe for Foamy Sauce appears twice, once each on page 111 and 112. There is no apparent difference apart from the calorie amount. Both versions have been left in place.
The recipe for Sauce for Puddings (page 112) appears identical to the recipe for Wine or Fruit Sauce (page 111), except for the recipe name and calorie amounts. Both versions have been left in place.
The table heading on page 117 refers to cuts of lamb and mutton, while the table itself refers to lamb and veal. This has been left as printed.
There are two instances of a recipe called Beef Juice, on pages 119 and 141. Both have been left in place as printed.
The following amendments have been made:
Page 30—Mellanbly amended to Mellanby—"Mellanby of England believes the “A” vitamine to be a factor ..."
Page 31—or amended to of—"Effect of Heat on the “A” Vitamine."
Page 77—the first reference to centigram has been amended from c. to cgm.
Page 80—in amended to is—"... that every Fahrenheit degree is 9/5 times as large ..."
Page 92—erroneous 'or' removed from second malted milk recipe (original called for either milk and water or salt).
Page 111—omitted word 'juice' added to ingredients list in Wine or Fruit Sauce recipe.
Page 125—omitted subheading for Fish added.
Page 128—repeated heading 'Vegetables and Fruits' removed.
Page 131—omitted 'or' added to dressing options in Tomato (No. 1) recipe.
Page 134—in the ingredients for French Dressing, paprika amended to salt, to follow the recipe.
Page 145—superfluous 'and' deleted between paragraph starting "½ cup raisins ..." and paragraph starting "Cream butter and sugar ..."
Page 146—chlorid amended to chloride—"1 dram sodium chloride (common salt)"
Page 146, footnote—Ellithorp amended to Ellithorpe—"Courtesy of Misses Foley and Ellithorpe, Dieticians."
Page 147—agar gar amended to agar-agar—"1 tsp. or 7 gms. agar-agar"
Page 156—superfluous 'grams' removed following calorie count in Casoid Flour and Bran Muffins recipe.
Page 156—omitted ', trace;' added to carbohydrate quantity for one muffin in the Casoid Flour and Bran Muffins recipe.
Page 157—omitted 'protein,' added to 2 grams quantity for one muffin in the Soya Meal and Bran Muffins recipe.
Page 172—dioxid amended to dioxide—"Those which produce carbon dioxide without the use ..."
Page 194—grapefuit amended to grapefruit—"... dates, figs, or grapefruit, stewed or raw."
Page 213—proced amended to proceed—"... we will proceed with the method itself."
Page 219—zweiback amended to zwieback—"... pieces of stale bread, toast or zwieback."
Page 241—Mellenby amended to Mellanby—"Mellanby of England claims that the oil owes its curative ..."
Page 244f—empysema amended to emphysema—"... broncho-pneumonia, acute emphysema and collapse of the lung ..."
Page 259—"Soft-cooked egg (1)" has been amended to "1 soft-cooked egg" in the 11 A.M. section of the Seventh Day diet, for consistency with other entries.
Page 272—omitted heading 'Breakfast' added.
Page 281—tonsilitis amended to tonsillitis—"... as accompany colds, tonsillitis, chicken pox ..."
Page 337—omitted 'of' added—"... the end-products of the nitrogenous foods ingested, ..."
Page 349—grams amended to c.c.—"Supper 5 P.M. ... 200 c.c. ..."
Page 385—Huntly amended to Huntley (Breakfast biscuit entry on table).
Page 407—bilous amended to bilious—"In certain individuals beer will induce a bilious attack."
Page 435—supportting amended to supporting—"... which have been deprived of the supporting fat."
Page 476—Sapato amended to Sapota (in table).
Page 481—Horlick amended to Horlick's (milk powder entry in table).
Page 519—The index entry for Organic acids originally followed Over-feeding of infants and children. It has been moved to the correct place.
Page 523—The index entry for Utensils originally followed Under-feeding in infants and children. It has been moved to the correct place.
Omitted page numbers were blank pages in the original.
Alphabetic links have been added to the index for ease of navigation.
End of Project Gutenberg's Dietetics for Nurses, by Fairfax T. Proudfit
*** END OF THIS PROJECT GUTENBERG EBOOK DIETETICS FOR NURSES ***
***** This file should be named 33379-h.htm or 33379-h.zip *****
This and all associated files of various formats will be found in:
http://www.gutenberg.org/3/3/3/7/33379/
Produced by Kevin Handy, John Hagerson, Sam W. and the
Online Distributed Proofreading Team at http://www.pgdp.net
Updated editions will replace the previous one--the old editions
will be renamed.
Creating the works from public domain print editions means that no
one owns a United States copyright in these works, so the Foundation
(and you!) can copy and distribute it in the United States without
permission and without paying copyright royalties. Special rules,
set forth in the General Terms of Use part of this license, apply to
copying and distributing Project Gutenberg-tm electronic works to
protect the PROJECT GUTENBERG-tm concept and trademark. Project
Gutenberg is a registered trademark, and may not be used if you
charge for the eBooks, unless you receive specific permission. If you
do not charge anything for copies of this eBook, complying with the
rules is very easy. You may use this eBook for nearly any purpose
such as creation of derivative works, reports, performances and
research. They may be modified and printed and given away--you may do
practically ANYTHING with public domain eBooks. Redistribution is
subject to the trademark license, especially commercial
redistribution.
*** START: FULL LICENSE ***
THE FULL PROJECT GUTENBERG LICENSE
PLEASE READ THIS BEFORE YOU DISTRIBUTE OR USE THIS WORK
To protect the Project Gutenberg-tm mission of promoting the free
distribution of electronic works, by using or distributing this work
(or any other work associated in any way with the phrase "Project
Gutenberg"), you agree to comply with all the terms of the Full Project
Gutenberg-tm License (available with this file or online at
http://gutenberg.org/license).
Section 1. General Terms of Use and Redistributing Project Gutenberg-tm
electronic works
1.A. By reading or using any part of this Project Gutenberg-tm
electronic work, you indicate that you have read, understand, agree to
and accept all the terms of this license and intellectual property
(trademark/copyright) agreement. If you do not agree to abide by all
the terms of this agreement, you must cease using and return or destroy
all copies of Project Gutenberg-tm electronic works in your possession.
If you paid a fee for obtaining a copy of or access to a Project
Gutenberg-tm electronic work and you do not agree to be bound by the
terms of this agreement, you may obtain a refund from the person or
entity to whom you paid the fee as set forth in paragraph 1.E.8.
1.B. "Project Gutenberg" is a registered trademark. It may only be
used on or associated in any way with an electronic work by people who
agree to be bound by the terms of this agreement. There are a few
things that you can do with most Project Gutenberg-tm electronic works
even without complying with the full terms of this agreement. See
paragraph 1.C below. There are a lot of things you can do with Project
Gutenberg-tm electronic works if you follow the terms of this agreement
and help preserve free future access to Project Gutenberg-tm electronic
works. See paragraph 1.E below.
1.C. The Project Gutenberg Literary Archive Foundation ("the Foundation"
or PGLAF), owns a compilation copyright in the collection of Project
Gutenberg-tm electronic works. Nearly all the individual works in the
collection are in the public domain in the United States. If an
individual work is in the public domain in the United States and you are
located in the United States, we do not claim a right to prevent you from
copying, distributing, performing, displaying or creating derivative
works based on the work as long as all references to Project Gutenberg
are removed. Of course, we hope that you will support the Project
Gutenberg-tm mission of promoting free access to electronic works by
freely sharing Project Gutenberg-tm works in compliance with the terms of
this agreement for keeping the Project Gutenberg-tm name associated with
the work. You can easily comply with the terms of this agreement by
keeping this work in the same format with its attached full Project
Gutenberg-tm License when you share it without charge with others.
1.D. The copyright laws of the place where you are located also govern
what you can do with this work. Copyright laws in most countries are in
a constant state of change. If you are outside the United States, check
the laws of your country in addition to the terms of this agreement
before downloading, copying, displaying, performing, distributing or
creating derivative works based on this work or any other Project
Gutenberg-tm work. The Foundation makes no representations concerning
the copyright status of any work in any country outside the United
States.
1.E. Unless you have removed all references to Project Gutenberg:
1.E.1. The following sentence, with active links to, or other immediate
access to, the full Project Gutenberg-tm License must appear prominently
whenever any copy of a Project Gutenberg-tm work (any work on which the
phrase "Project Gutenberg" appears, or with which the phrase "Project
Gutenberg" is associated) is accessed, displayed, performed, viewed,
copied or distributed:
This eBook is for the use of anyone anywhere at no cost and with
almost no restrictions whatsoever. You may copy it, give it away or
re-use it under the terms of the Project Gutenberg License included
with this eBook or online at www.gutenberg.org
1.E.2. If an individual Project Gutenberg-tm electronic work is derived
from the public domain (does not contain a notice indicating that it is
posted with permission of the copyright holder), the work can be copied
and distributed to anyone in the United States without paying any fees
or charges. If you are redistributing or providing access to a work
with the phrase "Project Gutenberg" associated with or appearing on the
work, you must comply either with the requirements of paragraphs 1.E.1
through 1.E.7 or obtain permission for the use of the work and the
Project Gutenberg-tm trademark as set forth in paragraphs 1.E.8 or
1.E.9.
1.E.3. If an individual Project Gutenberg-tm electronic work is posted
with the permission of the copyright holder, your use and distribution
must comply with both paragraphs 1.E.1 through 1.E.7 and any additional
terms imposed by the copyright holder. Additional terms will be linked
to the Project Gutenberg-tm License for all works posted with the
permission of the copyright holder found at the beginning of this work.
1.E.4. Do not unlink or detach or remove the full Project Gutenberg-tm
License terms from this work, or any files containing a part of this
work or any other work associated with Project Gutenberg-tm.
1.E.5. Do not copy, display, perform, distribute or redistribute this
electronic work, or any part of this electronic work, without
prominently displaying the sentence set forth in paragraph 1.E.1 with
active links or immediate access to the full terms of the Project
Gutenberg-tm License.
1.E.6. You may convert to and distribute this work in any binary,
compressed, marked up, nonproprietary or proprietary form, including any
word processing or hypertext form. However, if you provide access to or
distribute copies of a Project Gutenberg-tm work in a format other than
"Plain Vanilla ASCII" or other format used in the official version
posted on the official Project Gutenberg-tm web site (www.gutenberg.org),
you must, at no additional cost, fee or expense to the user, provide a
copy, a means of exporting a copy, or a means of obtaining a copy upon
request, of the work in its original "Plain Vanilla ASCII" or other
form. Any alternate format must include the full Project Gutenberg-tm
License as specified in paragraph 1.E.1.
1.E.7. Do not charge a fee for access to, viewing, displaying,
performing, copying or distributing any Project Gutenberg-tm works
unless you comply with paragraph 1.E.8 or 1.E.9.
1.E.8. You may charge a reasonable fee for copies of or providing
access to or distributing Project Gutenberg-tm electronic works provided
that
- You pay a royalty fee of 20% of the gross profits you derive from
the use of Project Gutenberg-tm works calculated using the method
you already use to calculate your applicable taxes. The fee is
owed to the owner of the Project Gutenberg-tm trademark, but he
has agreed to donate royalties under this paragraph to the
Project Gutenberg Literary Archive Foundation. Royalty payments
must be paid within 60 days following each date on which you
prepare (or are legally required to prepare) your periodic tax
returns. Royalty payments should be clearly marked as such and
sent to the Project Gutenberg Literary Archive Foundation at the
address specified in Section 4, "Information about donations to
the Project Gutenberg Literary Archive Foundation."
- You provide a full refund of any money paid by a user who notifies
you in writing (or by e-mail) within 30 days of receipt that s/he
does not agree to the terms of the full Project Gutenberg-tm
License. You must require such a user to return or
destroy all copies of the works possessed in a physical medium
and discontinue all use of and all access to other copies of
Project Gutenberg-tm works.
- You provide, in accordance with paragraph 1.F.3, a full refund of any
money paid for a work or a replacement copy, if a defect in the
electronic work is discovered and reported to you within 90 days
of receipt of the work.
- You comply with all other terms of this agreement for free
distribution of Project Gutenberg-tm works.
1.E.9. If you wish to charge a fee or distribute a Project Gutenberg-tm
electronic work or group of works on different terms than are set
forth in this agreement, you must obtain permission in writing from
both the Project Gutenberg Literary Archive Foundation and Michael
Hart, the owner of the Project Gutenberg-tm trademark. Contact the
Foundation as set forth in Section 3 below.
1.F.
1.F.1. Project Gutenberg volunteers and employees expend considerable
effort to identify, do copyright research on, transcribe and proofread
public domain works in creating the Project Gutenberg-tm
collection. Despite these efforts, Project Gutenberg-tm electronic
works, and the medium on which they may be stored, may contain
"Defects," such as, but not limited to, incomplete, inaccurate or
corrupt data, transcription errors, a copyright or other intellectual
property infringement, a defective or damaged disk or other medium, a
computer virus, or computer codes that damage or cannot be read by
your equipment.
1.F.2. LIMITED WARRANTY, DISCLAIMER OF DAMAGES - Except for the "Right
of Replacement or Refund" described in paragraph 1.F.3, the Project
Gutenberg Literary Archive Foundation, the owner of the Project
Gutenberg-tm trademark, and any other party distributing a Project
Gutenberg-tm electronic work under this agreement, disclaim all
liability to you for damages, costs and expenses, including legal
fees. YOU AGREE THAT YOU HAVE NO REMEDIES FOR NEGLIGENCE, STRICT
LIABILITY, BREACH OF WARRANTY OR BREACH OF CONTRACT EXCEPT THOSE
PROVIDED IN PARAGRAPH F3. YOU AGREE THAT THE FOUNDATION, THE
TRADEMARK OWNER, AND ANY DISTRIBUTOR UNDER THIS AGREEMENT WILL NOT BE
LIABLE TO YOU FOR ACTUAL, DIRECT, INDIRECT, CONSEQUENTIAL, PUNITIVE OR
INCIDENTAL DAMAGES EVEN IF YOU GIVE NOTICE OF THE POSSIBILITY OF SUCH
DAMAGE.
1.F.3. LIMITED RIGHT OF REPLACEMENT OR REFUND - If you discover a
defect in this electronic work within 90 days of receiving it, you can
receive a refund of the money (if any) you paid for it by sending a
written explanation to the person you received the work from. If you
received the work on a physical medium, you must return the medium with
your written explanation. The person or entity that provided you with
the defective work may elect to provide a replacement copy in lieu of a
refund. If you received the work electronically, the person or entity
providing it to you may choose to give you a second opportunity to
receive the work electronically in lieu of a refund. If the second copy
is also defective, you may demand a refund in writing without further
opportunities to fix the problem.
1.F.4. Except for the limited right of replacement or refund set forth
in paragraph 1.F.3, this work is provided to you 'AS-IS' WITH NO OTHER
WARRANTIES OF ANY KIND, EXPRESS OR IMPLIED, INCLUDING BUT NOT LIMITED TO
WARRANTIES OF MERCHANTIBILITY OR FITNESS FOR ANY PURPOSE.
1.F.5. Some states do not allow disclaimers of certain implied
warranties or the exclusion or limitation of certain types of damages.
If any disclaimer or limitation set forth in this agreement violates the
law of the state applicable to this agreement, the agreement shall be
interpreted to make the maximum disclaimer or limitation permitted by
the applicable state law. The invalidity or unenforceability of any
provision of this agreement shall not void the remaining provisions.
1.F.6. INDEMNITY - You agree to indemnify and hold the Foundation, the
trademark owner, any agent or employee of the Foundation, anyone
providing copies of Project Gutenberg-tm electronic works in accordance
with this agreement, and any volunteers associated with the production,
promotion and distribution of Project Gutenberg-tm electronic works,
harmless from all liability, costs and expenses, including legal fees,
that arise directly or indirectly from any of the following which you do
or cause to occur: (a) distribution of this or any Project Gutenberg-tm
work, (b) alteration, modification, or additions or deletions to any
Project Gutenberg-tm work, and (c) any Defect you cause.
Section 2. Information about the Mission of Project Gutenberg-tm
Project Gutenberg-tm is synonymous with the free distribution of
electronic works in formats readable by the widest variety of computers
including obsolete, old, middle-aged and new computers. It exists
because of the efforts of hundreds of volunteers and donations from
people in all walks of life.
Volunteers and financial support to provide volunteers with the
assistance they need, are critical to reaching Project Gutenberg-tm's
goals and ensuring that the Project Gutenberg-tm collection will
remain freely available for generations to come. In 2001, the Project
Gutenberg Literary Archive Foundation was created to provide a secure
and permanent future for Project Gutenberg-tm and future generations.
To learn more about the Project Gutenberg Literary Archive Foundation
and how your efforts and donations can help, see Sections 3 and 4
and the Foundation web page at http://www.pglaf.org.
Section 3. Information about the Project Gutenberg Literary Archive
Foundation
The Project Gutenberg Literary Archive Foundation is a non profit
501(c)(3) educational corporation organized under the laws of the
state of Mississippi and granted tax exempt status by the Internal
Revenue Service. The Foundation's EIN or federal tax identification
number is 64-6221541. Its 501(c)(3) letter is posted at
http://pglaf.org/fundraising. Contributions to the Project Gutenberg
Literary Archive Foundation are tax deductible to the full extent
permitted by U.S. federal laws and your state's laws.
The Foundation's principal office is located at 4557 Melan Dr. S.
Fairbanks, AK, 99712., but its volunteers and employees are scattered
throughout numerous locations. Its business office is located at
809 North 1500 West, Salt Lake City, UT 84116, (801) 596-1887, email
business@pglaf.org. Email contact links and up to date contact
information can be found at the Foundation's web site and official
page at http://pglaf.org
For additional contact information:
Dr. Gregory B. Newby
Chief Executive and Director
gbnewby@pglaf.org
Section 4. Information about Donations to the Project Gutenberg
Literary Archive Foundation
Project Gutenberg-tm depends upon and cannot survive without wide
spread public support and donations to carry out its mission of
increasing the number of public domain and licensed works that can be
freely distributed in machine readable form accessible by the widest
array of equipment including outdated equipment. Many small donations
($1 to $5,000) are particularly important to maintaining tax exempt
status with the IRS.
The Foundation is committed to complying with the laws regulating
charities and charitable donations in all 50 states of the United
States. Compliance requirements are not uniform and it takes a
considerable effort, much paperwork and many fees to meet and keep up
with these requirements. We do not solicit donations in locations
where we have not received written confirmation of compliance. To
SEND DONATIONS or determine the status of compliance for any
particular state visit http://pglaf.org
While we cannot and do not solicit contributions from states where we
have not met the solicitation requirements, we know of no prohibition
against accepting unsolicited donations from donors in such states who
approach us with offers to donate.
International donations are gratefully accepted, but we cannot make
any statements concerning tax treatment of donations received from
outside the United States. U.S. laws alone swamp our small staff.
Please check the Project Gutenberg Web pages for current donation
methods and addresses. Donations are accepted in a number of other
ways including checks, online payments and credit card donations.
To donate, please visit: http://pglaf.org/donate
Section 5. General Information About Project Gutenberg-tm electronic
works.
Professor Michael S. Hart is the originator of the Project Gutenberg-tm
concept of a library of electronic works that could be freely shared
with anyone. For thirty years, he produced and distributed Project
Gutenberg-tm eBooks with only a loose network of volunteer support.
Project Gutenberg-tm eBooks are often created from several printed
editions, all of which are confirmed as Public Domain in the U.S.
unless a copyright notice is included. Thus, we do not necessarily
keep eBooks in compliance with any particular paper edition.
Most people start at our Web site which has the main PG search facility:
http://www.gutenberg.org
This Web site includes information about Project Gutenberg-tm,
including how to make donations to the Project Gutenberg Literary
Archive Foundation, how to help produce our new eBooks, and how to
subscribe to our email newsletter to hear about new eBooks.